Frontalis Sling Using a Silicone Rod for Ptosis in Third Nerve Palsy: Cosmesis versus Safety
Article information
Abstract
Purpose
To evaluate the results of the frontalis sling operation using a silicone rod for the correction of ptosis in patients with third nerve palsy with a focus on corneal safety.
Methods
Patients with third nerve palsy who underwent the frontalis sling operation using a silicone rod between 2008 and 2019 were included in this study. The medical records of all patients were reviewed, and their clinical characteristics and postoperative outcomes were analyzed. In this retrospective, interventional case series, the main outcome measures were eyelid contour, eyelid height by margin reflex distance, and corneal status.
Results
Twenty-four eyes of 18 patients (12 male and six female patients) were included. The mean age at the time of surgery was 35.1 years (range, 5–64 years). Twelve patients underwent a unilateral ptosis operation, and six patients received a bilateral ptosis operation. The mean follow-up period was 32.1 months (range, 2–87 months). Most patients (21 of 24 eyes, 88%) showed poor Bell’s phenomenon on preoperative examination. Satisfactory eyelid height and eyelid contour were achieved in almost all patients (mean postoperative margin reflex distance, +1.2 mm) postoperatively. Although corneal erosions were detected for several months in eight of 24 eyes after surgery, these findings were well controlled medically with artificial tear eye drops and ointments.
Conclusions
Frontalis sling surgery using a silicone rod can safely and effectively correct ptosis without severe corneal complications in patients with third nerve palsy. Our study outlines a new method to define the postoperative safety outcome by specifically focusing on categorized corneal status.
Third cranial nerve palsy (3rdNP, oculomotor palsy) is a condition caused by damage to the oculomotor nerve, leading to decreased function of the various muscles it controls. This condition occurs due to vascular disease, trauma, aneurysm, or tumors [1]. Common clinical manifestations of 3rdNP are strabismus, limitation of extraocular movement, ptosis, and mydriasis. Blepharoptosis is a common consequence of 3rdNP and can be difficult to manage [2]. The ptotic eyelid may obscure the pupil, causing amblyopia in children and functional and cosmetic problems in adults. The severe ptosis associated with 3rdNP can present challenging management problems. This form of ptosis often involves poor levator muscle function, necessitating frontalis sling operation in many cases [3]. However, because of the limited upgaze in patients with 3rdNP, many show poor Bell’s phenomenon, making the cornea vulnerable to exposure keratopathy after the surgery. Among the many suspension materials currently used for frontalis sling operations, silicone rods offer good elasticity for favorable eyelid blinking and simple adjustability in revision surgery [4,5]. Therefore, frontalis sling surgery using a silicone rod could be a good treatment option in managing severe ptosis due to 3rdNP in cases showing the possibility of postoperative corneal complications.
To date, there are a few articles [6–8] reporting on frontalis sling surgery using a silicone rod related to 3rdNP. Bagheri et al. [6] reported 18 patients of 3rdNP who received levator resection and frontalis sling procedures; however, the types of suspension materials used are mixed in sling surgery: silicone rods and Supramid (S. Jackson, Alexandria, VA, USA) or fascia. One case report [7] mentioned the efficacy of using silicone rods as a suspension material in frontalis sling surgery. However, in these papers, postoperative corneal status was not the main outcome measure. Until now, many studies [8–11] have covered the functional and cosmetic outcomes in frontalis sling surgery. However, in patients with 3rdNP who have poor corneal protective mechanism, the safety outcomes for the cornea should be clearly emphasized. This study aimed to investigate the surgical results of frontalis sling surgery using a silicone rod in 3rdNP by specifically focusing on the condition of the cornea. In addition, we investigated the safe eyelid height for the cornea postoperatively.
Materials and Methods
This retrospective, interventional case series was approved by the institutional review board of Seoul National University Bundang Hospital (No. B-2004-608-102). The current study involving the surgical procedure was carried out in adherence to the tenets of the Declaration of Helsinki. Informed consent was not required; the institutional review board granted a waiver of informed consent for this retrospective chart review study. All operations were performed by a single surgeon.
