The Prevalence and Demographic Characteristics of Anterior Polar Cataract in a Hospital-Based Study in Korea
Article information
Abstract
Purpose
Anterior Polar Cataract (APC) develops by a mechanism different from that of other age-related cataracts, and outside of Korea, it is an extremely rare condition. We investigated the prevalence and epidemiological characteristics of APC in Koreans.
Methods
The evaluation on the prevalence of APC in comparison to the other age-related cataracts was performed on the 2,108 cataract patients who were treated at 5 different areas in Korea from August 2003 to December 2003. The demographic characteristics of APC were studied on the, 656 cataract patients who were treated from January 2004 to January 2005 at one hospital. These patients were classified according to the type of lens opacity (nuclear, cortical, posterior subcapsular, mixed and APC).
Results
The prevalence of patients with APC among all the cataract patients was 6.02% during the 5 months in this hospital-based study. Eighty-seven per cent of patients with APC were male. In contrast, the proportion of female was greater than 50% in the other cataracts. The mean age of APC patients was 52.7 years. Among the APC patients, 38.9% were under 50 years of age, 42.6% in their 50s, 14.8% in their 60s, and 3.7% were in their 70s. However, 80% of patients were over the age of 60 years in nuclear, cortical, and mixed-type cataracts.
Conclusions
The prevalence of APC among all cataracts was high in comparision with another country. The proportion of APC was high in individuals younger than 60 years of age, and in males.
Medical treatment has not been proven yet to prevent, delay, or reverse the development of cataract, although it causes a major visual impairment among affected individuals and results in significant health resource consumption for populations and society.1 Age-related cataract is usually a gradual, progressive opacification of the crystalline lens resulting in impaired visual fuction. The various epidemiological studies have reported the prevalence and etiology of age-related cataracts, the opacification of the lens.2-6
The developmental mechanism of APC is distinguished from that of other age-related cataracts. APC is caused by opacity beneath the anterior capsule of the lens as a result of transdifferentiation of lens epithelial cells.7 This change is different from the change of lens fiber proteins in the other types of cataracts.
Although identifying the epidemiology for cataract may help establish preventative measures, to our knowledge, there has never been a paper which has specifically recorded an epidemiological study of APC in other countries. Thus, in this study, the prevalence and demographic characteristics of APC were investigated.
Materials and Methods
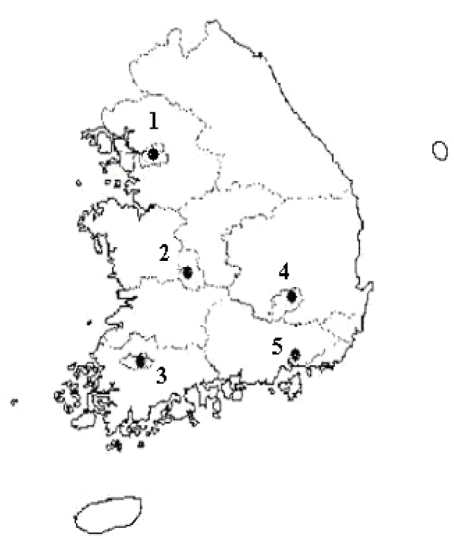
A two-stage screening process was used to recruit subjects in Korea. In the primary process, we investigated the proportion of APC to other cataracts. From August 2003 to December 2003, 2,108 cataract patients were collected for multiple general hospital survey, to examine the prevalence of APC. Seoul, Daejeon, Kwangju, Daegu, and Pusan were included in the survey districts (Fig. 1). Ophthalmologists in the eye centers completed a short eligibility form for each of their cataract patients. In the second process, from January 2004 to January 2005, 656 cataract patients were collected at one hospital to investigate the demographic characteristics including the age and the sex of APC patients.
A patient was included in the study if at least one eye had lens opacities occurring alone, a best corrected visual acuity of 20/32 or worse, and had no other condition for the vision loss. A more detailed examination including the lens examination after dilation of the pupil, slit lamp biomicroscopy and direct ophthalmoscopy were done. If one eye qualified as a case and the patient's the other eye had a different type of opacity, the patient was excluded from the study. Also, subjects having congential cataracts were excluded.
