Patient Awareness of Cataract and Age-related Macular Degeneration among the Korean Elderly: A Population-based Study
Article information
Abstract
Purpose
Age-related eye disease is often considered part of natural aging. Lack of awareness of eye conditions can result in missed treatment. We investigated the rates of awareness of cataract and age-related macular degeneration, the most common age-related eye-diseases, and the associated factors among elderly Koreans.
Methods
We identified 7,403 study subjects (≥40 years old) with cataract or age-related macular degeneration based on ophthalmic examination results during the 5th Korean National Health and Nutrition Examination Survey conducted between 2010 and 2012. We assessed whether patients were aware of their eye condition based on a previous diagnosis by a physician.
Results
The average awareness rate over the 3-year study period was 23.69% in subjects with cataract and 1.45% in subjects with age-related macular degeneration. Logistic regression analysis showed that patients with cataract were more likely to recognize their condition if they had myopia (odds ratio, 2.08), hyperopia (odds ratio, 1.33), family history of eye disease (odds ratio, 1.44), or a past eye examination (odds ratio, 4.07-29.10). The presence of diabetes mellitus was also a significant predictor of patient awareness of cataract (odds ratio, 1.88).
Conclusions
Poor patient recognition of eye disease among the Korean elderly highlights the seriousness of this potential public health problem in our aging society. Pre-existing eye-related conditions and diabetes were significant predictors of awareness; therefore, patients in frequent contact with their doctors have a greater chance of detecting eye disease.
Eye diseases are some of the most easily overlooked illnesses and can have a significant impact on the quality of life of the elderly [12]. Two major age-related eye diseases (AREDs) known to cause blindness worldwide are cataract and age-related macular degeneration (AMD) [3]. ARED-induced visual disabilities reduce health-related quality of life in the elderly; people with ARED have significantly higher levels of mental distress than those without ARED (relative risk, 1.4; 95% confidence interval [CI], 1.27 to 1.54) [2]. Furthermore, visual disability-related comorbidities include depression and femur fracture [4567].
Many people do not recognize the necessity and importance of maintaining eye health; instead, ARED is often considered a part of natural aging. Lack of awareness and interest in eye conditions can result in delayed or missed treatment [89]. Eye diseases, similar to chronic conditions such as diabetes or hypertension, are usually asymptomatic in the early stages, until the disease has progressed. However, while diabetes and hypertension are monitored regularly, eye diseases are generally ignored, resulting in large proportions of patients who are unaware of their status. In a study conducted in Singapore, 80% of patients with common eye diseases were unaware of their condition [10].
According to the 2012 Korean National Health and Nutrition Examination Survey (KNHANES), approximately 94% and 16% of people aged ≥70 years had cataract and AMD, respectively [11]. The 2011 Korean National Health Insurance statistical report showed that cataract and lens defects were the leading causes of hospitalization and treatment [12]. Therefore, eye diseases are common in the elderly and are responsible for considerable health care expenditure. Patients with moderate vision loss, severe vision loss, or blindness are estimated to have higher adjusted mean eye-related costs (345, 407, or 237 US dollars/yr, respectively) and non-eye related costs (2,193, 3,301, or 4,443 US dollars/yr, respectively) than those with normal vision [7].
To prevent avoidable vision loss, patients need to be aware of their eye condition and receive appropriate treatment. U nfortunately, r esearch on the level of A RED awareness and factors influencing awareness among the elderly, including those in Korea, is limited. This study examines the extent to which elderly people with ARED in Korea are aware of their eye condition. Specifically, we used national representative data from the KNHANES between 2010 and 2012 to estimate the gap between prevalence and awareness of the two most common AREDs (i.e., cataract and AMD). Furthermore, factors accounting for the awareness gap pertaining to cataract were investigated in order to suggest effective strategies for reducing this gap in our aging society.