Patients with 3rdNP who underwent frontalis sling surgery with a silicone rod for ptosis correction between 2008 and 2019 were included in this study. The patients’ clinical characteristics and surgical outcomes were retrospectively analyzed by reviews of medical records and photographs. The obtained data included information on sex, age, visual acuity, laterality of 3rdNP, extraocular movement, Bell’s phenomenon, levator function, preoperative and postoperative margin reflex distance (MRD), laterality of surgery, type of surgery performed, type of suspension material used, postsurgical status of the cornea, and presence of sling adjustment. The levator function was classified into three groups: poor (4 mm or less), moderate (between 5 and 7 mm), and good (8 mm or more). The Bell’s phenomenon was categorized into three stages: poor, moderate, and good.
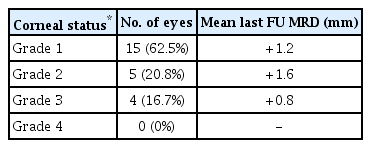
Surgical techniques
Surgery was performed under local or general anesthesia depending on the patient’s age. Lidocaine (2%) mixed with 1:100 000 epinephrine was injected in the operation site. Five horizontal incisions were made with a No. 15 blade in a pentagonal shape, of which two were made 3 mm above the upper eyelid margin and three above the brow. Two horizontal incisions were made at the upper eyelid margin, and dissection was performed with sharp Wescott scissors through the orbicularis oculi muscle. After the plane of tarsus was exposed, two 6-0 polypropylene sutures were preplaced at the tarsal plate. After that, the Wright needle was passed above the tarsus, and the silicone rod (Visitec; BD Ophthalmics, Franklin Lakes, NJ, USA) was brought under the pretarsal orbicularis oculi. The silicone rod was fixed to the tarsal plate by tying the preplaced polypropylene sutures. A Jaeger lid plate was placed under the eyelid, and its tip was placed just under the superior orbital rim. The medial and lateral aspects of the silicone rod were passed towards the medial and lateral brow incisions, respectively, and then redirected toward the central brow incision with the Wright needle. The tips of the silicone rods were gathered together with a sleeve, and the upper eyelid was pulled up high until the MRD was +1.0 mm. The sleeve was tied with 6-0 polypropylene sutures and situated in the central brow incision. The subcutaneous tissue of the central incision was sutured with 6-0 vicryl. The skin incisions of the brow were closed with 6-0 polypropylene (Fig. 1A–1F).
Description of the sling surgery, drawn by the authors of this article. (A) Indication of five stab incision. (B) Passage of the rod through the two eyelid incision sites, from point I to point II. (C) Passage of the lateral end of the rod, from eyelid incision site (point II) to lateral suprabrow incision site (point III). (D) Passage of the medial end of the rod, from medial eyelid incision site (point I) to medial suprabrow incision site (point V). (E) Exit of both tips of the rod through the central suprabrow incision site (point IV). (F) Tips of the rod brought within a sleeve.
Both, artificial tear eye drops and ointments, were started immediately after the frontalis sling operation. Patients visited our hospital at 1 week, 1 month, and 6 months postoperatively. Postoperative eyelid contour, eyelid height by MRD, and corneal condition were examined at each checkup. In cases showing overcorrected or undercorrected ptosis at 1 week, eyelid height was adjusted to achieve the targeted eyelid height.
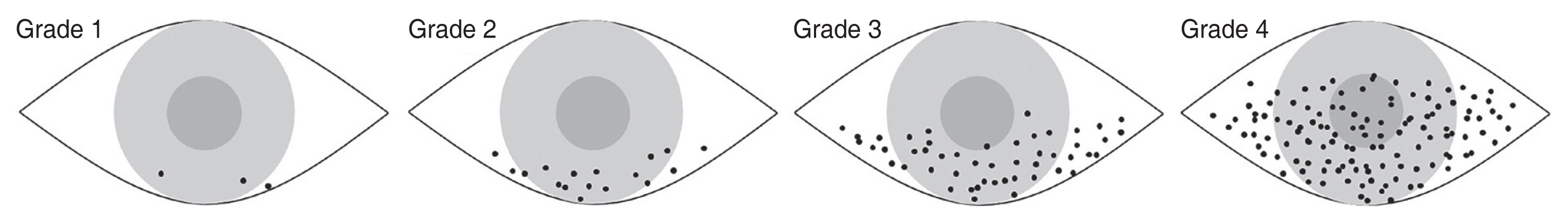
Corneal status evaluation
The postoperative corneal status was categorized and evaluated as follows: grade 1, no or minimal erosions; grade 2, mild erosions easily controlled by topical eye drops and ointments; grade 3, moderate erosions but controlled by medical therapy; and grade 4, severe, persistent erosions or infiltration requiring additional surgery (Fig. 2).