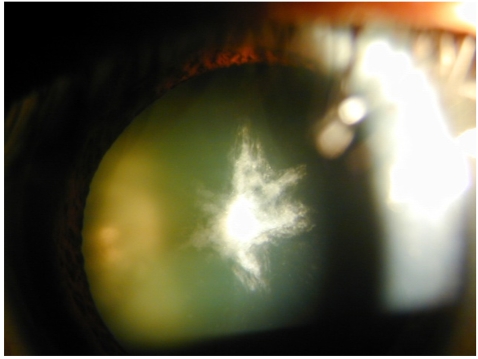
The type of lens opacity was classified based on the method of the Lens Opacities Classification System III (LOCS III),8 and the APC type was added to it and used. APC was present when dots or star-shaped opacities occupied the axial area of the anterior polar area (Fig. 2).
Statistical analysis was performed using SAS® software (Version 8.01, SAS Institute Inc., Cary, NC). The chi square test was used to confirm the sex distribution by cataract type. TSs, and a p-value less than 0.05 was considered statistically significant.
Results
Table 1 shows the proportion of APC to total cataracts during the 5 months in this hospital-based study. The prevalence of APC was 6.02% among total cataract patients. Locally, Seoul area having the prevalence of 9.58% showed the highest prevalence among the five areas. The prevalence of APC in Daegu and Pusan were 6.12% and 8.77%, respectively. The prevalence of APC to total cataracts in Kwangju and Daejeon were 2.51% and 2.06%, respectively.
Figure 3 presents the demographic distributions by type of cataract. In other cataracts the female proportion was high (greater than 50%) but, of those affected with APC, the male proportion was 87.0% (Chi-square test, p<0.001).
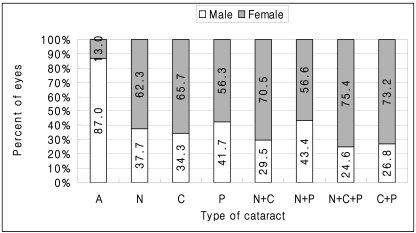
Distribution of women and men by cataract type.
(A) Anterior polar (n=54), (N) Nuclear (n=77), (C) Cortical (n=210), (P) Posterior subcapsular (n=47), (N+C) Nuclear+Cortical (n=95), (N+P) Nuclear+Posterior subcapsular (n=53), (N+C+P) Nuclear+Cortical+Posterior subcapsular (n=65), (C+P) Cortical+Posterior subcapsular (n=55). Chi-square test, p<0.001.
The mean age of nuclear and cortical cataract patients were 66.9 and 67.2 years, respectively and that of patients with mixed cataract was 70~71 years, which was the typical cataract pattern. The mean age of posterior subcapsular cataract patients was 58.5 years. The mean age of APC, in particular, was 52.7 years which is significantly lower than in other types (ANOVA, Scheffe test, p<0.001) (Fig. 4). Also, in nuclear, cortical, and mixed-type cataracts, 80% of patients were over the age of 60 years. However, in APC, the proportion under 50 years of age was 38.9%, the proportion in their 50s was 42.6%, the proportion in their 60s was 14.8%, and the proportion in their 70s was 3.7%(ANOVA, Scheffe test, p<0.001) (Fig. 5).
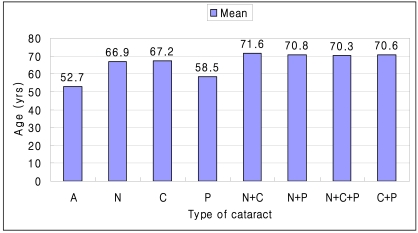
Mean age by cataract type.
(A) Anterior polar (n=54), (N) Nuclear (n=77), (C) Cortical (n=210), (P) Posterior subcapsular (n=47), (N+C) Nuclear+Cortical (n=95), (N+P) Nuclear+Posterior subcapsular (n=53), (N+C+P) Nuclear+Cortical+Posterior subcapsular (n=65), (C+P) Cortical+Posterior subcapsular (n=55). ANOVA, p<0.001.
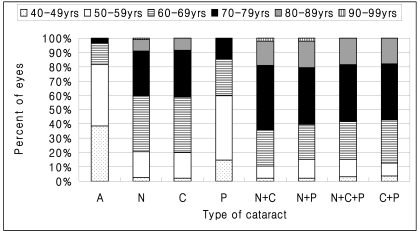
Distribution of age by cataract type.
(A) Anterior polar (n=54), (N) Nuclear (n=77), (C) Cortical (n=210), (P) Posterior subcapsular (n=47), (N+C) Nuclear+Cortical (n=95), (N+P) Nuclear+Posterior subcapsular (n=53), (N+C+P) Nuclear+Cortical+Posterior subcapsular (n=65), (C+P) Cortical+Posterior subcapsular (n=55). ANOVA, Scheffe test, p<0.001.
