Structural and Functional Outcomes in Chronic Central Serous Chorioretinopathy Treated with Photodynamic Therapy
Article information
Abstract
Purpose
To study the retinal pigment epithelium (RPE) and retinal alterations in chronic central serous chorioretinopathy treated with photodynamic therapy, and its correlation with functional parameters such as best-corrected visual acuity (BCVA) and contrast sensitivity (CS).
Methods
Retrospective, noncomparative, consecutive evaluation by optical coherence tomography and its correlation with BCVA and CS in 31 eyes of 26 patients.
Results
In all affected patients, 88.5% were male with a mean age of 42.9 years. The right eye was involved in 64.5% of cases, bilateral in 19% and 73.9% were hyperopic (spherical refraction between 0 and +5.0 diopters). Of these cases, 51.5% had peri-RPE abnormalities, 17.3% hyperreflective substances at RPE, 19.4% RPE atrophy, 55.3% foveolar atrophy, 3.1% pigment epithelial detachment, 5.2% subretinal fluid persistence, 8.3% fibrin deposits, 68.4% photoreceptor inner and outer segment line interruption and 31.1% external limiting membrane interruption.
Conclusions
Time evolution and number of outbreaks were related to the decrease in foveal and chorodial thickness and in those with worse BCVA and CS. RPE abnormalities and atrophy were related to the age of onset of symptoms. Photoreceptor elongation has been correlated with poor BCVA and inner and outer segment line destructuring and interruption with poor CS.
Central serous chorioretinopathy (CSC) is a condition described in 1967 by Gass, characterized by the existence of neurosensory retinal detachment in the macular area [1]. It is detected by the patient as the appearance of a central or paracentral area of blurred vision in the visual field. There are controversies on the etiology of this disease and it is considered the most common hyperpermeability of the retinal pigment epithelium (RPE) [234]. However, Matsumoto et al. [5] suggested that the alteration was located in photo-receptor's outer layer. CSC occurs most frequently in young male patients with a type A personality, with an age range of 20 to 50 years, in hyperopic or emmetropic eyes [6], and in patients with gastric discomfort or patients in drug treatment with corticosteroids, oral contraceptives and sildenafil [78]. Although this disease is self-limiting with a good prognosis and a mean resolution time of 4 to 6 months, in 30% to 50% of cases there are recurrences and 5% can become chronic with severe damage to the RPE and photoreceptors, causing decreased best-corrected visual acuity (BCVA) [910].
There have been different treatments used in chronic cases such as diode laser by micropulses, ranibizumab, bevacizumab and verteporfin photodynamic therapy (PDT), at standard or half dosages [3411]. Verteporfin PDT treatment has obtained good results by the induction of choroidal vascular perfusion narrowing and consequently, decreases choroidal exudation [12]. However, several studies have suggested that PDT may increase the risk of retina and RPE complications and may further injure the retina and RPE in chronic CSC. This is the reason why some authors recommend the application of half-dose verteporfin with PDT in chronic cases when possible [1314].
Noninvasive cross sectional posterior segment tests as optical coherence tomography (OCT) allows one to visualize and quantify macular defects, which are characteristics of this disease [311]. The aim of this review is to study the retinal and RPE changes in chronic CSC cases (more than six months duration) that were treated with PDT, and establish its correlation with BCVA and contrast sensitivity (CS).
