Case of Bilateral Retinal Neovascularization Associated with Chronic Idiopathic Myelofibrosis
Article information
Abstract
We report a case of bilateral peripheral retinal neovascularization and chronic idiopathic myelofibrosis in a 69-year-old man. Ophthalmic examination revealed peripheral retinal nonperfusion with retinal neovascularization in both eyes and vitreous hemorrhage in the right eye. Fluorescein angiography of both eyes showed a marked midperipheral and peripheral avascular retina temporally with arteriovenous anastomosis and sea-fan neovascularizations. Blood tests showed pancytopenia and teardrop-shaped red blood cells, and bone marrow examination showed hypocellular marrow with severe fibrosis. The neovascularization was regressed following pars plana vitrectomy in the right eye and scatter laser photocoagulation in the left. The results suggest that peripheral retinal vessel occlusion and neovascularization may be associated with idiopathic myelofibrosis.
Chronic idiopathic myelofibrosis (CIMF) is a clonal hematopoietic stem cell disorder characterized by increased bone marrow collagen fibrosis, leukoerythroblastic anemia with teardrop-shaped red cells, splenomegaly, and extramedullary hematopoiesis [1]. Retinal hemorrhage results from inefficient blood cell production, and blood cell irregularities have been reported in its association [2]. However, a MEDLINE search did not reveal any previous reports of retinal neovascularization in CIMF. We report one case of bilateral retinal neovascularization with CIMF.
Case Report
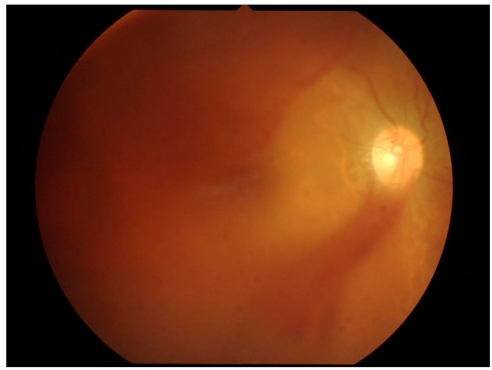
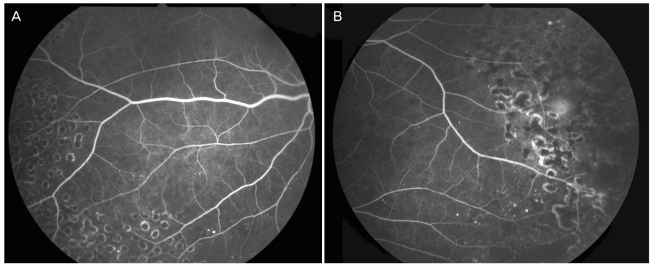
A 69-year-old man was referred to our clinic in August, 2006 presenting with decreased visual acuity in his right eye. He had been diagnosed with CIMF in July, 2000 and continued to have supportive care for CIMF throughout his follow-up. He had no specific ocular history and no history of irradiation. Visual acuities were 20/25 in the right eye and 20/20 in the left. Slit lamp examination showed no abnormalities on the conjunctiva, cornea, anterior chamber and iris. Fundus examination disclosed a mild vitreous hemorrhage in the right eye (Fig. 1). The peripheral fundi of both eyes showed marked vessel occlusion and microaneurysms in the temporal area. Fluorescein angiography in both eyes showed arteriovenous anastomosis with a marked area of nonperfusion and multiple sea-fan neovascularization on both eyes (Fig. 2). On laboratory examination, hemoglobin was 4.9 g/dL, platelet count was 63,000/mm3, and white blood cell count was 2,500/mm3 (with no blast cells). A peripheral blood smear test showed teardrop-shaped red cells. His fasting blood sugar value was normal, and the hemoglobin electrophoresis study was negative. Bone marrow examination showed hypocellular marrow with severe fibrosis and osteosclerosis (cellularity 11-20%), and no Philadelphia chromosome or BCR/ABL gene rearrangement was found.
(A) Fluorescein angiography of the right eye showing a peripheral arterial occlusion and multiple microaneurysms with sea-fans. (B) Fluorescein angiography of the left eye showing a peripheral arterial occlusion, a veno-arterial shunt vessel and neovascularization.
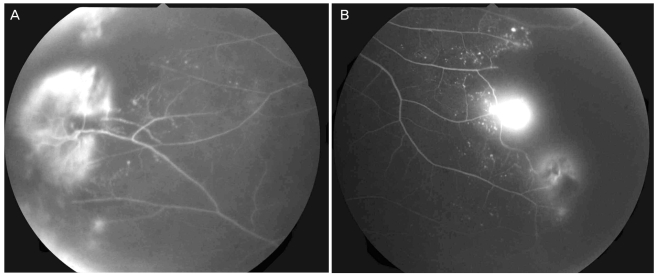
In view of these findings, photocoagulation of the peripheral avascular retina of the left eye and laser photocoagulation with pars plana vitrectomy of the right eye were performed. Intraoperative findings were mild vitreous hemorrhage with a diffuse traction membrane around the temporal avascular retina. The vitreous hemorrhage and traction membrane were removed and laser photocoagulation was performed. Four weeks after surgery, his visual acuities were 20/25 in the right eye and 20/20 in the left, fundus examination of the right eye revealed no vitreous hemorrhage, and the retinal neovascularization had regressed in both eyes with good laser scars (Fig. 3).
Discussion
Retinal ischemia and neovascularization have been described in relapsed chronic myeloid leukemia with increased blood viscosity caused by the marked leukocytosis or thrombocytosis [3-5]. The case described here may be unique because the patient's white blood cell and platelet count were decreased below the normal range, and it is unlikely, in our opinion, that a bleeding tendency due to thrombocytopenia induced the vitreous hemorrhage because no indications of leukemic retinopathy, such as intraretinal hemorrhage or cotton-wool exudates, were found. In our case, the fundus and fluorescein angiography findings were very similar to those of sickle retinopathy in which dense, sickled erythrocytes implicate retinal vaso-occlusions in the small caliber vessels. However, sickle cell disease is extremely rare in far-east Asians, and there was no other evidence of sickle cell disease in our case. We speculate that the red blood cells with abnormal morphologies in our CIMF patient occluded the peripheral microvasculature, eventually leading to peripheral retinal neovascularization. It has been reported that many patients with CIMF have remarkable histories of thromboembolic episodes and hemorrhage [6]. Also, neoangiogenesis is known to be an important feature of CIMF due to increased levels of angiogenic cytokines such as b-fibroblastic growth factor and vascular endothelial growth factor [6]. The neovascularization in the retina of our patient might be associated with the angiogenic tendencies in CIMF. The results suggest that peripheral retinal vessel occlusion and neovascularization may be associated with CIMF.
Notes
No potential conflict of interest relevant to this article was reported.