Materials and Methods
Data source and study population
Data were obtained from the 5th KNHANES, covering 2010 to 2012. This is a nationally representative, stratified, multistage sampling, cross-sectional survey comprising three parts: health interview, health examination, and nutrition surveys. KNHANES has been conducted by the Korean Centers for Disease Control and Prevention since 1998. The sampled population for KNHANES is non-institutionalized civilians aged ≥1 year. Details regarding the KNHANES survey design and methods are provided elsewhere [1314].
This study included 7,403 individuals aged ≥40 years who had a cataract or AMD in either eye, as extracted from KNHANES ophthalmic examinations of 25,533 participants. Since we consider early diagnosis of ARED important, we included both middle-aged and elderly individuals in our study. To assess AMD in the KNHANES ophthalmic examination, a 45° digital fundus photograph of both eyes was obtained under physiological mydriasis and graded using the international AMD classification and grading system [15]. The presence of cataract was defined as ≥1 type of lens opacity or evidence of cataract extraction in either eye. Lens opacities were assessed using the Lens Opacities Classification System (LOCUS) III scores: cortical (LOCUS III score ≥2), nuclear (LOCUS III score ≥4), posterior subcapsular (LOCUS III score ≥2), and mixed cataracts (>1 type per eye) [1617]. The quality of the ophthalmic surveys, fundus photograph readings, and cataract evaluations were verified by the Epidemiologic Survey Committee of the Korean Ophthalmologic Society [1819].
Variables
For each patient group (cataract or AMD), we determined the individual's awareness of their eye condition based on the answer to the following question: Have you ever been diagnosed by a physician with a cataract (or AMD) in either eye? If the respondent answered “yes,” the person was assumed to be aware of their eye disease.
We employed Andersen's behavioral model to select variables explaining the awareness of ARED [202122]. Andersen's model provides a conceptual framework for analyzing various factors influencing an individual's health care use, including predisposing, enabling, and need factors. Predisposing factors were sex, age, educational level, marital status, and residential area (urban or rural).
Family income level, type of health security program, and supplementary health insurance were included in the model as enabling factors. Family income level was classified as quartiles of average monthly household income. The type of health security program was either National Health Insurance (NHI) or Medical Aid (MA), the two tiers of the universal health insurance system in Korea. The NHI program is a wage-based, contributory insurance program covering approximately 96% of the population, and the MA program is a government-subsidized public assistance program for poor and medically indigent individuals. In an earlier study, patients enrolled in MA tended to have higher health care utilization than those in NHI with the same condition [23]. We therefore assumed that people in the MA program would have greater awareness of their eye condition than those in the NHI program. Regarding supplementary private health insurance, it was assumed that the availability of an additional financing source for health care services has a positive effect on health care utilization, facilitating recognition of an eye disease.
Need factors were used to measure eye-specific and overall health status. We hypothesized that individuals with poor health status were more likely to visit health care providers and consequently had a higher chance of having their eye diseases detected. To describe eye-specific health status, we included the occurrence of visual disturbance, myopia, hyperopia, astigmatism, previous eye surgery, and family history of eye disease. We also measured the degree of exposure to eye examinations, defined as the time since the most recent eye examination. In a previous study, the extent of sunlight exposure was identified as a risk factor for eye disease [24]; therefore, we also included daily sunlight exposure (≥5 or <5 hours) [25]. Self-rated health status, measured using a 5-point Likert-type scale, was included to reflect overall health status. In addition, selected comorbid conditions that are prevalent in elderly Koreans, such as obesity, hypertension, and diabetes mellitus, were included to represent overall health status.
Statistical analysis
All statistical analyses were performed using SAS ver. 9.4 (SAS Institute, Cary, NC, USA), incorporating sampling weights and adjusting for the complex survey design of the KNHANES. Survey sampling weights were used to produce estimates that were representative of the non-institutionalized civilian Korean population. Chi-square tests were employed to examine differences in patient characteristics between the aware and unaware patient groups. Multivariate logistic regression analysis was used to examine factors associated with cataract awareness in patients diagnosed with cataract. For patients with AMD, it was not feasible to conduct a multivariate analysis due to the small sample size of the AMD awareness group (n = 16) (Fig. 1). Statistical significance was accepted at p < 0.05.