Materials and Methods
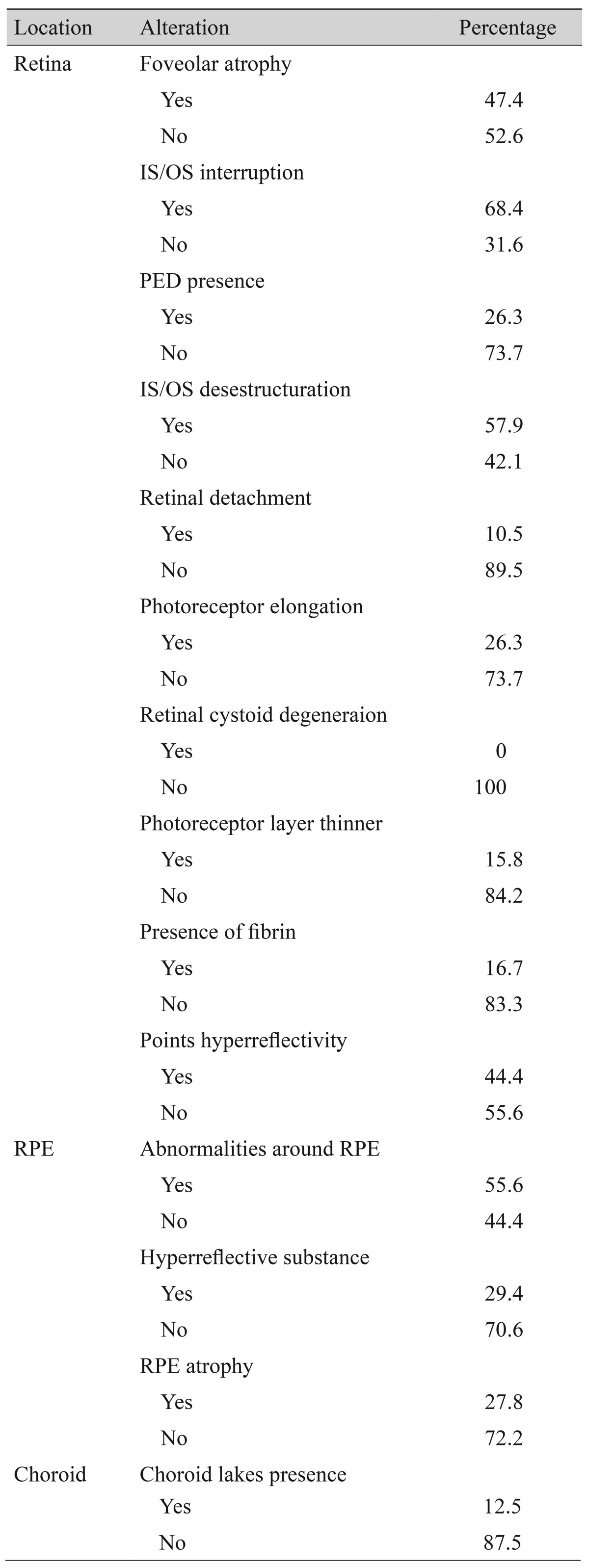
Retrospective, noncomparative consecutive study conducted in a tertiary center in Madrid, Spain. Patients with chronic CSC (at least 6 months or longer) treated with verteporfin PDT were included. Patients with media opacities or uncontrolled glaucoma, history of intraocular surgery or previous vitreoretinal disease were excluded. All patients underwent a complete ophthalmic examination including BCVA (logarithm of the minimum angle of resolution, logMAR), CS (Pelli Robson), biomicroscopy, funduscopy and OCT (software 512x128 macular cube and 5 HDline Cirrus raster; Carl Zeiss Meditec, Dublin, CA, USA) (Fig. 1). We considered individual epidemiological factors (sex, age, personality type, history of gastrointestinal disease, affected eye, refraction and previous systemic and ocular treatments), and the following variables collected by OCT: foveolar atrophy, subretinal fluid persistence, RPE integrity, peri-RPE abnormalities, pigment epithelium detachment (PED), hyperreflective substances, presence of fibrin deposits, photoreceptor inner and outer segment (IS/OS) line interruption, external limiting membrane abnormalities, and the presence of choroidal lakes and choroidal thickness (Table 1 and Fig. 2).

(A) Affected eye best-corrected visual acuity (logarithm of the minimum angle of resolution). (B) Affected eye contrast sensitivity.

(A) Case A with hyper-reflective substances visualized by optical coherence tomography (OCT). (B) Case B shows anatomic success objectified by OCT. (C) Case C, OCT demonstrates foveolar atrophy. (D) Case D, pigment epithelial detachment and inner and outer segment line interruption. T = temporal; N = nasal.
All statistical tests were analyzed using SAS ver. 9.1 (SAS Institute, Cary, NC, USA). Pearson's chi-square or Fisher exact tests were applied when dealing with qualitative variables, while the Mann-Whitney test was used to determine the association between quantitative and qualitative variables. Quantitative variables were analyzed using Pearson bivariate correlations. Values with p < 0.05 were considered significant.
