 |
 |
| Korean J Ophthalmol > Volume 26(5); 2012 > Article |
Abstract
We present cases of primary open angle glaucoma patients without previous history of pseudoexfoliation who developed pseudoexfoliative materials on the anterior surface of the intraocular lens after cataract surgery. Among 5 unilateral pseudophakic pseudoexfoliation cases, 3 showed a more advanced state of glaucoma in the affected eye. The other 2 cases showed progression of glaucoma in the affected eye after the development of pseudophakic pseudoexfoliation, while the unaffected eyes remained stable. In the latter 2 cases, control of intraocular pressure was difficult, and more glaucoma medication was needed in the affected eye. Pseudophakic pseudoexfoliation in glaucoma patients with no history of pseudoexfoliation syndrome or pseudoexfoliative glaucoma has not been reported. In our cases, the eyes which developed pseudophakic pseudoexfoliation showed a more advanced state of glaucoma, more difficulty controlling intraocular pressure, and faster progression of glaucoma. More observation is needed, but we cautiously postulate that pseudophakic pseudoexfoliation may have a role as a clinical risk factor in the prediction of glaucoma progression.
Pseudophakic pseudoexfoliation is a rare condition; only about 10 cases have been reported [1-4]. The pattern of radial striations on the anterior surface of the intraocular lens (IOL) is similar to the pattern commonly observed on the crystalline lens of patients with pseudoexfoliation syndrome. Pseudoexfoliation syndrome increases clinical risk of glaucoma by 5- to 10-fold. However, the etiology and clinical significance of pseudophakic pseudoexfoliation are not known.
We present patients with no history of pseudoexfoliation syndrome who developed pseudoexfoliative materials on the anterior surface of the IOL after cataract surgery (Table 1). These patients had no evidence of exfoliative materials on ocular tissues, iris atrophy at the pupil margin, irregular pigmentation on the trabecular meshwork, or poorly dilated pupils during follow-up. Except for one case that was referred to our hospital, the remaining four cases received follow-up for several years by one ophthalmologist (three cases had received follow-up for over 10 years), and there was no evidence of pseudoexfoliation syndrome in those eyes. After an uneventful phacoemulsification with IOL implantation in the bag, pseudoexfoliative materials developed on the anterior surface of the IOL. However, interestingly, the eye with this condition had a more uncontrolled state of glaucoma than the opposite eye.
A 69-year-old female was diagnosed with primary open angle glaucoma in 1999. She was using β-blockers (Betoptic; Alcon, Fort Worth, TX, USA) in both eyes. At diagnosis, her visual field examination showed a mean deviation (MD) of -7.41 dB in the right eye and MD -28.36 dB in the left eye. In 2003, she presented with symptomatic cataract in both eyes. No evidence of pseudoexfoliation was observed in either eye. Uneventful phacoemulsification with IOL implantation was performed in both eyes in 2003.
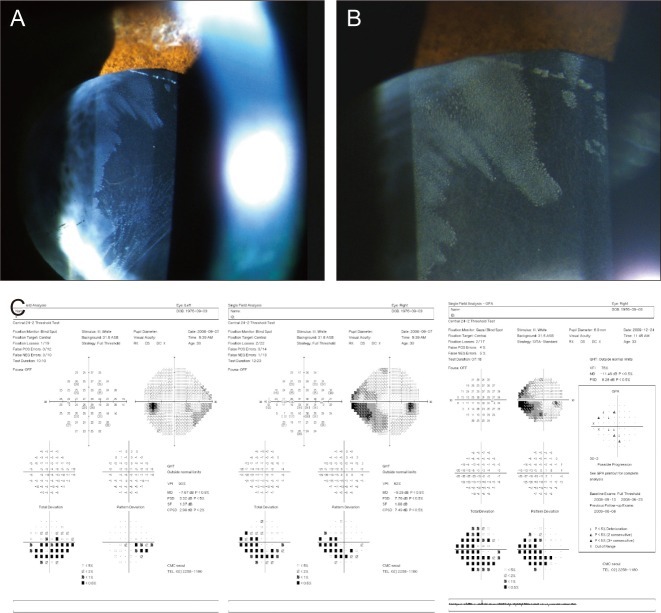
In 2009, a concentric ring of fine, spoke-like opacities resembling the deposits seen in pseudoexfoliation were observed on the anterior surface of the IOL optic in the left eye. A clear zone was observed between the spoke-like opacities and the anterior capsulorhexis margin (Fig. 1). No pseudoexfoliative materials were found in the right eye.