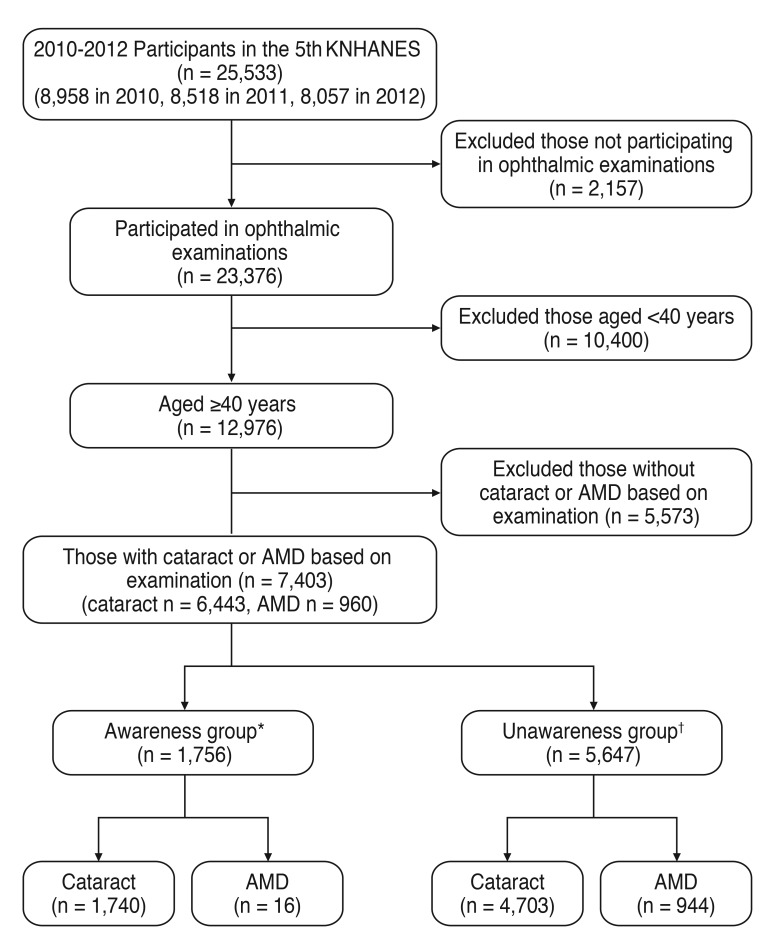
Process for identifying and including study subjects. KNHANES = Korea National Health and Nutrition Examination Survey; AMD = age-related macular degeneration. *Individuals who answered that they had been diagnosed with cataract or AMD by a physician; †Individuals who answered that they had not been diagnosed with cataract or AMD by a physician.
Results
Patient awareness of their eye disease
Among the subjects with cataract, 23.69% were aware of their eye disease (Fig. 2A). The average awareness rate of AMD was 1.45% over the 3-year study period, approximately 16.3-fold lower than the cataract awareness rate. The proportion of patients with AMD who were aware of their eye disease increased 3.4-fold over the 3 years, from 0.69% (2010) to 2.38% (2012) (Fig. 2B). In contrast, cataract awareness increased only slightly from 22.71% to 25.48%.
