Dacryoendoscopic Findings in the Failed Silicone Tube Intubations without Dacryoendoscopy
Article information
Abstract
Purpose
To investigate the clinical characteristics and dacryoendoscopic findings and clinical efficacy of silicone tube intubation (STI) in the patients who referred to our center due to failed with conventional STI.
Methods
We retrospectively reviewed the medical records of 61 cases from 50 patients who underwent STI or endoscopic dacryocystorhinostomy using dacryoendoscopy from January 2016 to May 2021. Clinical characteristics, tear meniscus height, lacrimal irrigation test, dacryocystographic findings, dacryoendoscopic findings and surgical outcomes were evaluated.
Results
The study included 12 male and 38 female patients (mean age, 64.1 ± 13.2 years). In the preoperative lacrimal irrigation test, passage was found in 33 eyes (54.1%) and no passage in 28 eyes (45.9%). The causes of lacrimal duct obstruction were in the order of stenosis (31.1%), mucus (27.9%), membrane (24.6%), granulation (13.1%), and stone (3.3%), and the location were in the order of nasolacrimal duct (39.3%), lacrimal sac (36.1%), canaliculus (21.3%), and inferior meatus (3.3%). As for the characteristics of obstruction, the secretory type was 21 eyes (34.4%), and structural change type was 40 eyes (65.6%). The STI group consisted of 57 eyes (93.4%) and endoscopic dacryocystorhinostomy consisted of four eyes (6.6%). The overall success rate was 83.9%. Clinical results were correlated with dacryoendoscopic finding (p = 0.015), but not with lacrimal irrigation test or dacryocystography. The structural change type had a higher surgical success rate than the secretory type (84.4% vs. 66.7%, p = 0.015). In particular, the structural change type showed higher success rate than the secretory type below the lacrimal sac (95.5% vs. 61.9%, p = 0.034).
Conclusions
STI using dacryoendoscopy has a higher surgical success rate than conventional STI since dacryoendoscopy provides direct visualization of nasolacrimal duct obstruction. It could be useful in increasing the surgical success rate in patients with structural changes below lacrimal sac.
Nasolacrimal duct obstructions induce severe epiphora and recurrent infections with mucopurulent discharge, and thereby visual impairment [1,2]. Conservative treatments only achieve temporary relief of symptoms; thus, surgery is the treatment of choice. In the treatment of nasolacrimal duct obstruction, there are silicone tube intubation (STI) and dacryocystorhinostomy (DCR) [3,4].
STI is one of the surgical treatments that is applied for the patients who failed conservative treatment in nasolacrimal duct obstruction. The surgical success rate of STI using dacryoendoscopy higher than that of conventional STI. Because surgery can be performed by identifying the internal structure of the lacrimal duct system [5,6].
Of the normal structure of lacrimal drainage system (LDS) in the dacryocystography (DCG), it was found that about 73% of the cases were obstructed in the dacryoendoscopy. Dacryoendoscopy allows for a comprehensive investigation of the lacrimal path and can help to understand phenomena that are not confirmed by other tests [7].
Factors of patients who failed STI are being studied, but few studies have been conducted on the findings of the dacryoendoscopic findings. Therefore, in this study, we aimed to investigate clinical characteristics of referred patients due to failed with conventional STI and to analyze dacryoendoscopic findings and determine clinical efficacy of STI guided with dacryoendoscopy.
Materials and Methods
Ethics statement
This study and data collection were approved by the Institutional Review Board of CHA Bundang Medical Center (No. 2022-06-023) and our study design adhered to the tenets of the Declaration of Helsinki. Informed consent was obtained from each subject before enrollment.
Study design
We retrospectively reviewed the medical records of 61 cases from 50 patients who underwent STI or endoscopic DCR (endo-DCR) using dacryoendoscopy from January 2016 to May 2021. Patients who referred to our hospital due to failed with conventional STI was included. Patients with previous DCR were excluded from the study.
Prior to surgery, irrigation test and dacryocystography (DCG) was performed. For the irrigation test, saline was injected through the lacrimal punctum using a 2-mL syringe connected to a 26G ophthalmic cannula. It was checked whether the saline passed through the nose. The results of the irrigation test were classified as “passed” and “not passed,” and complete passed and partially passed were included as “passed.” DCG was performed to evaluate the obstructed site, using a water-soluble contrast agent, lohexol (Bonorex; Central Medical Service, Seoul, Korea). The DCG findings were classified into two patterns: primary and secondary. The primary pattern included partial or complete obstruction; the secondary pattern included beading or dilation of the lacrimal sac in DCG.
