A Case of Retinal Cavernous Hemangioma Diagnosed with Spectral Domain Optical Coherence Tomography
Article information
Dear Editor,
Retinal cavernous hemangioma (RCH) is a rare, benign, congenital vascular anomaly, incidentally diagnosed in asymptomatic patients. Its characteristics were first reported by Gass [1] in 1971, as multiple saccular intraretinal aneurysms with dark red color. In most cases, RCH presents with no symptoms, but sometimes it causes visual deterioration when the lesion involves macular and/or vitreous hemorrhage. Several reports have demonstrated that RCH may accompany cutaneous and central nervous system angiomatous lesions, so that RCH could be classified as part of a neuro-oculocutaneous syndrome [23]. The lesions are mostly located in the inner retinal layer or the surface of the optic disc, with a complex ‘grape bunch’ dilated vascular shape. In the former studies, few investigators reported optical coherence tomography (OCT) findings for RCHs, and the details of this disease have not been studied. Herein, we describe a patient diagnosed with RCH by various diagnostic modalities, with special emphasis on spectral domain optical coherence tomography (SD-OCT) findings.
A 54-year-old Korean female was referred to the retina clinic after a routine health checkup detected a pigmented retinal mass in the right eye. On initial examination, visual acuity was 20 / 20 in both eyes; intraocular pressure was 14 mmHg in the right eye and 15.1 mmHg in the left eye. Ophthalmic examination of the anterior segments revealed no other abnormal findings. Fundus examination showed 3-optic disc diameter sized ‘bunch-of-grapes’-like retinal lesions on the superotemporal side of the major vascular arcade (Fig. 1A). Fluorescein angiography showed hypofluorescent aneurysms in the vascular filling phase and later hyperfluorescence in the recirculation phase with typical fluorescein-blood levels. These are related to erythrocytic sedimentation in the ‘bunch-of-grapes’-like retinal lesion, known as fluorescence capping (Fig. 1B-1D) [4]. Based upon the results of the examinations stated above, the pigmented retinal mass was diagnosed as RCH. In most previous studies, RCH was diagnosed with clinical, genetic, pathologic, and conventional angiographic imaging [1234]. But in this case, it was possible to visualize a detailed cross-sectional image of the tumor lesion and adjacent structures with SD-OCT (Fig. 1E).
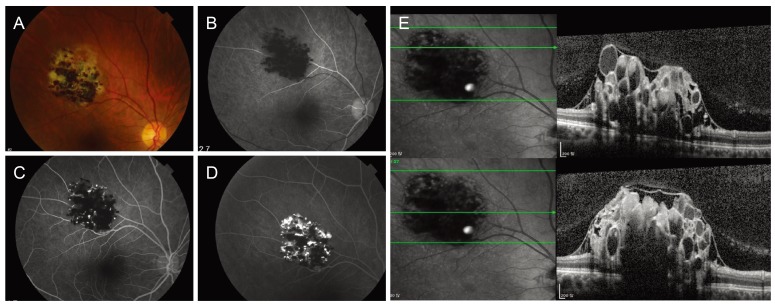
(A) A color fundus photograph of the right eye of the retinal cavernous hemangioma (patient at the first visit). Whitish-violet color retinal lesion is seen along the superotemporal arcade. (B-D) An early-phase fluorescein angiography image shows that the cystic space unstained with fluorescein, appears hypofluorescent. A late-phase fluorescein angiography image shows that the superior vascular cystic space, which is stained with fluorescein, appears hyperfluorescent. Hypofluorescence in the inferior space is related to erythrocytic sedimentation. (E) Spectral domain optical coherence tomography shows that the ‘grape bunch’ shape cystic hemangioma is located under the internal limiting membrane.
SD-OCT showed several remarkable findings in this RCH patient. First, the ‘grape bunch’ shape cystic hemangioma was located under the internal limiting membrane. This indicated that the tumor originated from the internal retinal layer. The inside of the cystic space had multiple hypo- and hyperref lective signals that originated from erythroclastic layering. Moreover, there was adhesion between the vitreous and the hemangioma, thus the risk of vitreous hemorrhage could not be ruled out.
A previous study used time-domain OCT to diagnose RCH [5], but there has been no report on using SD-OCT for RCH diagnosis, especially in Korean patients. Compared with the first generation OCT, SD-OCT technology yields higher axial resolutions allowing detailed RCH structural analysis. Although the confirmative diagnosis of RCH necessitates angiographic study, the characteristic SD-OCT lesion findings may facilitate accurate diagnosis without invasive examination. In addition, with the aid of SD-OCT, we were able to evaluate the risk of complications such as vitreous hemorrhage associated with vitreous adhesion to the lesion.
In conclusion, SD-OCT can be a useful tool for diagnosis and monitoring of RCH patients.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.