Combined Cataract Extraction and Vitrectomy for Macula-sparing Retinal Detachment: Visual Outcomes and Complications
Article information
Abstract
Purpose
To evaluate the visual outcome of combined phacoemulsification, intraocular lens implantation, and vitrectomy for macula-sparing rhegmatogenous retinal detachment.
Methods
The results of combined vitrectomy with cataract extraction were retrospectively analyzed in patients with preexisting cataracts and new-onset rhegmatogenous retinal detachment. To qualify, patients must also have had macular sparing in a region 6,000 µm in diameter on optical coherence tomography. The anatomical success rate, visual outcomes, and postoperative complications relating to visual acuity were evaluated.
Results
In 56 patients followed postoperatively for more than 12 months, the initial and final surgical success rate was 96.4% and 100%, respectively. The mean preoperative logarithm of the minimum angle of resolution visual acuity was 0.05 and decreased to 0.11 postoperatively (p < 0.001). Of the 56 patients, 20 (35.7%) had worse visual acuity postoperatively, compared with preoperatively (0.06 vs. 0.27, p < 0.001); these cases were comprised of six patients with epiretinal membranes, 12 patients with a posterior capsule opacity, and two patients with cystoid macular edema. In the remaining 36 patients, there were no significant differences in visual acuity preoperatively and postoperatively (0.04 vs. 0.03, p = 0.324).
Conclusions
In patients with cataracts who develop macula-sparing rhegmatogenous retinal detachment and whose visual prognosis is excellent assuming the retina can be reattached successfully, combined phacoemulsification, intraocular lens implantation, and vitrectomy might be an effective treatment. However, the visual prognosis is significantly affected by postoperative complications such as an epiretinal membranes, posterior capsule opacity, and cystoid macular edema. Therefore, further studies should examine methods to prevent these postoperative complications.
With the introduction of scleral buckling [1], pneumatic retinopexy [2,3], and vitrectomy [4] for treating rhegmatogenous retinal detachment, remarkable advances have been made in recent years [5]. Using these methods, the anatomical success rate in the treatment of rhegmatogenous retinal detachment exceeds 90% [6,7,8]. In particular, pars plana vitrectomy has undergone several advancements in recent years compared to scleral buckling for the selective treatment of rhegmatogenous retinal detachment, although their reported surgical success rates are equivalent [9]. Despite the high rate of anatomical success, the prognosis for visual acuity is relatively poor. Despite a surgical success rate of 97%, the mean postoperative visual acuity was 20/50 according to a recent prospective study [7].
Many factors affect postoperative visual acuity [10]. The most crucial prognostic factors include the preoperative visual acuity [11,12,13], and the presence and duration [14] of macular detachment. When rhegmatogenous retinal detachment involves areas adjacent to the macula larger than a diameter of 6,000 µm, the presence of macular detachment cannot be evaluated precisely using a conventional fundus exam, particularly with shallow retinal detachment. Optical coherence tomography (OCT), a novel imaging diagnostic modality, provides high-resolution cross-sectional images of the macular region, which accurately assess the preoperative presence of macular detachment.
Given this background, the anatomical success rate and visual outcomes were examined following pars plana vitrectomy, phacoemulsification, and intraocular lens (IOL) implantation for rhegmatogenous retinal detachment in patients with cataracts who had no macular detachment within a 6,000-µm-diameter on preoperative OCT. Complications that affect postoperative visual acuity were also assessed.
Materials and Methods
This study was a retrospective analysis of the medical records of patients who were treated surgically for rhegmatogenous retinal detachment in the department of ophthalmology of the Chungnam University Hospital between May 2006 and June 2009. Approval by the institutional review board of the Chungnam National University Hospital was obtained for this retrospective study. Patients were enrolled if they had rhegmatogenous retinal detachment and preexisting cataracts with a 6,000-µm-diameter area of macular sparing on preoperative OCT for which they underwent combined pars plana vitrectomy, phacoemulsification, and IOL implantation.
