Epiretinal Proliferation Associated with Lamellar Hole or Macular Hole: Origin and Surgical Prognosis
Article information
Abstract
Purpose
To determine the origin of epiretinal proliferation (EP), a condition that is occasionally observed in lamellar hole and macular hole cases, and EP outcomes after vitrectomy.
Methods
This is a retrospective observational case review of 17 eyes with EP that underwent vitrectomy, EP dissection, and internal limiting membrane peeling between January 2013 and December 2016. Surgical specimens of EP tissue were successfully obtained from 5 cases and they were analyzed after immunohistochemical staining. Postoperative outcomes, including best-corrected visual acuity (BCVA) and macular configuration in spectral domain-optical coherence tomography, were reviewed.
Results
Mean BCVA improved from 0.54 ± 0.36 logarithms of the minimum angle of resolution preoperatively to 0.32 ± 0.38 logarithms of the minimum angle of resolution postoperatively (p = 0.002). BCVA improved in 13 eyes and remained unchanged in four eyes. No cases experienced vision decline after surgery. All 17 patients' lamellar hole or macular hole were successfully closed. Despite hole closure, ellipsoid zone defects were not corrected in 11 of the 17 patients. In immunohistochemical analyses, anti-glial fibrillary acidic protein and pan-keratin (AE1/AE3) were positive, but synaptophysin, anti-α-smooth muscle actin, and anti-CD68 were negative.
Conclusions
The epiretinal proliferative membrane seems to originate from Müller cells, not from the vitreous. It is unclear whether retinal pigment epithelia also contribute to EP formation. Gentle handling and preservation of the epiretinal proliferative tissue is crucial for successful surgical outcomes.
Epiretinal proliferation (EP) is a disease that has only recently become widely known, due to advancements in retinal imaging equipment [123456789]. EP has different features from conventional epiretinal membrane (ERM), and is referred to as thick ERM, dense ERM, or lamellar hole (LH)-associated EP [237]. Apart from tractional LH, it is also called degenerative LH [10]. Lai et al. [11] proposed “macular defect associated EP” as a more inclusive term, on the basis that EP is found, not only in LH cases, but also in macular hole (MH) cases. We also previously proposed the term “EP associated with macular hole or lamellar MH” [12]. However, because EP is occasionally found in extramacular areas, our term also does not encompass all cases [7].
Despite a growing literature around EP, its pathogenesis, origin, and post-surgery clinical outcomes are not fully understood [39111314]. The natural course of EP is relatively stable [57]. In some cases, however, EP can be morphologically and functionally exacerbated, or it can be found in associated cases of full-thickness MH (FTMH) or impending MH (I-MH). These cases are subject to surgery, but there is a disagreement about post-surgical prognosis [1114].
Histological studies also disagree about the origin of this unusual tissue [9121315]. Compera et al. [9] and Compera et al. [13] suspected its origin to be the vitreous, because they found that myofibroblasts with contractive properties are predominant in conventional ERM cells, whereas EP cells had hyalocytes, fibroblasts, and glial cells without contractive properties. Also, they observed vitreous collagen strands in EP tissue through an electron microscope. These findings indicated that EP originates from the vitreous. On the other hand, Pang et al. [15] claims that EP pathogenesis may involve a Müller-cell-driven process that originates from the inner retinal layers during LH development. We previously suggested that the retinal pigment epithelial (RPE) cells might contribute to EP [12].
The purpose of this study was to broaden the understanding of EP origin, surgical outcomes, and prognosis based on surgical reviews and histological studies.
