Therapeutic Effect of 0.03% Tacrolimus Ointment for Ocular Graft versus Host Disease and Vernal Keratoconjunctivitis
Article information
Abstract
Purpose
To determine whether topical tacrolimus might prove effective in the treatment of refractory anterior segment inflammatory diseases, and to evaluate its efficacy in eyes with ocular graft versus host disease (GVHD), and vernal keratoconjunctivitis (VKC).
Methods
Twenty-eight eyes of 14 patients with anterior segment inflammation refractory to steroid treatment were treated with 0.03% tacrolimus ointment at the Samsung Medical Center, Seoul, Korea from March 2008 through August 2009. Seven patients had ocular GVHD and seven had VKC. We evaluated the conjunctival and corneal inflammatory change at one, two, four, and eight weeks after treatment with a scoring system. Time to initial response of treatment and therapeutic effect between GVHD and VKC was also analyzed. After the eight-week treatment period, patients were divided into two groups (maintenance group and discontinuance group). Eight patients maintained the treatment for an additional four months, and six patients discontinued the treatments. Therapeutic effect was also compared between the groups at eight weeks and six months after treatment.
Results
The mean conjunctival and corneal inflammation score was reduced significantly at eight weeks after treatment (p < 0.0001). The therapeutic effect in conjunctival inflammation was first noted at week two after the initial treatment (p = 0.002); reduction in corneal inflammation was first noted at one week (p = 0.0009). When compared according to diagnosis, no therapeutic difference was detected between the groups (p > 0.05). Six months after treatment, we noted no therapeutic differences between the maintenance group and discontinuance group (p > 0.05).
Conclusions
0.03% tacrolimus ointment was safe and effective for use in anterior segment inflammatory disease refractory to steroid.
The treatment of refractory anterior segment inflammatory diseases is still a dilemma. Most cases require steroids to be used over a long time, but such treatment should be used with caution due to the risk of steroid induced cataract, glaucoma [1], and superinfections [2].
Tacrolimus, referred to as FK506, is a potent immunosuppressive macrolide agent, which is isolated from Streptomyces tsukubaenis [3]. Tacrolimus inhibits T-cell activity by decreasing the transcription of interleukin-2 and lymphokines [4]. These inflammatory cytokines have been blamed in the pathogenesis of many ocular surface disorders. Systemic tacrolimus has been used to prevent allograft rejection in liver, kidney, and heart transplantation patients [5-7]. Topical tacrolimus (Protopic ointment 0.03%; Astellas Pharma, Tokyo, Japan) has been proven effective in the treatment of atopic dermatitis [8]. However, there are only a few reports regarding its use for the treatment of anterior segment inflammatory disorders [9-11]. Recently, several studies have been conducted on topical tacrolimus, but the majority of these have been case reports. However, no studies have yet been reported to determine the time required for the medication to show an effect or to determine the proper time to discontinue that treatment.
The principal objective of this study was to determine whether topical tacrolimus treatment is effective in anterior segment inflammatory disorders such as chronic ocular graft versus host disease (GVHD) and vernal keratoconjunctivitis (VKC), which have dependency to steroid or are refractory to said therapy. Also, we aimed to evaluate the time period required to achieve a significant effect after tacrolimus therapy and the proper duration of treatment. Thus, this is the first study to analyze the timeframe of the use of this medication, and our results should also prove useful in guiding the use of tacrolimus in ophthalmology.
Materials and Methods
This prospective study was conducted at Samsung Medical Center, Seoul, from March 2008 to August 2009. Thirty-two eyes of 16 patients who provided informed consent were enrolled after approval from the institutional review board. The study was carried out within the tenets of the Declaration of Helsinki. The inclusion criteria were: patients with ocular GVHD and VKC refractory to standard steroid therapy, worsening of symptoms during steroid tapering or having steroid induced complications, and no posterior segment inflammation. We focused on these two disorders for our study as they are relatively common, always require steroid therapy, and have mostly unsatisfactory outcomes. Exclusion criteria were patients with a history of herpes and patients already on cyclosporine.
Before commencing the treatment all patients underwent a detailed slit lamp examination and an anterior segment photograph was taken for follow-up analysis. The patients were asked to apply 0.03% tacrolimus ointment in the lower conjunctival sac twice a day after using a drop of 1% prednisolone eye drop. Prior to tacrolimus treatment, the mean frequency of prednisolone acetate 1% was 4.3 ± 3.1 per day and the mean duration was 5.6 ± 4.7 months.