Surgical instrument and procedures
In this study, the dacryoendoscope used (FT-203F; Fibertech Co., Tokyo, Japan) had the following specifications: probe outer diameter, 0.9 mm; field of view, 70°; number of image elements, 6,000; and observation depth, 1 to 10 mm. The probe of the endoscope was bent at a 27° angle, 1 cm from its tip. A sheath (angiocatheter, 0.92 mm; Daewon, Seoul, Korea) was wrapped around the probe for covering and dilation of the lumen, with back and forth movement possible inside lacrimal duct system. The nasal endoscope (7208CA; Carl Strotz, Tuttlingen, Germany) had the following specifications: probe outer diameter, 2.7 mm; view angle direction, 0°; and number of image elements, 410,000.
The type of obstruction was defined according to dacryoendoscopic findings for the occluded area, i.e., video images of the canaliculus to the inferior meatus. Obstruction can be classified into two groups: secretory versus structural groups. The secretory group encompassed mucus, stones, and granulation, and the structural group included fibrotic membrane and stenosis (Fig. 1A). The pattern of obstruction was divided into focal and diffuse based on the length of obstruction longer than 2 mm through the dacryoendoscopic examination
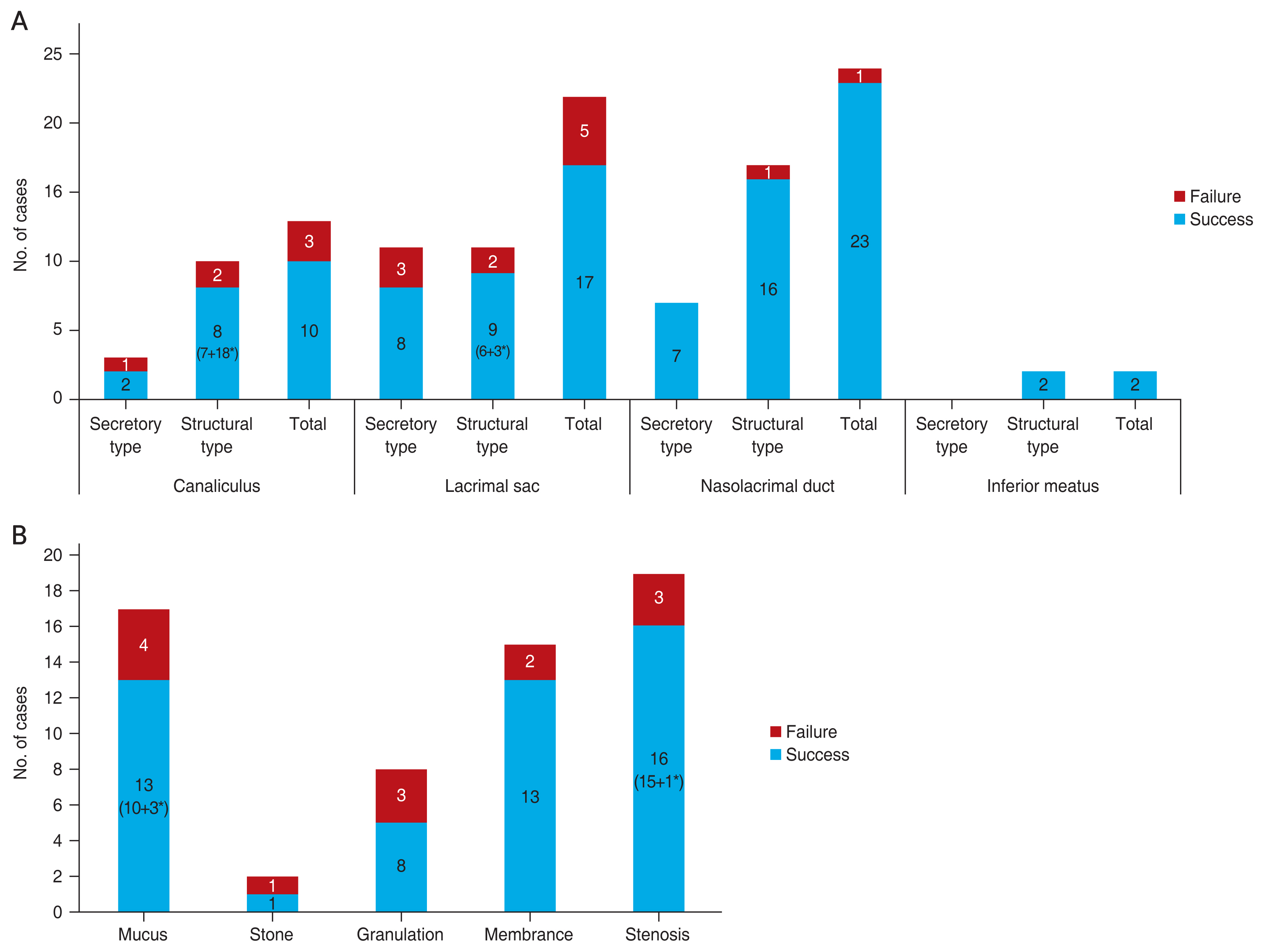
Dacryoendoscopic findings of nasolacrimal duct system in the failed with conventional silicone tube intubation. (A) Dacryoendoscopic findings according to the level of obstruction. The frequencies were as follows: nasolacrimal duct, 39.3%; lacrimal duct, 36.1%; canaliculus, 21.3%; and inferior meatus, 3.3%. (B) Dacryoendoscopic findings according to the obstruction type. The frequencies of the dacryoendoscopic findings were as follows: stenosis, 31.1%; mucus, 27.9%; membrane, 24.6%; granulation, 13.1%; and stone, 3.3%. *Endoscopic dacryocystorhinostomy.
