Resolution of Recalcitrant Uveitic Optic Disc Edema Following Administration of Methotrexate: Two Case Reports
Article information
Abstract
A 13-year-old male and a 15-year-old female presented with optic disc edema associated with chronic recurrent uveitis. While the ocular inflammation responded to high doses of oral prednisolone, the disc edema showed little improvement. After oral administration of methotrexate, the disc edema and ocular inflammation were resolved, and the dose of oral corticosteroid could be reduced.
Optic disc edema or papillitis is commonly associated with chronic anterior uveitis in children, and its prevalence has been reported to be 21% [1]. However, there have been few reports regarding the treatment for recalcitrant uveitic disc edema, especially in children [2]. Methotrexate, a member of the antimetabolite class, has been used as an immunosuppressive agent that is effective against ocular inflammatory disease [3]. Here, we report two cases of children with chronic recurrent uveitis and disc edema that did not respond to oral corticosteroid but that showed significant improvement following administration of methotrexate.
Case Report
Case 1
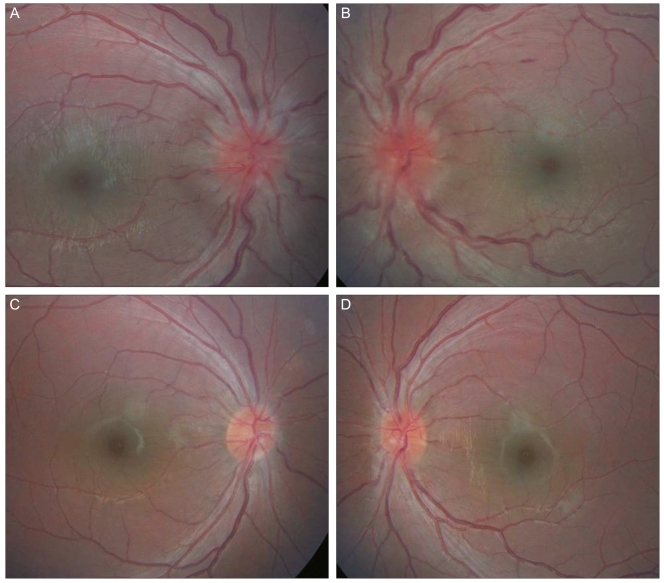
A 13-year-old male patient presented with bilateral optic disc edema accompanied by idiopathic chronic anterior uveitis that had been ongoing for two months. At that time, his visual acuity was 20 / 25 in the right eye and 20 / 40 in the left eye, and there was no macula edema on funduscopic examination or optical coherence tomography. He had been taking 30 mg (0.52 mg/kg) of oral prednisolone daily. We could not find any neurologic or systemic abnormalities to explain the disc edema. For six months, he had taken oral prednisolone and could not taper it due to the recurrence of ocular inflammation. In addition, the disc edema had not subsided, even with a high dose of oral prednisolone (60 mg [1.05 mg/kg] per day). Thereafter, we added oral methotrexate 10 mg (0.18 mg/kg) per week to the daily dose of prednisolone 30 mg (0.52 mg/kg). After 3 weeks of methotrexate, the disc edema and ocular inflammation were alleviated, and his vision improved to 20 / 20 in both eyes (Fig. 1A and 1B). The disc edema and inflammation recurred during the oral prednisolone tapering period. However, a daily low-to-moderate dose of prednisolone (10-20 mg) combined with a weekly dose of methotrexate 15 mg (0.26 mg/kg) alleviated the ocular inflammation and disc edema (Fig. 1C and 1D). After 18 months of methotrexate and tapering the dose of oral prednisolone, the patient achieved stable vision without optic disc edema or ocular inflammation.
Case 2
A 15-year-old female patient presented with optic disc edema in the right eye and bilateral idiopathic panuveitis (Fig. 2A and 2B) with no associated neurologic or systemic abnormalities. Despite continued daily administration of oral prednisolone 30 mg (0.44 mg/kg) for 4 months, the disc edema persisted. We added a daily dose of cyclosporine 150 mg (2.21 mg/kg) to her medications. Although the anterior chamber inflammation had improved significantly, the disc edema persisted. We then prescribed a weekly dose of methotrexate, starting at 7.5 mg (0.11 mg/kg) and increasing to 15 mg (0.22 mg/kg), while reducing the prednisolone dose to 10 mg (0.15 mg/kg) per day and discontinuing the cyclosporine. The disc edema resolved dramatically one month after the initiation of methotrexate (Fig. 2C and 2D). The dose of oral prednisolone was tapered while increasing the dose of methotrexate to 20 mg weekly without recurrence of disc edema or ocular inflammation. After one year of methotrexate, the patient had good visual acuity in both eyes, and the intraocular inflammation was controlled without optic disc edema.
Discussion
Optic disc edema from various causes may result in irreversible axonal damage and progressive visual field loss [4]. Although there have been reports of resolution of optic disc edema after successful treatment of anterior uveitis [2,5], there is no definite treatment guideline for uveitic disc edema in children who do not respond to corticosteroids. While corticosteroids are one of the traditional treatment regimens of uveitis, chronic oral intake by children can lead to serious side effects, i.e., cataract, glaucoma, and growth retardation in prepubescent children. Recent studies have reported that methotrexate is moderately effective for controlling ocular inflammation and for achieving corticosteroid-sparing objectives as a monotherapy or in combination with other agents in both adults and children [3,6,7].
For long-term treatment with methotrexate, caution should be exercised regarding the systemic and ocular side effects. Elevated liver enzymes, nausea, fatigue, cytopenia, stomatitis, bone marrow suppression and liver cirrhosis have been reported as systemic side effects of methotrexate [8-12]. Ocular side effects include irritation and dry eye [13], as well as the rare occurrence of toxic optic neuropathy, which can be reversed by the intake of folic acid [14-17]. Thus, regular ophthalmic and systemic examination is mandatory during methotrexate intake.
In our cases of steroid-refractory uveitic optic disc edema in children, methotrexate had a beneficial effect on the resolution of optic disc edema and controlled intraocular inflammation while sparing the corticosteroid. We are unaware of previous reports showing the efficacy of methotrexate reducing recalcitrant uveitic disc edema in children. Therefore, we think that this report is a significant reference regarding the effect of methotrexate in the treatment of pediatric uveitis accompanying disc edema.
Notes
No potential conflict of interest relevant to this article was reported.