Materials and Methods
Patients
Twenty patients diagnosed with EP using spectral-domain optical coherence tomography (SD-OCT) underwent pars plana vitrectomy, EP dissection, and internal limiting membrane (ILM) peeling by a single surgeon (JS) between January 2013 and December 2016. All patients were followed for over 6 months. Among the 20 patients, 3 were excluded from analyses because they had severe concurrent ocular diseases: one had age-related macular degeneration, one had proliferative diabetic retinopathy, and one had advanced glaucoma. All patients were recommended to undergo surgery according to the following indication criteria: (1) an association with FTMH or I-MH, (2) progression to MH during follow-up, (3) best-corrected visual acuity (BCVA) decreased below 2 or more logarithms of the minimum angle of resolution (logMAR) lines during follow-up, and (4) presence of disturbing metamorphopsia. Informed consent was obtained from all 17 EP associated with macular hole or lamellar MH patients. This study was approved by the institutional review board of HanGil Eye Hospital (HanGil IRB-15002). Informed consent was obtained from all 17 patients, and it adhered to the tenets of the Declaration of Helsinki.
Surgical procedures
A single surgeon (JS) performed 23-gauge pars plana vitrectomy in all patients. If cataracts were also present, cataract surgery was also performed. Concurrent ERM was carefully removed using retinal forceps. Yellowish tissue that was diagnosed as EP during preoperative OCT was carefully separated from the underlying retina using a soft-tip cannula or ILM forceps but was not removed from the MH margin. When peeling the tissue, a crown-like structure appeared around the fovea. We previously named this structure “perifoveal crown tissue” [12].
Indocyanine green (0.125%, 1.25 mg/mL; Dianogreen Injection, Daiichi Pharmaceutical, Tokyo, Japan)-assisted ILM peeling was performed in all patients. Redundant perifoveal proliferative tissue was trimmed with microscissors, leaving some remaining tissue at the fovea margin. Sufficient epiretinal proliferative tissue was obtained from 5 patients with retinal scissors for histological analysis. Perfluoropropane (C3F8) gas tamponade was performed in seven patients, while air tamponade was performed in the other ten patients. All surgeries were completed without any complications.
Visual acuity and macular configuration follow-up
Visual acuity and macular configuration were measured throughout the 17 patients' follow-up visits. BCVA was measured in logMAR units. Macular configuration was recorded at every visit using SD-OCT (Cirrus, Carl Zeiss Meditec, Dublin, CA, USA; or Spectralis, Heidelberg Engineering, Heidelberg, Germany). Volumes of B-scan images were extracted from Heidelberg Viewer Module 5.6.4 (Heidelberg Engineering) and saved in JPG files. The saved images were analyzed by two physicians (YY and GS) and confirmed by a senior grader (JS). Changes in ellipsoidal zone defects and hole configuration after surgery were analyzed.
Specimen preparation
Special care was taken to remove only the yellowish epiretinal proliferative tissue. Each tissue specimen was fixed in 10% buffered formalin and sent for histological analysis [1]. Each tissue was then embedded in paraffin and stained with H&E. Automated immunocytochemical staining was performed using the Bond-max system (Leica Microsystems, Bannockburn, IL, USA). All steps were performed using the manufacturer's instructions in the following order: deparaffinization; heat-induced epitope retrieval (antigen unmasking); peroxide block; incubation with primary antibodies for the following: synaptophysin (1:400, SY38; DAKO, Carpinteria, CA, USA), pan-keratin (1:100, AE1/AE3; Novocastra, Newcastle, UK), α-smooth muscle actin (SMA; 1:200, 1A4, DAKO), CD68 (1:500, KP-1, DAKO), and glial fibrillary acidic protein (GFAP; 1:400, 6F2, DAKO); color development with 3,3'-diaminobenzidine tetrahydrochloride chromogen; hematoxylin counterstaining; and slide mounting. Normal human serum served as a negative control. Samples were considered to be positive for synaptophysin and pan-keratin if they exhibited any degree of cytoplasmic staining. For photodocumentation of the specimens, we used a digital camera at 200x magnification (E1000; Nikon, Tokyo, Japan). Synaptophysin was used to mark cells of neuronal origin, pan-keratin for cells of epithelial origin, α-SMA for myofibroblasts, CD68 for macrophages/microglia cells, and GFAP for glial cells.