For STI, two to four drops of proparacaine hydrochloride 0.5% (Alcaine; Alcon, Fort Worth, TX, USA) were applied to the conjunctival sac. Local anesthesia and vasoconstriction of the nasal mucosa were performed with 0.01% epinephrine added to 4% lidocaine intranasal spray. After subconjunctival local injection of 2% lidocaine 2.5 mL with a 30G needle, the upper and lower lacrimal puncta were dilated, and the dacryoendoscope was inserted through the upper and lower puncta. The dacryoendoscope was moved slowly toward the canaliculus and forward gently to the lacrimal sac. On reaching the lacrimal sac, the dacryoendoscope was held upright and thrust forward to the occluded portion of the lacrimal duct under the visual guidance of a dacryoendoscope. When the stenotic lacrimal duct system was confirmed by dacryoendoscopy, probing and clearing of the lacrimal duct system were performed using a customized sheath made with an 18G catheter like trephine or dilator to recanalize the lacrimal passage. And then 0.5% moxifloxacin ophthalmic solution (Vigamox, Alcon) and 0.1% fluorometholone ophthalmic solution (Flumetholon; Santen, Osaka, Japan) were irrigated through the LDS. A bicanalicular silicone tube with a diameter of 0.94 mm (Yoowon Meditec, Seoul, Korea) was inserted through the sheath under visual guidance. The sheath and the tube were retrieved, and both ends of the tube were locked and stabilized under the inferior turbinate. After STI, 0.5% levofloxacin ophthalmic solution (Cravit, Santen) and 0.1% fluorometholone ophthalmic solution (Flumetholon) were administered four times a day for a month, and oral antibiotics were taken for 1 week.
Outcome measures
As a baseline test, tear meniscus height of the lower lid was measured with a spectral domain optical coherence tomography system (Spectralis; Heidelberg Engineering, Heidelberg, Germany). After STI or endo-DCR, the patients were followed up 1 week for the first time, every 1 month until 6 months postoperatively. After 6 months, extubation of silicone tube was performed and they were followed up every 6 month. Surgeries were defined to be successful when the postoperative Munk score was 0 or 1, tear meniscus height was <300 μm, and the irrigation test was passed after extubation.
Statistical analysis
Statistical analysis was performed using IBM SPSS ver. 23.0 (IBM Corp., Armonk, NY, USA). A paired t-test was performed before and after surgery. A p-value of <0.05 was considered statistically significant.