Statistical analysis
Statistical analysis was performed using IBM SPSS ver. 22.0 (IBM Corp., Armonk, NY, USA). The variables were analyzed using the Mann-Whitney U-test, Kruskal-Wallis test, and linear-by-linear association. Statistical significance was set at p < 0.05.
Results
A total of 24 eyes of 18 subjects with 3rdNP (12 male and six female patients) were enrolled in this study. Eleven of them showed a unilateral presentation, while seven showed a bilateral presentation of 3rdNP. The etiologies of 3rdNP were traumatic in six patients, congenital in five, vascular in four, tumor in one, inflammatory in one, and undetermined in one case. Frontalis sling operation with a silicone rod was performed on 24 eyelids of 18 patients; one patient who had presented with bilateral ptosis underwent unilateral surgery. Eleven of the 18 patients underwent strabismus surgery at the same time. The mean age at the time of ptosis surgery was 35.1 years (range, 5–64 years). The mean follow-up period was 32.1 months (range, 2–87 months).
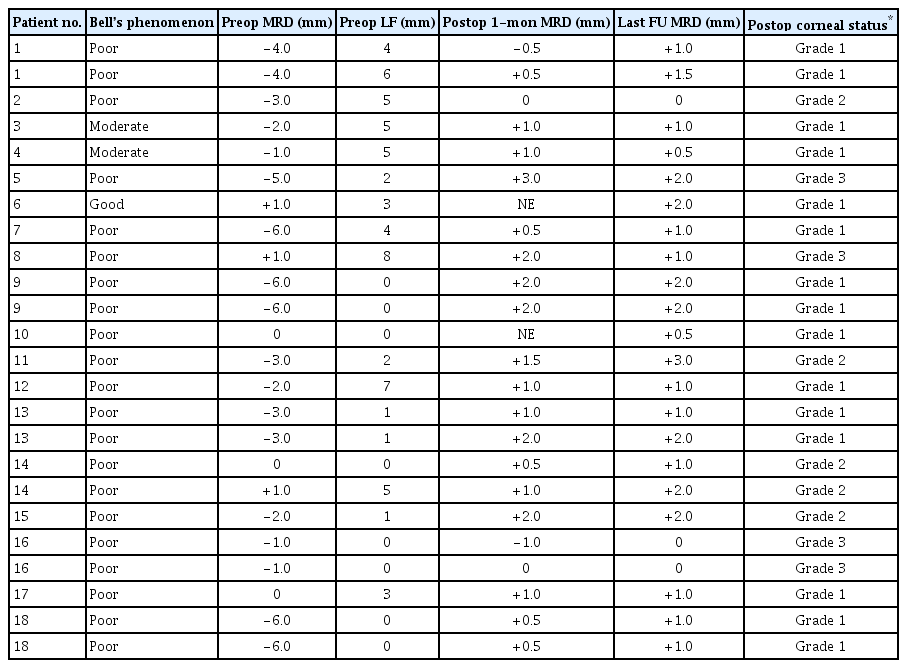
The preoperative Bell’s phenomenon was poor in 21 eyes (87.5%), moderate in two (8.3%), and good in one eye (4.2%). The preoperative levator function was poor in 17 eyes (70.8%), moderate in six (25.0%), and good in one eye (4.2%). Mean preoperative MRD was −2.5 mm (range, −6.0 to +1.0 mm) and the mean MRD at 1 week after the operation was +1.2 mm (range, −0.5 to +3.0 mm). The mean MRD at 1 month after sling surgery, 6 months after surgery, and at the last follow-up was +1.0 mm (range, −1.0 to +3.0 mm), +1.1 mm (range, −1.0 to +2.0 mm), and +1.2 mm (range, 0 to +3.0 mm), respectively. The demographic characteristics and clinical data of all patients are presented in Tables 1 and 2.