Discussion
Cataract is the leading cause of blindness in the world, and most cataracts are age-related.9 According 1998 World Health Report, it is estimated that there were over 19 million people blinded from cataract, which represented 43% of global blindness.10 The definitive management for cataract is surgical extraction with intraocular lens implantation. Even though cataract surgery is an effective cure, research into causative factors and pathomechanisms to delay and prevent the development of cataract is a major challenge for the 21st century.11 Reports from the longitudinal studies of epidemiology for cataract are becoming available to clarify prevalence and risk factors identified in previous studies.2 However, epidemiology for APC seems to lack sufficient research. Thus, we investigated the prevalence and demographic characteristics of APC in Korea. The purpose of this study was to contribute to the baseline study that is emerging in regards to characteristics associated with APC, which occurs in relatively younger men compared to other cataract patients.
In this study, during the predetermined period, the mean age of APC patients was 52.7 years, and the proportion of patients younger than 50 years of age was 38.9%. In addition, APC most often occurred in young people against the other age-related cataracts. Kim et al.12 has reported that the average age of APC patients was 51.9 years in Korea. The demographic distribution of APC has not yet been reported in any other country; however, the distribution appears to be substantially different from that of other age-related cataracts. Leske et al.13 showed that in cataract patients, the mean ages of patients with nuclear, cortical, posterior subcapsular, and mixed cataracts were 69.0, 65.3, 61.8, and 67.5 years, respectively. The proportions of patients younger than 50 years of age were 7.3, 17.9, 34.7, and 14.1%, respectively.13
In the Age-Related Eye Disease Study (AREDS), the proportions of male patients with moderate nuclear and moderate cortical cataracts were 37.0% and 42.0%, respectively.14 Our study has shown, by contrast, the distribution of APC was significantly higher in males, and males represented 87.0% of all patients with APC.
The age-standardized prevalence was 3.9% in persons aged 60 to 80 years in Copenhagen, Denmark.15 The prevalence of nuclear, cortical and posterior subcapsular cataract were 9.1%, 11.4%, and 10.2%, respectively, in Australian urban population aged 40 years old excluding previous cataract surgery.16 In Korea, the prevalence of cataract based on aged 40 years and older was 32.8% in mountainous area (Choung Won) and 45.2% in rural area (Mun Kyung).17 In this study we found 127 persons (6.02%) having APC from among the 2,108 persons with cataracts in 5 areas of Korea.
The developmental mechanism of APC is the proliferation of lens epithelial cells in the anterior subcapsular lens without migration to the equatorial area, resulting in proliferated cells accumulating in the anterior subcapsule as several layers.7 This phenomenon is different from the mechanisms of other cataracts. It is limited to the anterior subcapsular area, and lens opacity occurs in a relatively small area. It may, however, induce severe vision disturbance.18 As shown by our results, APC occurred mainly in males aged 40 to 60 years causing severe vision impairment in this productive population and leading to heavy losses in the social and economic fields. Interestingly, the Beaver Dam Eye Study showed that postmenopausal hormone replacement therapy is associated with a decreased risk of nuclear sclerosis.19 Recent epidemiologic studies suggest that female hormones play a role in protecting against cataract.20 Animal study also indicates a correlation between a higher incidence of cataract in women and the lack of estrogen.21 However, as shown by Zhang, estrogen, progesterone, or androgen receptors were not found in lens epithelial cells of 50 patients with age-related cataract.20 Therefore, the mechanism research is required that estrogen receptor protects transdifferentiation of lens epithelial cells causing APC in female.
We think that primary prevention will bring much better chance for decreasing the incidence of cataract. APC is being starved of epidemiologic studies as a baseline. Although this study was limited by the short-term and hospital based survey, these data could be used to address the basis of epidemiologic study on the prevention of APC. A long-term epidemiologic study on APC that occurs frequently only in Koreans is required in the future together with pertinent research on its mechanism, since APC cataract is caused by the change of lens epithelium in anterior polar region of lens that is different from the causality of other cataracts.
Acknowledgement
The authors thank the anterior polar cataract study team, in particular, Seon-Ho Kim, Hyung-Jun Kim, Jong-Il Park, and Si-Hwan Choi, who collected the patients with anterior polar cataract. Also, the authors would like to thank the volunteers for participating in this study.
Notes
This study was supported by the Korean Academy of Medical Sciences, Korea.