Results
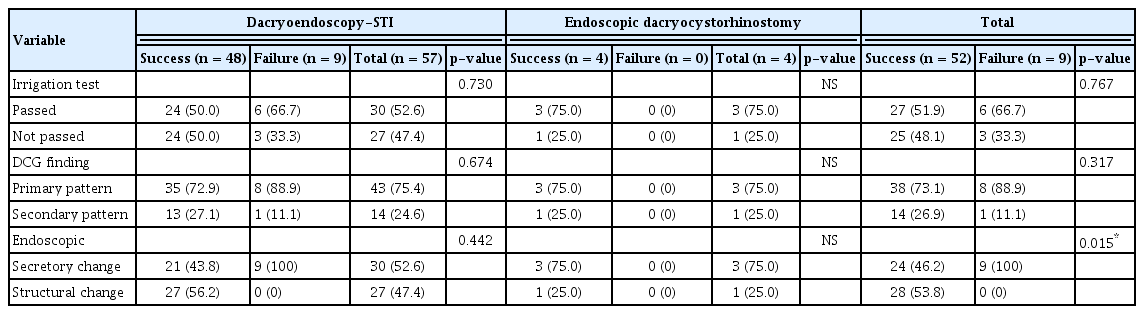
In total, 61 eyes of 50 patients (16 male and 45 female) underwent silicone intubation (57 eyes) or endo-DCR using dacryoendoscopy (four eyes). The mean age of the patients was 64.1 ± 13.2 years and the epiphora duration was 4.7 ± 5.3 years. The mean duration from previous surgery to reoperation was 4.1 ± 5.2 years. In saline irrigation testing, 33 eyes (54.1%) showed passage and 28 eyes (45.9%) did not. Endo-DCR was performed when difficult to proceed with dacryoendoscopy due to severe stenosis and structural changes. Silicon tube intubation was performed in 57 eyes (93.4%) and the success rate was 84.2%. Endo-DCR was performed in four eyes (6.6%) and all were success (Table 1).
The dacryoendoscopic findings were as follows: 19 stenosis cases (31.1%), 17 mucus cases (27.9%), 15 membrane cases (24.6%), eight granulation cases (13.1%), and two stone cases (3.3%). Among them, endo-DCR were three mucus and one stenosis cases (Fig. 1B).
The dacryoendoscopic findings according to the level of obstruction were as follows: 24 nasolacrimal duct cases (39.3%), 22 lacrimal duct cases (36.1%), 13 canaliculus cases (21.3%), and two inferior meatus cases (3.3%). Obstruction type was divided into two types: secretory type, such as mucus, stone, granulation, pus, and structural change type, such as stenosis, edema and fibrosis (Fig. 1A).
In DCG findings, secondary pattern such as lacrimal sac dilation was found in 24.6%. The ratio of secretory change and structural change of dacryoendoscopic findings was similar (54.1% vs. 45.9%). The results of STI using the dacryoendoscopy did not correlated with the irrigation test and DCG findings, but endoscopic findings were statistically significant (p=0.015) (Table 2).
Of the total 61 subjects, they were examined inside the LDS using dacryoendoscopy and four eyes underwent DCR for patients’ preference of DCR. Therefore, they were excluded from the outcome analysis of dacryoendoscopy guided STI.
The type and pattern of dacryoendoscopy were not correlated with irrigation test or DCG findings. The success rate of the structural change group (100.0%) was significantly higher than that of the secretory change group (70.0%), and the focal group (91.0%) was significantly higher than that of the diffuse group (61.5%) (Table 3).