Factors associated with patient awareness of their eye disease
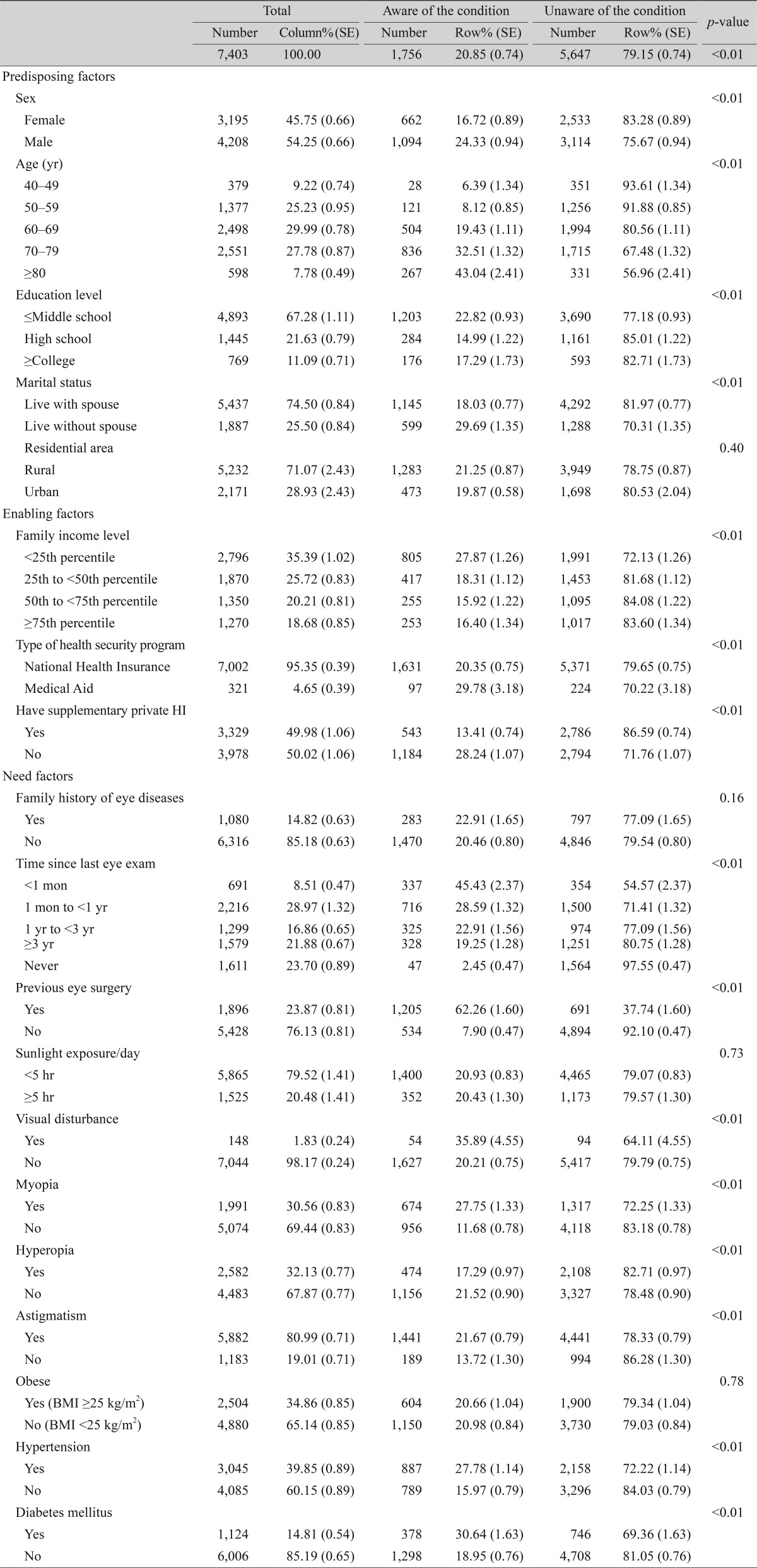
We compared the characteristics of the study subjects with either cataract or AMD according to awareness of their eye condition (Table 1). Almost all characteristics were significantly different (p < 0.05) between the aware and unaware groups. Women were 1.45-fold more aware of their eye disease (24.33%) than men (16.72%). While the prevalence of the two eye diseases was consistent across age groups (50 to 59 years, 25.23%; 60 to 69 years, 29.99%; and 70 to 79 years, 27.78%), the proportion of awareness was only 8.12% in the 50- to 59-year-old age group and increased to 32.51% for subjects aged 70 to 79 years. The lowest income group, with family income level below the 25th percentile of the national population, had a greater awareness rate (27.86%) than higher income groups (15.92% to 18.32%). Patients with chronic diseases such as hypertension (27.78%) and diabetes mellitus (30.64%) had greater awareness rates than those without these chronic diseases (15.97% and 18.95%, respectively). Patients who had undergone recent eye examinations also had greater awareness of their eye disease than those who had not. Patients with visual disturbance (35.89%), myopia (27.75%), or astigmatism (21.67%) showed greater awareness than those without these conditions (20.21%, 16.82%, and 13.72%, respectively).