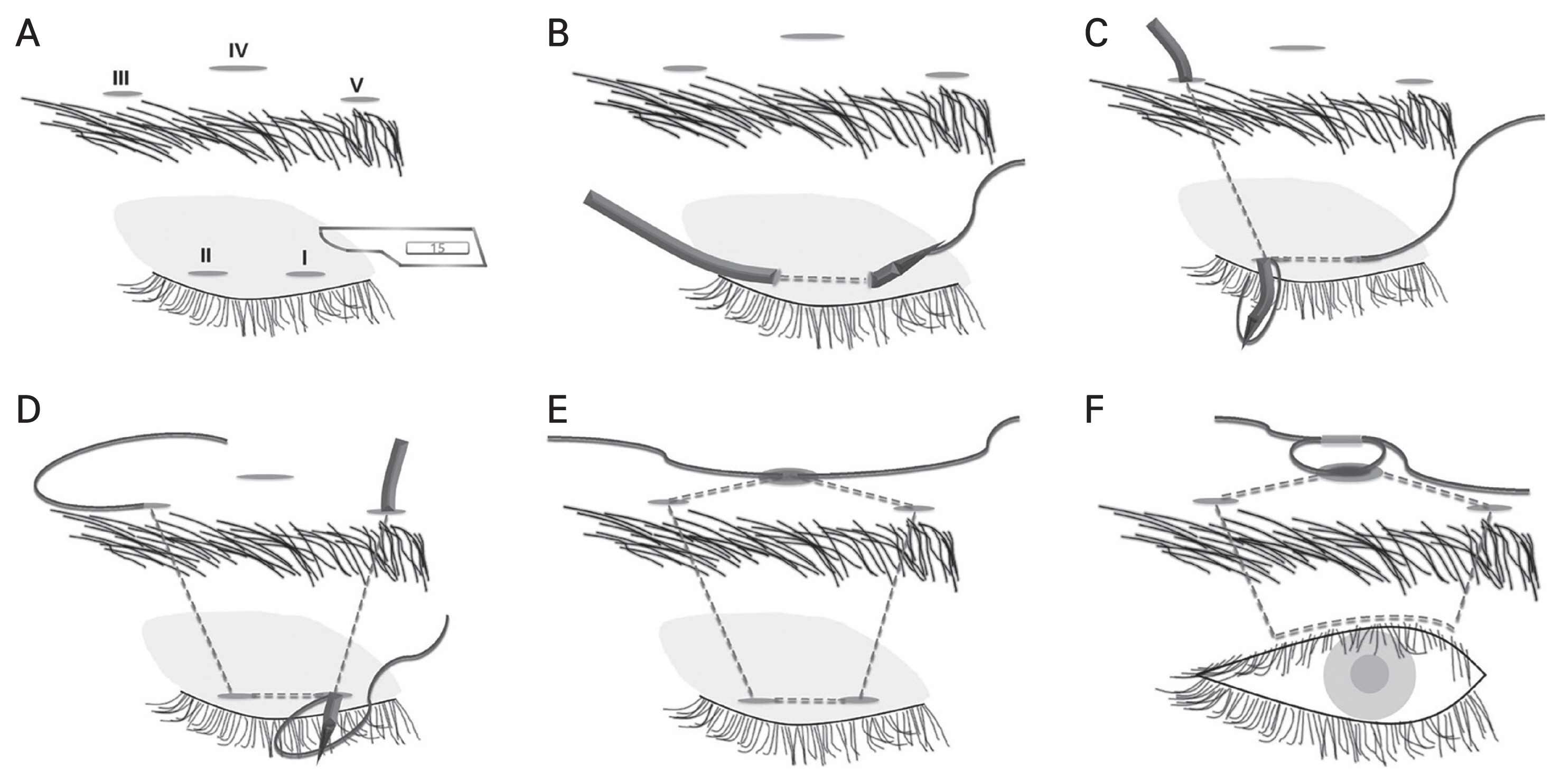
Almost all patients achieved satisfactory eyelid height and contour after the frontalis sling operation with a silicone rod (Fig. 3A, 3B). In assessments of postoperative corneal status, 15 eyes (62.5%) were categorized as grade 1, five (20.8%) as grade 2, and four (16.7%) as grade 3 (Table 3). The four eyes of three patients with grade 3 corneal status maintained their corneal condition through medical treatment fairly well but underwent a sling loosening surgery because of difficulty in visiting our clinic regularly. No patients showed grade 4 corneal condition. The MRDs of the four eyes with grade 3 corneal status were +2.0, +1.0, 0, and 0 mm at the last follow-up. There was no significant association between postoperative MRD and corneal status (Kruskal-Wallis test, p = 0.332). The degree of Bell’s phenomenon and postoperative corneal status did not show a significant correlation either (linear-by-linear association, p = 0.228).