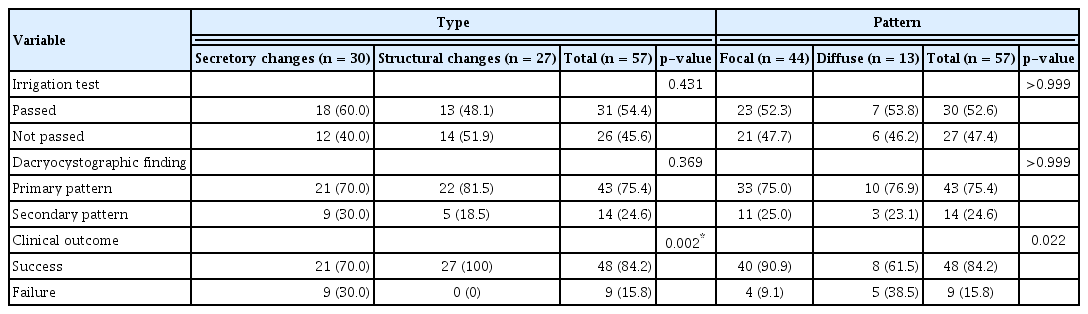
Dacryoendoscopic findings associated with the characteristics of obstruction in the patients who failed with conventional silicone tube intubation (n = 57)
The level of obstruction was divided into the presac, the sac and postsac. The patients who passed in saline irrigation test were more associated with sac and postsac. In the sac and postsac of obstructive level, when the dacryoendoscopic findings are secretory changes, secondary pattern such as beaded or sac dilation are more found in DCG. The surgical success rate was significant higher in the structural changes than secretory changes in the sac and postsac (Table 4).
Discussion
The success rate of STI in patients with nasolacrimal duct obstruction was variously reported as 51.6% to 83.0% [8]. This is because each study had a different degree of nasolacrimal duct obstruction, a different definition of surgical success, and a different duration of follow-up [9]. In particular, the surgical success rate was reported to be higher in patients with mild nasolacrimal duct obstruction or undergoing STI for the first time. It was commonly suggested that the factors affecting the success of STI were the preoperative saline irrigation test and the degree of obstruction. Factors affecting the success rate are age, the degree of obstruction and the duration of follow-up [10,11]. Recently, studies on long-term results after surgery are being conducted gradually. According to Koh et al. [12], the conventional STI success rate was 68.3% and the factors affecting the surgical success rate were the elderly of a history of facial palsy and the risk of recurrence was lower in functional nasolacrimal duct obstruction than in complete nasolacrimal duct obstruction.
In a previous study, mucus (39.9%) was the most common obstructive factor confirmed by dacryoendoscopy in patients with primary acquired nasolacrimal duct obstruction, followed by membrane (19.2%), stone (9.4%), granulation (8.9%), and stenosis (2.7%) [13]. Unlike the previous study, in this study, patients who failed treatment with conventional silicone intubation, stenosis, which was identified as the lowest factor in the previous study, was identified as the most common factor. This result suggests that the possibility of recurrence is higher in structural stenosis than functional obstruction using conventional surgical technique without visualization inside lacrimal duct system. And the level of obstruction is the most common in the lacrimal duct, followed by the lacrimal sac, canaliculus, and inferior meatus. Therefore, it may be more associated with failure of recanalization of conventional technique in patients and obstruction at the level below the lacrimal sac.
In this study, the success rate of STI was 84.2% and that of endo-DCR was 100%. Endo-DCR is the method of choice when STI is not possible due to the inability to recanalize the dacryoendoscopy. Previous studies have reported that the success rate of endo-DCR ranged from 82.4% to 92.0%, higher than STI, especially stenosis type and mucus type [14–16]. In our study, as in previous studies, the success rate of endo-DCR was higher than that of STI, but the difference in the success rate of these two methods can be attributed to the different surgical indications. The subjects of this study were all patients who were initially able to insert a silicone tube. However, in patients who failed once at STI, the disease can progress so much that it would be impossible to even advance a silicone tube, and it requires further invasive treatment. So, the failure of conventional STI could lead to the state of worse symptoms and more fibrotic nasolacrimal duct in the end.
In conclusion, dacryoendoscopy has a higher surgical success rate than that of conventional STI because it can be directly visualized and treated according to the cause of the nasolacrimal duct system. Therefore, dacryoendoscopy provides the better understanding and proper management of in nasolacrimal duct obstruction even for the patients who were failed with conventional STI, and it could be a safe and effective tool for the nasolacrimal duct obstruction patients whose obstruction was caused by structural changes at the lacrimal sac and nasolacrimal duct.
Acknowledgements
None.
Notes
Conflicts of Interest: Helen Lew is a member of the Editorial Board of the Korean Journal of Ophthalmology since 2015. However, she was not involved in any process of evaluation or review for this article. Otherwise, no other potential conflicts of interest relevant to this article were reported.
Funding: None.