Results
Demographics
The mean age of the 17 patients was 64.41 ± 8.78 years, including six men and eleven women. Twelve patients had MH (eight with FTMH and four with I-MH), and five patients had LH (Table 1). Nine patients were phakic, and the other eight were pseudophakic. Signs of mild non-proliferative diabetic retinopathy were observed in four patients, but none were complicated by diabetic macular edema.
Visual acuity and macular configuration
Postoperative outcomes for 17 patients, including BCVA and macular configuration, were reviewed (Table 2). The patient follow-up period ranged from 6 to 46 months, with a mean duration of 22.4 ± 13.9 months. BCVA improved in 13 eyes (decrease ≥0.3 logMAR in 8 eyes, decrease 0.1–0.2 logMAR in 5 eyes), and remained unchanged in 4 eyes. No cases experienced vision decline after surgery. Mean BCVA improved from 0.54 ± 0.36 logMAR, preoperatively, to 0.32 ± 0.38 logMAR, postoperatively (p = 0.002, Wilcoxon signed-rank test) (Fig. 1).
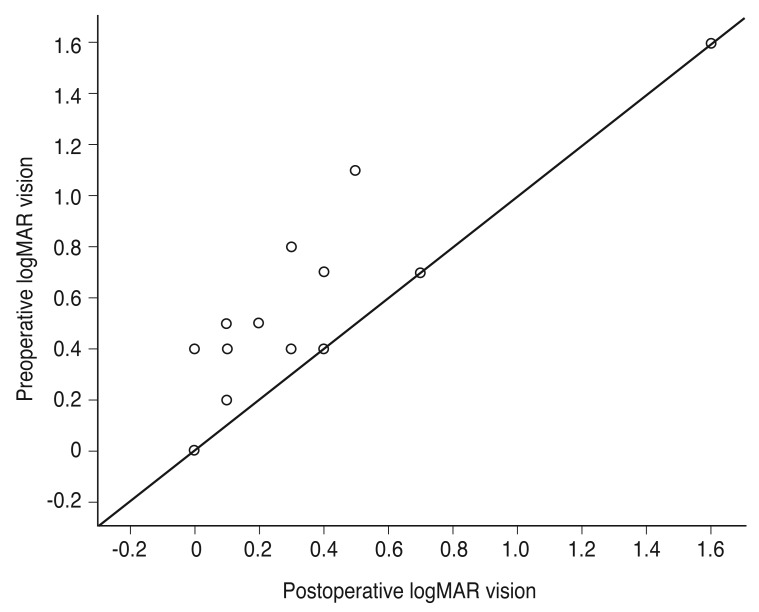
Logarithm of the minimum angle of resolution (logMAR) visual results after in patient with epiretinal proliferation associated with lamellar hole or macular hole.
The LHs and MHs of all 17 patients were successfully closed; however, ellipsoid zone defects were only corrected in six patients. Nevertheless, BCVA improved despite ellipsoid zone defects (Fig. 2A–2F).