Patients were made aware that the ointment is used for skin conditions and this study is an off label use. They were informed that the ointment may cause burning, stinging sensation, and blurred vision due to its oil based formulation. Two patients refused to use the ointment due to a burning sensation during the first week of treatment and so we were left with 14 patients. Seven patients of those remaining had ocular GVHD and seven persons had VKC.
All patients received tacrolimus treatment for eight weeks, and we evaluated them at weeks one, two, four, and eight. At every follow-up, we looked for inflammatory changes and also noted complaints such as a burning or foreign body sensation.
At every follow-up, patients were asked to gradually reduce the steroid eye drop usage. Also, we prescribed artificial tear drops to all patients. For the GVHD patients, there were no changes of systemic immunosuppressive treatment during this study period.
After an initial period of eight weeks of treatment, we gave all patients the option to maintain or to discontinue the treatment, eight patients who wished to continue treatment maintained the therapy (maintenance group) for an additional four months, and treatment was discontinued for another six patients (discontinuance group).
To assess the changes in inflammatory status, we used an inflammatory score given by Tanaka et al. [12]. The inflammation of conjunctiva was scored by four levels and inflammation of the cornea was scored by five levels. The conjunctival inflammation was scored with the following four levels: 0, none; 1, mild (mild hyperemia and flat papillary hypertrophy); 2, moderate (moderate hyperemia and papillary hypertrophy); 3, severe (severe hyperemia and high papillary hypertrophy). Corneal inflammation was scored with inflammation scores of (five levels): 0, none; 1, mild (superficial punctuate keratitis [SPK] less than half of cornea); 2, moderate (SPK more than half of cornea); 3, severe (corneal epithelial defect); 4, very severe (corneal ulcer or plaque) [12]. At all follow-up times, anterior segment photography was performed, and two examiners assessed the resulting image and gave marks blindly. At the final six-month follow-up, we compared surface inflammation between the maintenance group and the discontinuance group.
For statistical analysis, PASW ver. 17.0 (SPSS Inc., Chicago, IL, USA) was used. We utilized the Wilcoxon signed rank test with Bonferroni's correction to determine the time point at which the reduction of inflammation first appeared after beginning treatment. The Wilcoxon signed rank test was utilized to analyze the reduction of the instillation frequencies of topical steroids after treatment. To assess differences arising in diagnoses and maintenance, we utilized a Mann-Whitney test with Bonferroni's correction. A p-value of less than 0.05 was considered significant.
Results
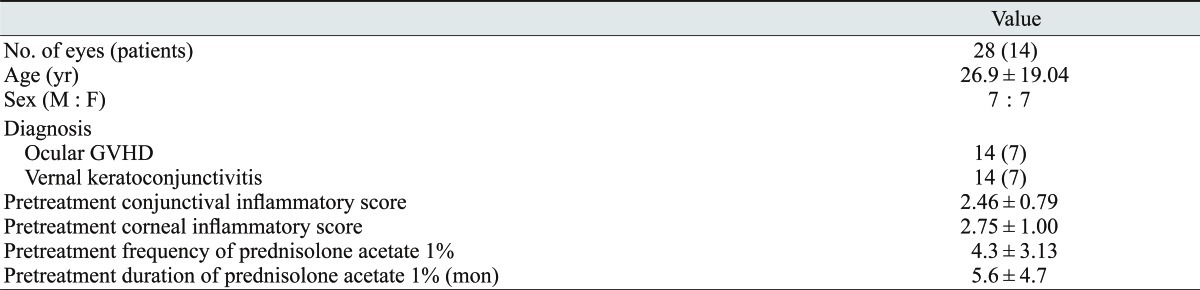
The mean age of the patients was 26.9 ± 19.04 years (range, 9 to 62 years), and the ratio of males to females was 7 : 7. Among these patients, 14 eyes from seven patients had ocular GVHD and 14 eyes of seven patients had VKC (Table 1).