At the end of the study, anatomic success was considered to be complete resolution of neurosensory detachment, macular thickness of 255.66 ± 8.61 microns and the absence of alterations in IS/OS layer and RPE [15]. The procedures performed were carried out in accordance with the Declaration of Helsinki, and PDT treatment was based on the indications of TAP study [16]. Informed consent was obtained from all patients after a full explanation of the study.
Results
We studied a total of 31 eyes from 26 patients and 88.5% were men, with a mean age of 42.92 years and an age range of 29 to 57 years. Among the patients, 64.5% chronic CSC had right eye involvement and 19% had bilateral involvement. Our findings showed that 73.9% of patients were hyperopic, 83.3% of patients had type A personality, 27.3% reported gastrointestinal discomfort and 29.2% were under treatment with corticosteroids or oral contraceptives at the time of the outbreak. Finally, 8% of patients had recurrences.
Over 71% of patients with chronic CSC received standard doses of verteporfin PDT and 28% received half-dose treatment. Final BCVA logMAR average was 0.17 with a mean of 29.77 CS, with no statistically significant difference in BCVA and CS regarding the opposite eye. On examination conducted by OCT, anatomic success was found in 20 eyes. Of the remaining 11 eyes, 55.3% had foveal atrophy, 5.2% persistence of subretinal fluid, 51.5% peri-RPE abnormalities, 19.4% RPE atrophy, 17.3% hyperreflective substances, 3.1% PED, 8.3% fibrin deposits, 68.4% IS/OS line interruption, and 31.1% external limiting membrane interruption.
Foveal and choroid thickness, IS/OS line interruption, and photoreceptor elongation were correlated with CSC time evolution. RPE abnormalities and RPE atrophy are related to the age at onset of symptoms. Fibrin and PED presence were correlated with refraction. Moreover, BCVA and CS were affected by the evolution time, the number of outbreaks, foveal thickness, choroid thickness and IS/OS layer destructuring.
Discussion
The microstructural morphological study of the retina using OCT allows one to quantify the typical findings of the disease and to correlate with the variables studied [17]. A relevant difference detected in this study with respect to previous reviews, is the relationship between long-term anatomical changes detected in patients with chronic CSC and BCVA and CS. We have found that after PDT application in patients with chronic CSC, the patients did not exhibit significant ocular nor systemic adverse effects, except for one case in which a subretinal neovascular membrane developed [18]. No significant differences were found in epidemiological factors such as age, sex, bilaterality, and personality type [19].
Time evolution and total number of outbreaks were related to a decrease in foveal and choroid thickness, and were also related to worse BCVA and CS (p < 0.05). The presence of fibrin deposits and subretinal precipitates had no statistical significance in our study in relation to final BCVA and CS. Iida et al. [20] correlated these findings with poor visual acuity due to deposits of degenerative material around the perifoveolar vessels producing a decrease in capillary flow.
Weingessel et al. [21] demonstrated that the integrity of the IS/OS line was an important predictive factor for final BCVA. In this study, photoreceptor outer segment elongation was correlated with worse BCVA, and IS/OS line destructuring and interruption with worse CS. Our study did not determine whether the detected IS/OS layer disturbance is prior to PDT treatment or created by it, in agreement with the study by Ratanasukon et al. [22]. RPE abnormalities and atrophy were correlated with the age at onset of symptoms (p < 0.05). We could not detect choroidal defects in patients treated with PDT, however in other studies with indocyanine green angiography and OCT, PDT was shown to directly affect choroid functionality and histology [423].
Our study has a number of limitations such as a small sample size and lack of a control group. To obtain conclusive results another multicenter study with a larger sample size should be conducted in order to give value to the results.
The ideal treatment for CSC should preserve photoreceptor anatomy and remove subretinal fluid without adverse effects on the retina and choroid. Fujita et al. [13] showed that there is a significant improvement in the retina after half-dose PDT in eyes with chronic CSC. This improvement was correlated with the preservation of the IS/OS line.
In conclusion, IS/OS layer alteration in patients with chronic CSC treated with PDT appears to be responsible for BCVA and CS decreases, which are essential parameters for the assessment and monitoring of such patients.
Acknowledgements
We appreciate the help and support received from the Ophthalmology Service of Hospital Universitario La Paz, Madrid, Spain.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.