Patients whose retinal detachment involved the area of the macula within a 6,000-µm-diameter area were excluded from the analysis, as were patients who underwent concomitant scleral buckling. Also excluded were those having pseudophakia, a history of intraocular surgery or ocular trauma, or patients who were followed for less than 12 months postoperatively.
All of the surgical procedures were performed by a single surgeon (KJY) under general or local anesthesia. Following a peritomy, three 20-gauge sclerotomies were created in the pars plana of the ciliary body 4.0 mm from the corneal limbus. Surgery was performed using a vitrectomy machine (Accurus Surgical System; Alcon Laboratories, Fort Worth, TX, USA). A wide-field visualization system (Mini Quad XL; Volk Optical, Mentor, OH, USA) was used. If there was no posterior vitreous detachment, as verified with intravitreal triamcinolone injection, posterior vitreous detachment was induced using a vitreous cutter, intraocular forceps, and pick. In an attempt to reduce traction on the peripheral retina, posterior vitreous detachment was induced only to the posterior pole, and the rest of the vitreous was removed using a vitreous cutter with a high cutting rate. As much of the peripheral vitreous as possible was removed by performing scleral depression on the area over the entire 360 degrees. Simultaneously, the traction in the area adjacent to the retinal break was removed. Following fluid-air exchange, perfluorocarbon liquid was infused until it filled the area posterior to the retinal break. In a preexisting retinal break, intraocular-subretinal f luid drainage was performed using a backflush tip. Following removal of the perfluorocarbon liquid, intraocular laser retinopexy was done for the areas adjacent to the retinal break. The cataract was extracted concomitantly. Before the vitrectomy, phacoemulsification was carried out through a 2.8-mm clear cornea incision. Following the vitrectomy and fluid-air exchange, posterior chamber IOL implantation was performed. Following air-gas exchange with SF6 or C3F8, the sclerotomy was sutured.
Preoperative and postoperative best-corrected visual acuity (BCVA), occurrence and treatment of postoperative complications, and time of complication treatment were evaluated through a retrospective analysis of the medical records. Patient's age and sex, intraocular pressure, slit lamp microscopic examination, fundoscopy, and preoperative and postoperative OCT were also reviewed. Based on the comparison of the BCVA preoperatively and postoperatively, patients who had a significant decrease in visual acuity were assigned to group A, and the remaining patients were assigned to group B. The visual acuity was measured using a Snellen chart, and the results were converted to logarithm of the minimum angle of resolution (logMAR) for statistical analysis. A significant decrease in the visual acuity was defined as when the BCVA decreased postoperatively by more than 0.1 logMAR. In patients who developed complications reducing the postoperative BCVA, the postoperative BCVA was measured immediately before any surgical treatment. In patients who underwent epiretinal membrane (ERM) removal, the visual acuity measured the day before surgery was selected as the postoperative BCVA, and in patients who underwent posterior capsulotomy, the visual acuity measured before the posterior capsulotomy was selected as the postoperative BCVA.
In patients who had no complications or whose complications were not treated surgically, the visual acuity measured 12 months postoperatively was used as the postoperative BCVA. Statistical analysis was performed using a paired t-test. A value of p < 0.05 was considered statistically significant.