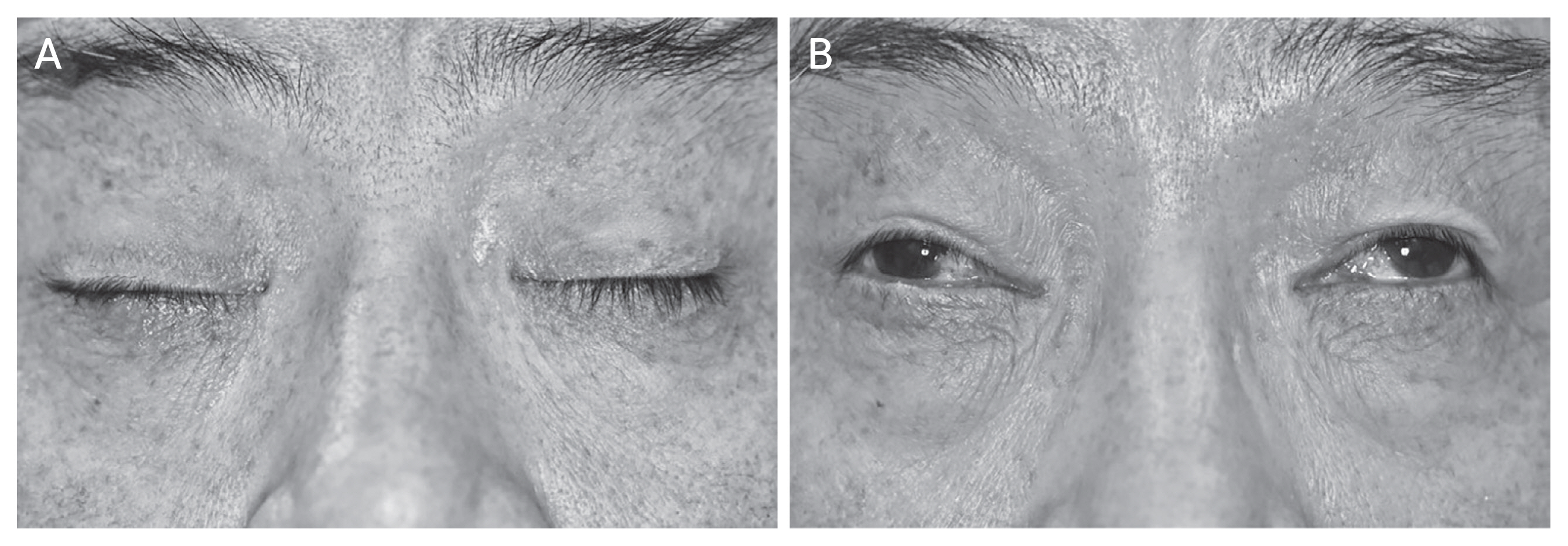
A 59-year-old male patient with bilateral severe ptosis due to third nerve palsy. (A) Preoperative feature with a margin reflex distance of −6 / −6. (B) Twenty-nine months after bilateral sling surgery, with a margin reflex distance of +2 / +2. The patient was recommended for additional strabismus surgery. The patient provided informed consent for publication of the images.