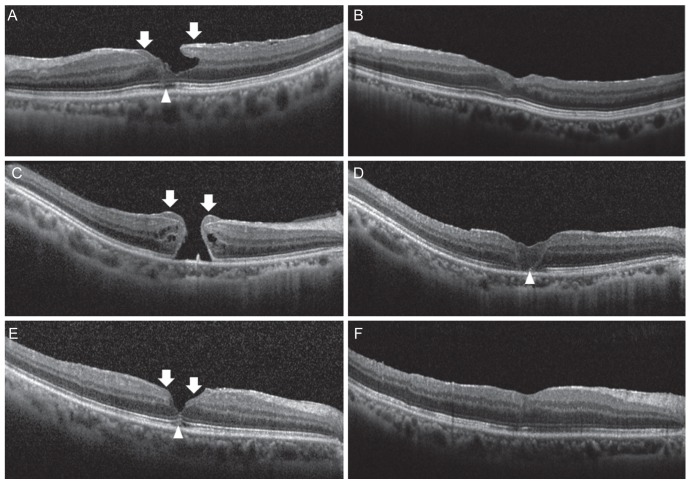
(A,B) Preoperative and postoperative optical coherence tomographic (OCT) images of lamellar hole (patient 15), (C,D) full-thickness macular hole (FTMH) (patient 14), and (E,F) impending macular hole (I-MH) (patient 10) with epiretinal proliferation (EP). (A) Preoperative OCT scan shows lamellar hole with EP (arrows) and ellipsoidal zone defect (arrowhead). (B) Postoperative OCT scan (6 months after surgery) shows closed lamellar hole and ellipsoidal zone defect restored. (C) Preoperative OCT scan shows FTMH with EP (arrows). (D) Postoperative OCT scan (3 months after surgery) shows closed FTMH and ellipsoidal zone defect (arrowhead) remained. (E) Preoperative OCT scan shows I-MH with EP (arrows) and ellipsoidal zone defect (arrowhead). (F) Postoperative OCT scan (3 months after surgery) shows closed I-MH and ellipsoidal zone defect restored.
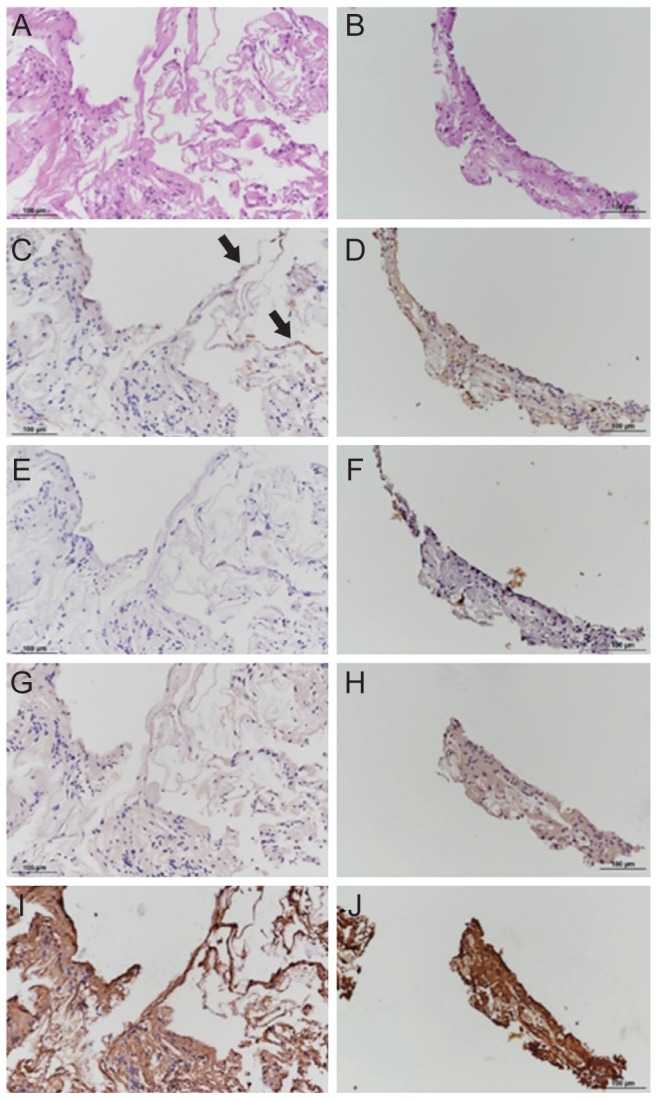
Histological assessment
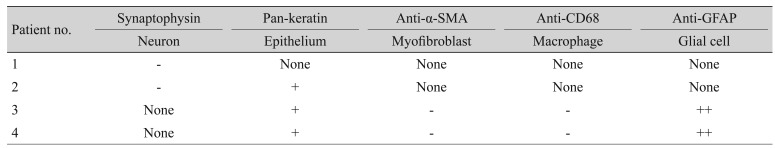
Histological analysis was attempted on five tissue samples (patients 1 to 5), but one (patient 5) was not suitable for analysis. On the analyzable samples, we performed H&E staining. For immunohistochemical analyses, synaptophysin was used for neuronal cells (patients 1 and 2), pan-keratin for epithelial cells (patients 2 to 4), anti-α-SMA for myofibroblasts (patients 3 and 4), anti-CD68 for macrophages/microglia cells (patients 3 and 4), and anti-GFAP for glial cells (patients 3 and 4) (Table 3). For H&E staining, all tissues showed lymphocyte aggregations and cells with medium-density nuclei. Hyalocytes and fibroblasts were not observed. In immunohistochemical staining, specimens reacted negatively to synaptophysin, anti-α-SMA, and anti-CD68, while they reacted positively to pan-keratin antibody and anti-GFAP (Fig. 3A–3J).