Results
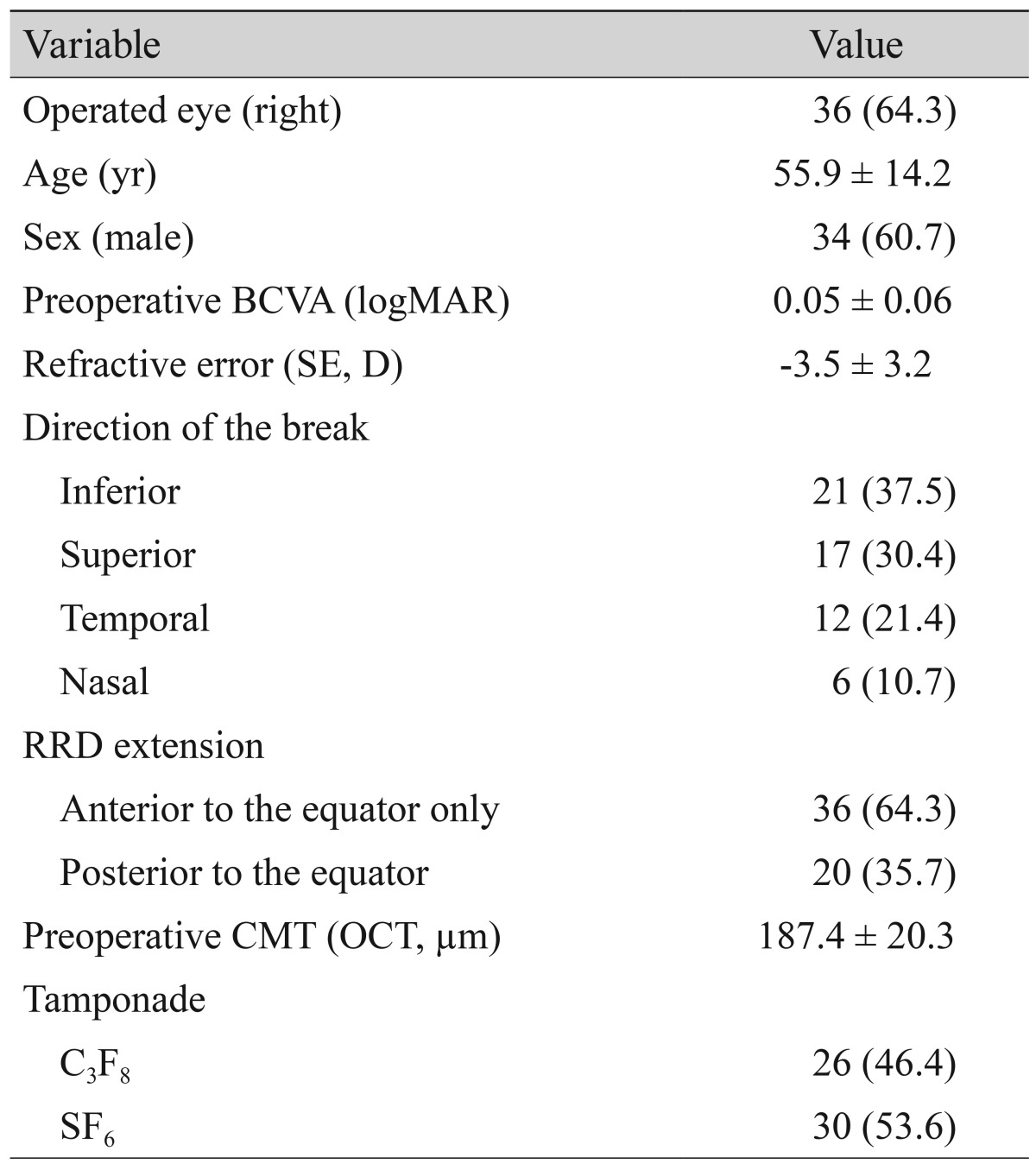
Of the patients who underwent vitrectomy and cataract surgery for macula sparing retinal detachment, 56 patients were analyzed who were followed for more than 12 months. Their mean age was 55.9 ± 14.2 years and 60.7% were male (Table 1). The grade of nuclear sclerosis or cortical opacity was between 1 and 2 according to the cataract grading system, Lens Opacity Classification III.
The rate of anatomical success of the primary surgery was 96.4% (54 / 56). In two patients who had recurrent retinal detachment, the retinal detachment was localized to a new break and did not involve the macular area. These two patients underwent secondary surgery and neither had further retinal detachment. Accordingly, the final surgical success rate was 100% (56 / 56).