In a comparison of congenital and acquired 3rdNP, the mean preoperative MRD was not different between the two groups (−2.7 mm in congenital 3rdNP and −2.5 mm in acquired 3rdNP; Mann-Whitney U-test, p = 0.907), and the degrees of Bell’s phenomenon were not different either (linear-by-linear association, p = 0.189). As for preoperative levator function, the congenital group showed poorer function than the acquired group (1.0 mm in the congenital group and 3.5 mm in the acquired group, linear-by-linear association, p = 0.019). However, surgical outcomes, including postoperative MRD and corneal status, were not different between the two groups (Mann-Whitney U-test, p = 0.726; linear-by-linear association, p = 0.091, respectively).
Discussion
We found that the frontalis sling operation using a silicone rod successfully treated ptosis with 3rdNP. Although poor Bell’s phenomenon was very common, the postoperative corneal condition was good enough to be controlled medically.
Oculomotor palsy is a relatively common clinical diagnosis that mainly presents with diplopia and ptosis. 3rdNP can be congenital or acquired and the etiology of this disease is variable and complex. Many conditions have been reported to cause 3rdNP, such as trauma, aneurysms, pituitary tumors, cavernous sinus fistula, infarction, inflammation, infection, cavernous sinus thrombosis, and subarachnoid hemorrhage [12,13]. In our study, five patients were diagnosed with congenital 3rdNP and 13 with the acquired form. Despite the more severe ptosis (mean MRD, −2.7 vs. −2.5 mm) and poorer preoperative levator function (1.0 vs. 3.5 mm) in congenital 3rdNP, surgical outcomes in congenital 3rdNP were not significantly different from those in acquired 3rdNP in terms of eyelid height and corneal condition. This suggests that congenital 3rdNP can also be successfully managed with a frontalis sling operation with a silicone rod, even though ptosis was severe and levator function was poor in congenital 3rdNP cases.
The third cranial nerve originates from the nucleus in the midbrain and divides into the superior and inferior branches across the cavernous sinus before entering the orbit. The superior branch innervates the levator muscle and superior rectus muscle, and the inferior branch innervates the inferior rectus muscle, inferior oblique muscle, and medial rectus muscle [14,15]. 3rdNP can occur due to damage to any part of the pathway between the oculomotor nucleus in the midbrain and the extraocular muscles within the orbit [12,16]. Ptosis in the 3rdNP occurs due to damage to the superior branch of the third cranial nerve; hence, deterioration of superior rectus muscle function is frequently observed. In our study, all the patients showed various degrees of strabismus, and 15 (83.3%) underwent strabismus surgery simultaneously or sequentially.
The method used for correcting ptosis depends on the patient’s age, the cause and extent of the ptosis, the function of the levator muscle, the corneal perception state, and the presence or absence of Bell’s phenomenon. Among these factors, the function of the levator muscle has the most important effect on the decision regarding surgical options [17]. The consensus for ptosis surgery recommends levator advancement when the levator function exceeds 10 mm, levator resection for levator function of 6 to 10 mm, and frontalis sling surgery for levator function of 4 to 5 mm or less [18,19]. Postsurgical corneal problems have been a major concern for ophthalmologists. Moreover, in patients with 3rdNP, the Bell’s phenomenon is often poor due to eye movement limitations; hence, the decision to perform sling surgery is somewhat risky.
Fortunately, frontalis sling operations performed using a silicone rod can effectively raise the ptotic eyelid while preserving eyelid closure function [20]. Many doctors have reported favorable results for this suspension material. Carter et al. [4] used silicone rods in 61 eyes of 35 patients and achieved good eyelid height. Only nine eyes (15%) with an absent or inadequate Bell’s phenomenon showed postoperative exposure keratitis, which was well controlled medically. Bernardini et al. [21] performed surgery using silicone rods in 16 eyes of 10 patients and obtained satisfactory eyelid height. Only one patient (10%) with absent Bell’s phenomenon required additional surgery to manage corneal complications.