The cataract or AMD subtype was considered as an important predictor of patient awareness. For cataract, awareness was approximately two-fold greater among patients with mixed types than among patients with single type (24.3% vs. 12.85%, p < 0.001) (Table 2). Awareness was approximately 24-fold greater among patients with late AMD than in those with early AMD (14.24% vs. 0.59%, p < 0.001) (Table 2). Multivariate logistic regression analysis was performed to examine the independent associations between the predisposing, enabling, and need factors and cataract awareness status (Table 3).
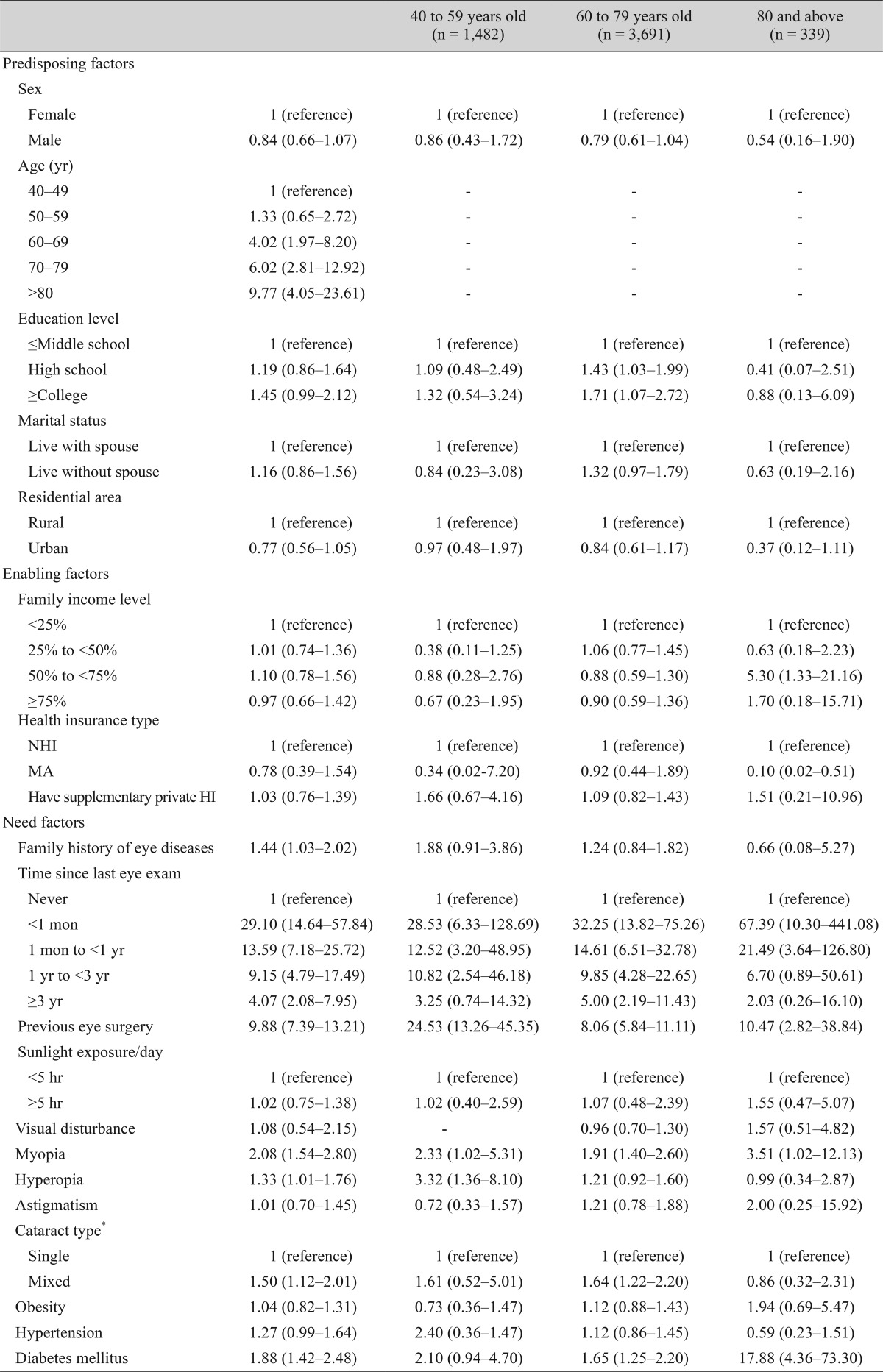
Age was the only statistically significant predictor among the predisposing factors; the probability that a person would be aware of a cataract significantly increased with age, with an odds ratio (OR) of 4.02 (95% CI, 1.97 to 8.20) in people aged 60 to 69 years and 9.77 (95% CI, 4.05 to 23.61) in those aged ≥80 years. None of the enabling factors were significant independent predictors of patient awareness of cataract. Among the need factors, most of the variables for eye-specific health status were significant predictors of awareness. Those with prior eye conditions such as myopia (OR, 2.08; 95% CI, 1.54 to 2.80), hyperopia (OR, 1.33; 95% CI, 1.01 to 1.76), or family history of eye disease (OR, 1.44; 95% CI, 1.03 to 2.02) were more likely to be aware of having a cataract. As expected, those who had undergone an eye examination in the past also had a greater chance of being aware of their cataract condition. Among the three chronic diseases, the presence of diabetes mellitus was the only significant predictor of cataract awareness (OR, 1.88; 95% CI, 1.42 to 2.48).