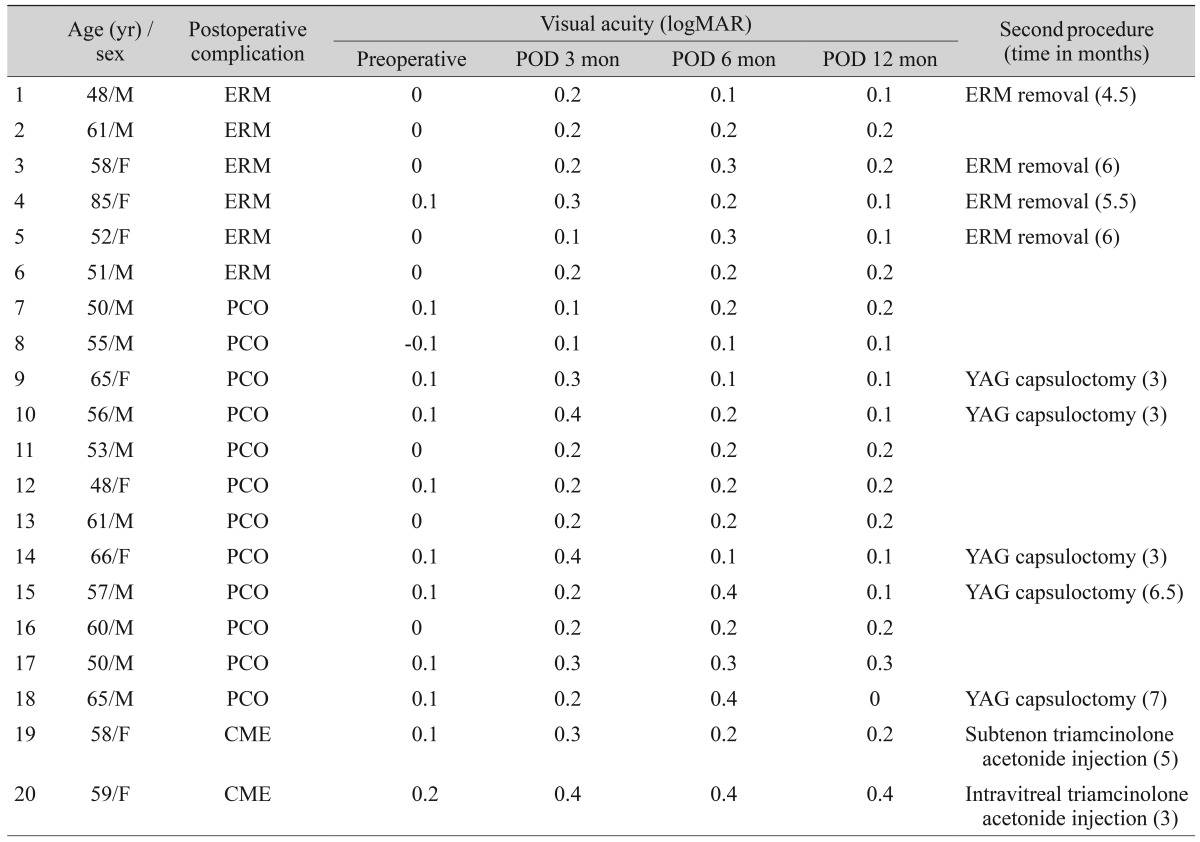
Of the 56 patients, 20 had a significant decrease in visual acuity following the surgery. These patients were classified in group A. The 36 patients who had a decrease in visual acuity of less than 0.1 logMAR or maintained or improved their visual acuity were classified in group B. In group A (n = 20), the mean age was 57.9 ± 8.5 years and 60.0% were male. In group B (n = 36), the mean age was 54.8 ± 14.9 years and 61.1% were male. The mean age and proportion of males did not differ significantly between the two groups ( p = 0.67 and 0.87, respectively). In group A, the causes of decreased visual acuity included six cases of an ERM, 12 cases of a posterior capsule opacity (PCO), and two cases of cystoid macular edema (CME). In these patients, the complications causing the decreased visual acuity were treated after obtaining written, informed consent.