Histopathological analysis of epiertinal proliferation tissue. (A,B) Hematoxylin and eosin staining of epiretinal proliferative tissue (×400). Aggregation of lymphocytes and cells with medium-density nucleus are scattered. There were no hyalocytes and fibroblasts identified. (C,D) Pan-keratin staining of epiretinal proliferative tissue (×100). Note cells with brownish-stained cytoplasm (arrows) scattered throughout the specimen. (E,F) Actin staining of epiretinal proliferative tissue (×200). No specific staining is observed. (G,H) Anti-CD68 staining of epiretinal proliferative tissue (×500). No specific staining is observed. (I,J) Anti-glial fibrillary acidic protein staining of epiretinal proliferative tissue (×400). Strong positive staining all around the specimen is observed. Epiretinal proliferation tissue acquired from patient 3 (A,C,E,G,I) and patient 4 (B,D,F,H,J).
Discussion
EP is now accepted as a distinct clinical entity from conventional ERM [7]. It was previously reported that eyes with LH-associated EP had significantly poorer BCVA compared with eyes without LH-associated EP [678]. This might be due to ellipsoidal zone defects, which are frequently found in eyes with EP [6810].
More than 90% of eyes with EP were reported to be morphologically stable without surgical intervention, such as with conventional LH cases [57]. However, surgical treatment is required for exacerbated cases or cases associated with FTMH. The surgical indications for EP have been presented in several studies, which are, in summary: (1) association with FTMH or I-MH, (2) progression to MH, (3) OCT changes (decrease in foveal thickness or increase in LH diameter) where BCVA decreased 2 logMAR lines or more, and (4) disturbing metamorphopsia [35916].
Previous studies of the postoperative prognosis of EP have been controversial [111416]. Postoperative BCVA is affected by various factors, such as preoperative BCVA, concomitant cataract surgery, and surgical procedure. Lai et al. [11] found no difference in postoperative visual prognosis between LH patient groups with and without EP. Conversely, Ko et al. [14] reported that LH-associated EP showed no visual benefit after surgery, despite anatomical improvement. These opposing results may have been affected by the different surgical procedures performed in the studies. Shiraga et al. [17] suggested that preserving the “thick ERM with macular pigment,” yields better clinical outcomes than removing it. We also believe that poor postoperative BCVA is associated with meticulous peeling or removing of the epiretinal proliferative tissue.
In this study, mean BCVA improved significantly after vitrectomy. Postoperative BCVA improved in 13 cases and remained unchanged in 4 cases. Three of the four eyes with no BCVA improvement were cases with FTMH or I-MH, and the remaining one was a case with LH. The LH patient who showed no visual improvement was preoperatively revealed to have a large ellipsoid zone defect on SD-OCT.