Patient 2 was a 56-year-old male who was referred to our clinic for uncontrolled IOP in the left eye in 2009. He was diagnosed with primary open angle glaucoma after an uneventful phacoemulsification with posterior chamber lens (PCL) implantation in both eyes in 2008. Previous records noted no evidence of pseudoexfoliation before cataract surgery. He was using prostaglandin (Xalatan; Pfizer, New York, NY, USA) in both eyes and a combination drug (Combigan; Allergan, Irvine, CA, USA) in the left eye. IOP was 16 mmHg in the right eye and 23 mmHg in the left eye. Visual field examination showed MD -8.9 dB in the left eye (Fig. 2).
Patient 3 was a 74-year-old female diagnosed with primary open angle glaucoma in 2007. In 2009, the patient underwent uneventful phacoemulsification with PCL implantation in both eyes. One year later, she showed uncontrolled IOP of 28 mmHg in the left eye. The uncontrolled eye showed pseudoexfoliative materials on the IOL surface of the affected eye. More glaucoma medication was added to control the IOP in the affected eye.
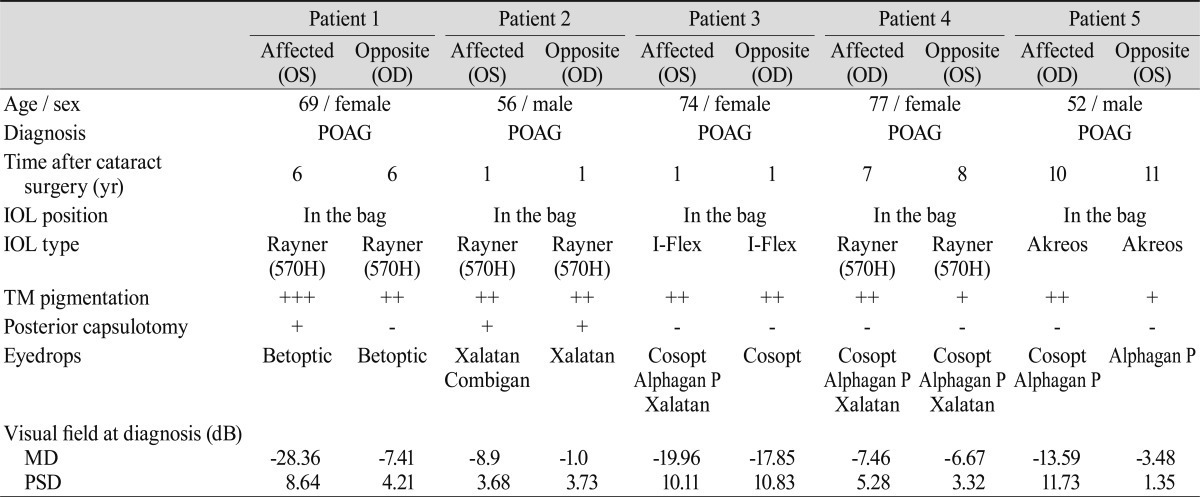
A 77-year-old female was diagnosed with primary open angle glaucoma in 1996. She underwent uneventful phacoemulsification with PCL implantation in the left eye in 2001 and in the right eye in 2002. Her glaucoma medications had been changed several times, and she was currently using a β-blocker/carbonic anhydrase inhibitor (Cosopt; Merck & Co. Inc., Whitehouse Station, NJ, USA), α-agonist (Alphagan P, Allergan), and prostaglandin (Xalatan, Pfizer) in both eyes. Visual field examination showed constant progression in her right eye since 2006. In 2007, a dilated eye examination showed pseudoexfoliative material on the anterior IOL surface on the inferior, temporal side. In 2008, the right eye showed a more progressed visual field examination result, and dilated eye examination showed increased pseudoexfoliative material on the superior side of the IOL. IOP was 11 to 16 mmHg in both eyes during the follow-up period (Fig. 3).
A 52-year-old male was diagnosed with primary open angle glaucoma in 1995. The right eye required several changes of glaucoma medication due to progression of glaucoma. Visual field examination showed constant progression in the right eye. Ten years after cataract surgery in both eyes, pseudophakic pseudoexfoliation developed in the right eye. Visual field examination showed MD -13.59 dB in the affected right eye, compared to MD -3.48 dB in the left eye. The IOP was similar in both eyes, in the range of 14 to 21 mmHg.
In the previously reported cases, pseudophakic pseudoexfoliation developed from four to ten years after cataract surgery [1-4]. None of the reported eyes had previous glaucoma, and this is the first report to describe the development of pseudophakic pseudoexfoliation in glaucomatous eyes. One study reported that the affected eye developed glaucoma after development of pseudophakic pseudoexfoliation; however, those cases were eyes with pseudoexfoliation syndrome [3]. The report postulated that posterior capsulotomy alters the flow of aqueous humor and may have triggered the deposition of pseudoexfoliative materials on the IOL surface. Another