Six patients were diagnosed with an ERM after primary surgery for rhegmatogenous retinal detachment using spectral domain OCT. ERM removal was recommended to four patients who presented with symptoms of metamorphopsia. They underwent ERM removal 4.5 to 6 months following the primary surgery. The vitrectomy was performed by the same surgeon (KJY). After removal of the ERM, the internal limiting membrane was stained with 0.5% indocyanine green (Dianogreen; Daiichi Pharmaceutical Co, Tokyo, Japan) for 20 to 30 seconds in a fluid filled eye while the infusion was stopped. After washing out the indocyanine green, the internal membrane was peeled off using microforceps. Two other patients also presented with more than 2 decimal lines of decreased visual acuity, but they opted out of further surgery and were only observed.
Of the 12 patients with PCO, five underwent neodymium-YAG (Nd-YAG) laser posterior capsulotomy 3 to 7 months after the primary surgery (Table 2). The decision to perform Nd-YAG laser posterior capsulotomy was based on slit-lamp findings with evidence of PCO at the center of the posterior capsule and symptoms of blurred vision with loss of 2 or more decimal lines of visual acuity. However, patients were again just observed if they opted out of further treatment.
Of the two patients with CME, each patient underwent subtenon or intravitreal triamcinolone acetonide (Tamceton; Hanall Biopharma, Seoul, Korea) injection 3 to 5 months after the primary surgery. All injections were administered in the supine position as an outpatient procedure. For subtenon injection, 40 mg/1.0 mL of triamcinolone acetonide was given, and for the intravitreal injection, 4 mg/0.1mL of triamcinolone acetonide was given at the superotemporal quadrant of the eye.
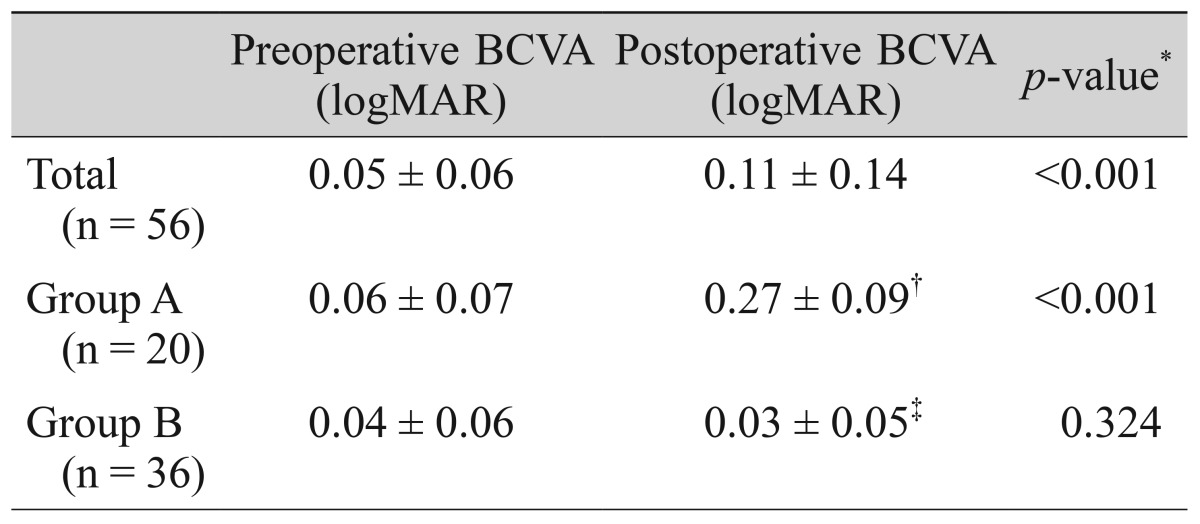
In the 56 patients, on average the BCVA decreased from 0.05 ± 0.06 preoperatively to 0.11 ± 0.14 postoperatively (p < 0.001). In group A, the postoperative visual acuity decreased significantly from 0.06 ± 0.07 preoperatively to 0.27 ± 0.09 (p < 0.001). In group B, the postoperative visual acuity improved from 0.04 ± 0.06 preoperatively to 0.03 ± 0.05, but the difference was not significant. The preoperative BCVA did not differ significantly between groups A and B (0.06 ± 0.07 vs. 0.04 ± 0.06; p = 0.64) (Table 3).