To examine whether predictors of patient awareness vary by patient age, we performed separate logistic regression analyses for each of the three age groups: 40 to 59, 60 to 79, and ≥80 years (Table 3). For the youngest patient group (40 to 59 years), an eye examination within the past 3 years, previous eye surgery, and history of myopia or hyperopia were significantly, positively associated with cataract awareness. For the young elderly patients (60 to 79 years), higher education level, past eye examination, previous eye surgery, mixed type of cataract, myopia, and diabetes mellitus were significant predictors of cataract awareness. Finally, for the oldest patient group (≥80 years), middle income status, an eye examination within the past year, previous eye surgery, myopia, and diabetes mellitus were significant predictors of cataract awareness.
Discussion
This study investigated the patient awareness rate of cataract or AMD and examined factors associated with these awareness rates among elderly Koreans. Although the proportion of patients with cataract or AMD who were aware of their eye disease increased during the study period (2010 to 2012), the awareness rates for both diseases were very low. Only one-fifth of the elderly population with a cataract was aware of their eye disease, based on data from the KNHANES eye examinations. Furthermore, <2% of the patients with AMD knew they had the disease. This significant lack of awareness in patients with ARED has been observed in other countries. Based on a population-based survey assessing five common eye conditions among 3,280 Malays aged 40 to 80 years in Singapore, the proportion of awareness was the lowest for AMD (0.6%), followed by glaucoma (8.0%), diabetic retinopathy (15.3%), cataract (21.6%), and myopia (48%) [10]. The Los Angeles Latino Eye Study in the US reported a proportion of detected eye disease of 2.1% for AMD and 43.0% for cataract [22]. Based on the 2005 to 2008 National Health and Nutrition Examination Survey, 17.7% of Americans aged ≥40 years were aware of their AMD [26].