The yellowish pigment-rich epiretinal proliferative tissue seems to be connected to the outer and middle layers of the retina [12]. Thus, removing the epiretinal proliferative tissue may lead to FTMH development [237]. Removing the epiretinal proliferative tissue would be, metaphorically, like pulling the central plug out of the structurally compromised macula [7]. We recommend that the epiretinal proliferative tissue not be removed meticulously. Rather, in our experience, the epiretinal proliferative tissue should be dissected gently, working from the outside to the edge of the hole. Microscissors or a vitrectomy cutter with very low suction can be used to trim the adherent epiretinal proliferative tissue around the hole margin, but it is better to preserve the epiretinal proliferative tissue as much as possible. Gentle handling of this tissue is very important.
There have been various attempts to determine the origin of this unusual EP. However, there is debate about whether the origin of epiretinal proliferative tissue is the vitreous, RPE cells, or Müller cells [379121315]. Parolini et al. [3] suspected the vitreous to be the origin. They suggested premacular vitreous remodeling as a potential causative mechanism, and they presented positive staining results of hyalocyte markers (CD45 and CD64) on epiretinal proliferative tissue as histological evidence. Although they reported a few positive staining results for epiretinal proliferative tissue and cellular retinaldehyde binding protein, which targets both RPE cells and glial cells, they suspected hyalocytes as the EP origin. Compera et al. [9] and Compera et al. [13] reached a similar conclusion, however, they performed epiretinal proliferative tissue fixation without completely differentiating the ILM. ILM specimens are composed of a variety of cells, including hyalocytes, glial cells, RPE, fibrocytes, and myofibrocytes [181920]. We previously suggested that epiretinal proliferative tissue could be the result of RPE proliferation that migrated through ellipsoid zone defects [12]. Based on an SD-OCT anatomical assessment, Pang et al. [7] hypothesized that there is a possibility that Müller cell proliferation is the origin of epiretinal proliferative tissue. They suggested that RPE cells could also propagate by migrating through the neuroretinal tissue; however, they concluded that a Müller cell-driven response is more likely for several reasons. Recently, Pang et al. [15] obtained a very pure patient sample of epiretinal proliferative tissue that reacted positively to anti-GFAP and anti-glutamine synthetase. They suggested that the epiretinal proliferative tissue must have originated from a Müller cell, because glutamine synthetase is a Müller cell-specific enzyme in the retina.
In our histological study, we obtained four epiretinal proliferative tissue samples suitable for histological analysis. We had harvested only a portion of the yellowish pigment-rich tissue when we noted dehiscence within the fluttering epiretinal proliferative tissue. Since tissue acquisition was performed after indocyanine green-assisted ILM peeling, there should have been a lower risk of target tissue contamination with the ILM components. Our tissue specimens showed positive reactions to GFAP and pan-keratin (AE1/AE3) antibodies, but negative reactions to smooth muscle actin and anti-CD68. GFAP has been used as a universal marker of Müller cell gliosis [212223]. These results indicate that Müller cell proliferation plays an important role in EP development. Pan-keratin (AE1/AE3) antibody shows a positive reaction in RPE cells but may also elicit a positive reaction in active glial cells, such as Müller cells [24]. Positive reactions with GFAP and pan-keratin (AE1/AE3) antibodies supports the hypothesis that epiretinal proliferative tissue originated from retinal glial cells, specifically Müller cells. However, it is unclear whether RPE is involved in EP formation because positive staining results for pan-keratin (AE1/AE3) antibodies do not absolutely confirm an RPE cell contribution. More specific immunohistochemical staining that targets RPE is needed.
This study has several limitations, mainly because of the small sample number and retrospective review design at a single institute. A sample of 17 patients is insufficient to establish statistical significance for surgical prognosis. However, details of the surgical procedure and follow-up protocol were standardized because all the surgeries were performed by a single surgeon. Additionally, pan-keratin (AE1/AE3) immunohistochemical staining targeting RPE cells was not sufficient to confirm the existence of RPE cells within the specimens.
In conclusion, the epiretinal proliferative membrane seems to originate from Müller cells, not from the vitreous. It is unclear whether retinal pigment epithelium also contributes to EP formation. Gentle handling and preservation of the epiretinal proliferative tissue is very important for improving surgical outcomes for EP.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.