Various materials other than silicone have been used in frontalis sling surgery. Autologous fascia lata [22–24] has been used for over 100 years and remains one of the preferred materials. However, in young children, it is not easy to obtain autologous fascia lata; additional surgery is required on the leg, and scars may remain. To overcome these limitations, banked fascia lata has also been used. However, the recurrence rate with banked fascia lata is higher than that with autologous fascia lata, and there is a risk of infection [25]. Several synthetic materials such as polypropylene and nylon have been used for temporary suspension, but they may be associated with high recurrence rates [26]. In this study, we chose silicone rods as a suspension material in all patients for many reasons. First, the silicone rods exhibit excellent elasticity, allowing patients to close their upper eyelids with greater ease while maintaining good eyelid height [4]. Second, the silicone rods have superior adjustability. The rods are not incorporated into the surrounding tissues and allow easy adjustment of eyelid height after the surgery [5,27]. Third, the silicone rods have a long shelf life and are less susceptible to infection.
Special emphasis on the cornea
In many articles dealing with frontalis sling surgery [8–11], the primary outcome is the functional and cosmetic results involving eyelid contour, eyelid height, and symmetry. They also described possible postoperative complications, such as exposure keratopathy or lagophthalmos, suture granuloma, eyelid edema, entropion, wound infection, and so on. Among them, complications related to the cornea can be vision-threatening and very critical. Under normal conditions, the eye is well equipped with natural defense mechanisms to protect the ocular surface, especially the cornea [28]. The eyelids provide a physical barrier to dryness and trauma and prevent adherence of microorganisms to the ocular surface [29]. If this important barrier collapses due to incomplete eyelid closure after frontalis sling surgery, corneal erosion or severe exposure keratitis may occur. On the basis of this importance, we intended to assess the postoperative status of cornea as one of the main outcomes. The corneal condition after surgery, which means safety outcome, was classified into four grades. Twenty eyes out of 24 (83.3%) showed minimal corneal erosions (grade I) or mild erosions (grade II) in our study. Considering the majority of our subjects had poor Bell’s phenomenon, this result is fairly good. It can be hypothesized that because the probability of developing lagophthalmos is lowered due to the elasticity of silicone rods, corneal erosion is less likely to occur after surgery. A further comparative study with other sling materials is needed to verify this.
Cosmesis versus safety
The guidelines for desirable eyelid height after frontalis sling operation vary from study to study. Ho et al. [11] defined an excellent eyelid height as postoperative MRD of 3 mm or more. Dave et al. [30] reported that a favorable outcome was defined as MRD of 4 mm in bilateral cases. However, no studies have investigated the stability of the cornea according to the eyelid height. Postoperative eyelid cosmesis and corneal safety are like the ends of a seesaw; if the surgeon places too much emphasis on one aspect, it can lead to disappointing results in the other. Therefore, determining the ideal eyelid height to balance corneal safety and desirable cosmetic result is essential, especially in subjects with poor Bell’s phenomenon. We thus sought to determine a safe upper limit of eyelid height for the postoperative cornea. However, the correlation between the postoperative MRD value and the postoperative corneal grade was not significant (Kruskal-Wallis test, p = 0.332). This may imply that the corneal condition may be affected not only by MRD, but also by other factors such as tear film condition, elasticity of eyelids, and compliance with eye drops application. In other words, the corneal status may not be influenced by MRD alone. Although this study could not statistically reveal the safe eyelid height for the cornea, both cosmetic and safety outcomes were achieved in all subjects. We hope that our investigation will be a cornerstone for future ophthalmologic studies to find out the optimum eyelid height.
In conclusion, to the best of our knowledge, this is the largest series to report outcomes of frontalis sling surgery using a silicone rod in third nerve palsy. This study suggests a new method to define the postoperative safety outcome by specially focusing on categorized corneal status. Frontalis sling surgery using a silicone rod can effectively and safely correct ptosis in 3rdNP patients without severe corneal complications despite poor Bell’s phenomenon. This finding can be helpful for surgical planning and counseling patients. The limitations of the current study include its retrospective nature, small sample size, and lack of a control group. Prospective large-scale studies are warranted to clarify the safety of frontalis sling surgery using a silicone rod in 3rdNP patients, and to find out the value of eyelid height safe for the cornea.
Acknowledgements
None.
Notes
Conflicts of Interest
None.
Funding
None.