The substantial difference in the awareness rates between cataract and AMD in the present and earlier studies might be due to differences in the nature of symptoms and public disease recognition of each disease. Compared with AMD, cataract is more frequently detectable because blurriness is an easily recognized symptom [2728]. In contrast, symptoms of AMD are often considered to be age-related by those experiencing them, and they do not actively seek treatment [29]. This might have contributed to the low rate of AMD detection.
AMD awareness substantially increased 3.4-fold during the 3-year study period (0.69% to 2.38%) in contrast with cataract awareness, which only increased slightly (22.7% to 23.7%). Since the study did not specifically investigate reasons for this change in awareness, we can only speculate on potential influences. One important factor might be the increase in ocular examinations, possibly due to the significant increase in media-based publicity of AMD during the study period, encouraging the public to receive regular ophthalmologic evaluations. The increase in awareness might reflect an increase in AMD prevalence resulting from longer life expectancy and adherence to a more Westernized diet. Finally, the altered pattern in ocular examinations by ophthalmologists might be another influential factor. The development of newer instruments has facilitated fundus examinations without the need for pupil dilation. Increased knowledge of AMD among the newer generations of ophthalmologists might also have led to increased diagnosis.
Cataract awareness was greater in patients with chronic diseases such as diabetes or a family or prior history of ophthalmic diseases. Since these patients are in more frequent contact with their doctors, they have a greater chance of being diagnosed with eye disease. In the past, when routine medical examinations were rare, many patients with hypertension or diabetes were unaware of their conditions. Presently, blood pressure, blood glucose level, and blood lipid level measurements are commonly conducted in routine medical examinations in Korea, and the detection of hypertension and diabetes has substantially improved [30]. Similarly, if ophthalmic diseases such as AMD and cataract become fundamental components in routine medical examinations, patient awareness for these conditions would improve. However, promoting ophthalmic tests for detecting ARED in routine medical examinations would require preceding economic justification. For example, a cost-benefit analysis of additional ophthalmic tests in routine medical examinations should be conducted to compare the direct costs of the tests with the expected benefits from early diagnosis and prevention of associated complications. Furthermore, increasing patient awareness of the relevance of ophthalmic health is just as important as the inclusion of ophthalmic tests in routine medical examinations.
Subgroup analysis by age showed that some of the predictors of cataract awareness differ across age groups. Unlike other age groups, younger elderly patients (60 to 79 years) tended to be aware of their eye condition, because they had received higher education. Higher family income was a significant predictor only for the oldest patient group (≥80 years old). The presence of diabetes mellitus was not a significant predictor of awareness for those <60 years old.
This study has several limitations. First, due to limitations in the information provided by the 5th KNHANES, we could only focus on cataract and AMD and were unable to include other common AREDs that were not included in the survey such as glaucoma and diabetic retinopathy. Second, the multivariate analysis was conducted only in patients with cataract because only 16 of the 960 patients with AMD were aware of their condition. Future studies using KNHANES data collected over a longer period should have a larger sample size and allow examination of factors associated with AMD awareness through multivariate analysis.
In conclusion, the observed poor awareness of AREDs among the middle-aged and elderly Korean population highlights the seriousness of this potential public health problem in an aging society. Eye-related conditions and diabetes are significant predictors of patient awareness, implying that patients in frequent contact with their doctor have a greater chance of detecting eye disease. Therefore, ophthalmic tests should be more commonly available to patients, and public health education should emphasize the importance of regular check-ups for eye diseases.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
The paper has been presented in the 21st International Society for Pharmacoeconomics and Outcomes Research Annual Meeting on May 21-25, 2016, Washington, DC, USA.