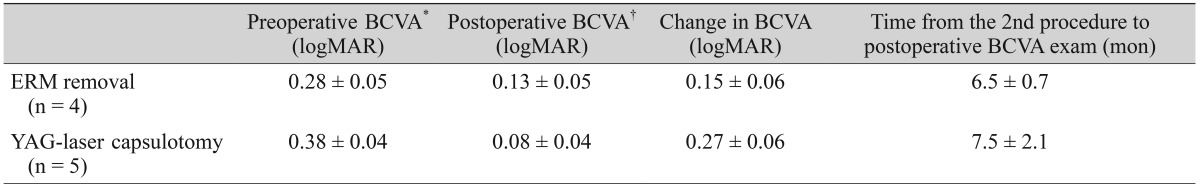
In the four patients who underwent ERM removal, the visual acuity improved by a mean of 0.15 ± 0.06 logMAR. In the five patients who underwent posterior capsulotomy, the visual acuity improved by a mean of 0.27 ± 0.06 logMAR. Of the four patients who underwent ERM removal, one recovered visual acuity to the level before surgery for retinal detachment. In the remaining three patients, however, the visual acuity decreased even after removal of the ERM compared to before the primary surgery. In all five patients who underwent posterior capsulotomy, the BCVA recovered to the level before the surgery for retinal detachment (Table 4).
Discussion
For the past several decades scleral buckling has been the standard surgical treatment for patients with retinal detachment [1]. However, complications of this procedure include migration, exposure, infection of the scleral bucking material, ischemia in the anterior ocular region, changes in the postoperative refractive index, and abnormal ocular movement. There are also some limitations in the clinical usefulness of scleral buckling in cases with proliferative vitreoretinopathy, a posterior retinal break, a giant retinal tear, or medium opacity.
Many studies have reported that vitrectomy has a higher rate of surgical success than scleral buckling [7,9]. Since it avoids the complications following scleral buckling, it has become a standard treatment for various vitreous retinal diseases [15]. Nevertheless, vitrectomy also has complications. The most common is the occurrence or progression of a cataract, particularly when the vitrectomy is performed for phakic eyes [16]. The incidence of cataract progression is as high as 79% following vitrectomy [17,18,19]. There is a higher chance of aggravating a cataract postoperatively, particularly in cases in which the cataract was present before the vitrectomy [17]. Accordingly, in patients with vitreoretinopathy who also have a cataract, vitrectomy combined with phacoemulsification and IOL implantation is preferentially performed [20,21,22]. In the present study combined surgery was also performed in patients with retinal detachment who had concurrent mild-to-moderate cataracts. As a result, cataracts could be prevented from impairing the postoperative visual acuity.
The presence [6] and duration [14] of macular detachment are key prognostic factors, together with the preoperative visual acuity [11,12,13]. However, the macular status can also be a confounding factor when analyzing visual prognosis because the conventional fundus exam has poor sensitivity for the detection of macular detachment, particularly in cases of shallow retinal detachment. Since patients with macular detachment on preoperative OCT were excluded, it was not possible to rule out the effect of preoperative macular detachment, one of the key factors causing a postoperative decrease in visual acuity. In the present series, the mean preoperative visual acuity was good, ranging from -0.1 to 0.2 logMAR. In patients with rhegmatogenous retinal detachment enrolled in this study, no comorbid intraocular disease other than cataracts were present. Therefore, it can be inferred that the cataract was resolved following combined surgery, which improved the BCVA. Despite prophylactic cataract removal, the average visual acuity for the entire patient group decreased significantly following surgery. Accordingly, the patients were subdivided into groups based on the postoperative change in visual acuity. In group B, which had no complications (n = 36), the postoperative visual acuity improved due to removal of the concurrent cataract, although the difference was not significant. This might have been both because the initial preoperative visual acuity was good, ranging from -0.1 to 0.2, and because too few patients were enrolled to determine whether the result was statistically significant. Of the 56 patients, 20 (35.7%) had decreased visual acuity postoperatively (group A). In these patients, the postoperative complications associated with decreased visual acuity included ERMs, posterior capsular opacity, and CME.