report postulated that sulcus implantation of the IOL might have led to the deposition on the IOL surface [2]. However, different features were found in our cases. Pseudophakic pseudoexfoliation developed as early as one year after cataract surgery. Posterior capsulotomy was performed in only two cases, and all five cases had the IOL positioned in the bag. The reported cases had various lens designs and materials, and these do not seem to be the most significant factors in the development of pseudophakic pseudoexfoliation.
All of our patients had been previously diagnosed with open angle glaucoma. Patients 1, 2, and 5 presented with a more advanced state of glaucoma at diagnosis, even before the development of pseudophakic pseudoexfoliation in patient 1. In patients 2 and 3, the affected eye showed more rapid progression of glaucoma. In patients 4 and 5, control of IOP was more difficult, and more glaucoma medications were needed to achieve target IOP. A previous report described four cases in which patients developed glaucoma more than eight years after cataract surgery in the eye with pseudophakic pseudoexfoliation [3]. Although it could simply be a matter of the presence of pseudoexfoliative material deposition, our cases showed no evidence of previous pseudoexfoliation syndrome. In addition, the affected eye showed a more rapid course of glaucoma with difficult control of IOP.
Although we do not know the precise etiology, we can cautiously postulate that control of glaucoma in an eye with pseudophakic pseudoexfoliation is especially challenging. As with pseudoexfoliation syndrome, pseudophakic pseudoexfoliation may have a role as a clinical risk factor in the prediction of glaucoma progression. Close follow-up is important, and aggressive treatment of the affected eye may be required in eyes with pseudophakic pseudoexfoliation. Further longitudinal evaluation with more cases will be needed to determine the exact clinical significance of this occurrence.
REFERENCES
1. Stewart JF, Jay JL. Pseudoexfoliation material on an acrylic lens. Br J Ophthalmol 1995;79:1050-1051.

2. Bahadur GG, Masket S. Pseudophakia with pseudo-pseudoexfoliation. J Cataract Refract Surg 2007;33:1827-1828.


Fig. 1
Photograph of the affected left eye of patient 1. (A) View of dilated pupil shows concentric ring on the intraocular lens (IOL) optic. (B) A detailed view shows fine, spoke-like opacities on the IOL optic with radial striations. There is a clear zone between the capsulorhexis margin and the opacities.

Fig. 2
Patient 2. Disc photographs of right (A) and left (B) eyes showing a more advanced state of glaucoma in the affected left eye. (C) A view of the fine deposits on the intraocular lens surface in the left eye.

Fig. 3
Photograph and visual field printout of the affected right eye of patient 4. (A) View of dilated pupil shows deposits on the anterior surface of the intraocular lens optic, which is more pronounced on the superior side. (B) A detailed view shows fine, dot-like deposits with radial striations. (C) Glaucoma progression analysis using the Humphrey Field Analyzer shows progression of glaucoma in the right eye.
- TOOLS
-
METRICS

- Related articles
-
Clinical Result of Prolonged Primary Chemotherapy in Retinoblastoma Patients.2003 June;17(1)



 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print



