Bilateral Sequential Optic Neuritis in Behçet's Syndrome
Article information
Dear Editor,
Optic neuritis is the most common inflammatory optic neuropathy affecting young adults [1]. Less commonly, optic neuritis may be associated with systemic autoimmune disease, of which Behçet's syndrome is an extremely rare cause, with only 20 identified cases to date [2]. To the best of our knowledge, there have been no reports in Korean patients. Herein, we report a patient presenting with bilateral sequential optic neuritis who was finally diagnosed with Behçet's syndrome.
30-year-old man visited the outpatient clinic for headache, periocular pain, and scotoma in his left eye. The symptom had developed over a period of several hours. He had no remarkable medical history, except experience of similar symptoms in his right eye about one year prior. Brain magnetic resonance imaging, cerebrospinal fluid tapping, and all markers for infectious diseases showed normal results. On ophthalmologic examination, his best corrected visual acuity was 20 / 20 in both eyes, and the anterior segments were normal in both eyes. Small central scotoma was noticed from Goldmann perimetry in both eyes. The left disc was swollen (Fig. 1A), and a small pigment epithelial detachment was found in his left eye on optical coherence tomography. We commenced treatment with intravenous methylprednisolone at a dose of 125 mg four times a day for three days. On the last day of steroid pulse therapy, the papillitis on the left eye had resolved fully.
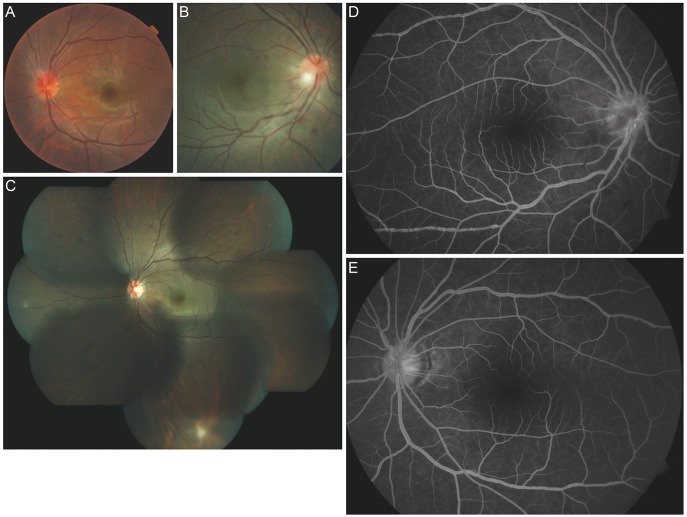
Fundus photographs showing the clinical course of the patient. (A) Fundus photograph of the left eye showing severe disc swelling. (B) Fundus photograph of the right eye during the second episode showing disc swelling with a granulomatous lesion at the inferotemporal border of the optic disc. (C) Fundus montage of the left eye showing dot opacities at the mid-peripheral retina. (D,E) Fluorescein angiography of both eyes showing mild venous sheathing with definite venous beading.
Two years later, he revisited our clinic for blurred vision and pain with movement in the right eye. His best corrected visual acuities were 20 / 30 in right eye and 20 / 20 in left eye. Slit lamp examination showed a trace amount of cells in the anterior chamber of both eyes. Fundus examination disclosed a granulomatous lesion on the inferotemporal border of the right disc (Fig. 1B), mild disc swelling of the right eye, and dot opacities in the mid-peripheral retina in the left eye (Fig. 1C). Fluorescein angiography demonstrated mild vessel sheathing with definite venous beadings in both eyes (Fig. 1D and 1E).
On more detailed history taking, the patient described several oral ulcers and pustular skin lesions on his legs, which had continued for several months. The pathergy test demonstrated positive results. As he fulfilled more than two of the four hallmark symptoms which are recurrent genital ulcerations, eye involvement, skin lesions, and a positive pathergy test, he was diagnosed with Behçet's disease. We started intravenous methylprednisolone 1 g daily for five days.
One week after discharge, the best corrected visual acuity of his right eye recovered to 20 / 20. Both anterior chambers were clear, and no disc edema was detected. He continued taking oral methylprednisolone, which was gradually tapered over six weeks. On the last follow-up visit, his best corrected visual acuities were 20 / 20 in right eye and 20 / 30 in left eye, and all examination results were unremarkable.
This case demonstrates recurrent episodes of acute optic neuritis involving both eyes in Behçet's syndrome. Although primary optic neuropathy is exceedingly rare in Behçet's patient, the possibility of Behçet's syndrome as an underlying cause of optic neuritis should be considered. As Behçet's syndrome is a chronic, relapsing, and occlusive vasculitis disease, lifelong immunosuppressive treatment is needed in order to prevent recurrence of neurological and ophthalmic complications [3].
Notes
No potential conflict of interest relevant to this article was reported.