An ERM is a primary disease, but it may also occur secondarily to various other intraocular diseases or intraocular surgery. It can be asymptomatic, but it may also reduce visual acuity and cause metamorphopsia [23]. There have been many previous reports on the complications of combined cataract extraction and vitrectomy compared to sequential vitrectomy and cataract extraction. However, ERMs have not been associated with cataract extraction [24]. Previous studies have reported an incidence of 6.1% to 20.5% following surgery for rhegmatogenous retinal detachment [25,26]. In the present study, six patients (10.7%) who developed ERM presented with multiple and larger breaks compared to others, which is similar to previous results reporting a high incidence of ERMs in relation to the number and size of the retinal break [25]. Also, ERMs are diagnosed based on findings of spectral domain OCT, which make the diagnosis more precise and accurate and increase the detection rate of ERMs.
A posterior capsular opacity is one of the most common complications following cataract surgery [27]. Compared to cases undergoing cataract surgery only, the incidence of this complication is higher when cataract surgery is performed concomitantly with vitrectomy. Toda et al. [28] reported an incidence of 4.2% in patients undergoing cataract surgery only versus 10.3% when a vitrectomy was performed concomitantly. Wensheng et al. [24] reported that PCO was one of the most common complications following combined surgery and noted it in 21.5% of their cases.
CME may also occur in association with various ocular diseases, intraocular surgery, or intraocular laser treatment with a reported incidence following combined surgery of 8.1% to 9% [21,24]. In the present study an ERM developed in 11% (6 / 56) of cases, a posterior capsular opacity developed in 21% (12 / 56) of cases, and CME developed in 3.6% (2 / 56) of cases following combined surgery. These results concur with previous reports.
In the present series, four patients who underwent ERM removal and five patients who underwent posterior capsulotomy had improved visual acuity. In particular, one of the four patients who underwent ERM removal and all five patients who underwent posterior capsulotomy regained a postoperative visual acuity equal to their preoperative acuity after combined surgery for rhegmatogenous retinal detachment. In the remaining three ERM patients, however, the visual acuity decreased following removal of the ERM compared to before the primary surgery. With an ERM following rhegmatogenous retinal detachment, the visual acuity has been shown previously to improve following removal of the ERM [29-31]. However, when compared with an idiopathic ERM, a poor postoperative prognosis for visual acuity has been reported in ERM following rhegmatogenous retinal detachment [29].
The main advantage of the present study was that only patients with macula-sparing retinal detachment confirmed by preoperative OCT were enrolled. Therefore, the effects of postoperative complications in combined pars plana vitrectomy, phacoemulsification, and IOL implantation for rhegmatogenous retinal detachment could be analyzed independently of macular detachment.
This study has some limitations. First, the combined surgery was performed on patients with macular-on retinal detachment who had a cataract. Accordingly, limitations exist in confirming the effects of a single vitrectomy in patients with macula-sparing retinal detachment. To verify this finding, one must evaluate the effects of vitrectomy in patients with pseudophakic retinal detachment in whom the macula is attached. Second, this study had a retrospective design and the data could differ from results that might be obtained with more recent surgical techniques incorporating the use of small gauge (23 to 25 G) needles for vitrectomy [32]. Current small gauge vitrectomy systems provide the retinal surgeons not only a small gauge entry system but also more advanced surgical options such as a high cutting rate, efficient suction, and several surgical modes for more safe and effective surgery than before. Therefore, further studies using a smaller gauge system are needed. Third, due to the limited number of patients with macular-on rhegmatogenous retinal detachment who concurrently had a cataract, the number of patients enrolled was relatively small. Further large-scale prospective studies are needed.
In conclusion, in patients with rhegmatogenous retinal detachment whose macular region has not detached, combined vitrectomy, phacoemulsification, and IOL implantation may be an effective treatment method. When postoperative complications such as an ERM, a posterior capsular opacity, or CME occur, the postoperative visual acuity may worsen. Further studies should examine methods for preventing these postoperative complications.
Acknowledgements
This study was financially supported by research fund of Chungnam National University in 2010.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.