The mean conjunctival inflammation and corneal inflammation scores prior to treatment were 2.46 ± 0.79 and 2.75 ± 1.00, respectively. After treatment with tacrolimus ointment, the scores were 2.21 ± 0.63 and 2.25 ± 1.04 at a week one, 1.79 ± 0.73 and 1.71 ± 0.84 at week two, 1.29 ± 0.50 and 1.23 ± 0.71 at week four, and 0.75 ± 0.40 and 0.80 ± 0.61 at week eight, respectively. The mean conjunctival inflammation score was significantly reduced (p < 0.0001), from 2.46 ± 0.79 to 0.75 ± 0.40 at eight weeks after treatment. The mean corneal inflammation score was reduced significantly (p < 0.0001), from 2.75 ± 1.00 to 0.80 ± 0.61 at eight weeks after treatment (Figs. 1 and 2).
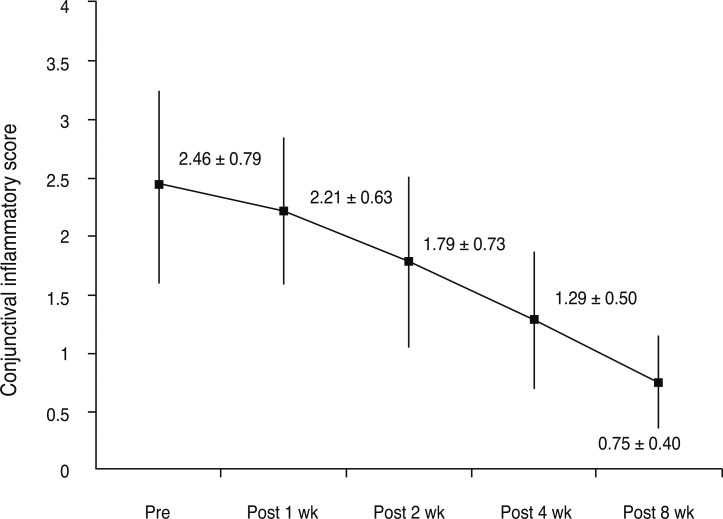
The conjunctival inflammatory score change. The degree of inflammation reduction by section was assessed at weeks one, two, four, and eight after beginning the tacrolimus ointment treatment. The mean conjunctival inflammation score was reduced significantly (p < 0.0001), from 2.46 ± 0.79 to 0.75 ± 0.40 at eight weeks after treatment. Meaningful reductions of inflammation initially appeared at week 2 (p = 0.002). Pre = pretreatment; Post = posttreatment.
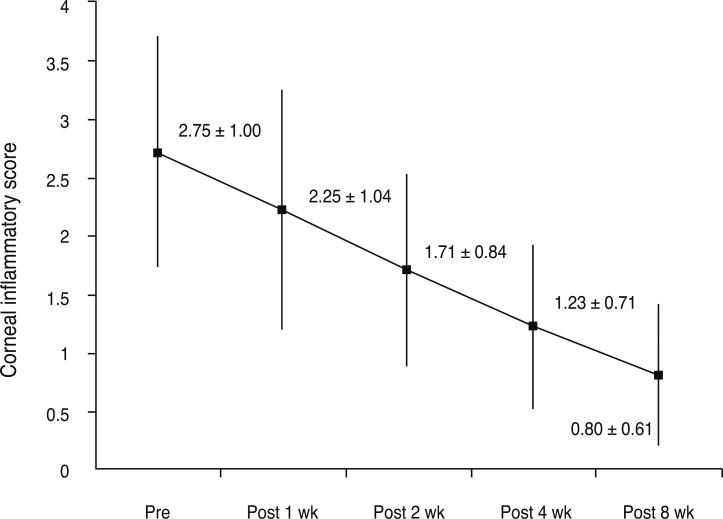
The corneal inflammatory score change. The degree of inflammation reduction by section was assessed at weeks one, two, four, and eight after the beginning of tacrolimus ointment treatment. The mean conjunctival inflammation score was reduced significantly (p < 0.0001), from 2.75 ± 1.00 to 0.80 ± 0.61 at eight weeks after treatment. Meaningful reductions in inflammation were initially observed at week 1 (p = 0.0009). Pre = pretreatment; Post = posttreatment.
On analysis of inflammation scores for each section, a significant reduction of inflammation initially appeared at week two for the conjunctiva (p = 0.002) and at week one for the cornea (p = 0.0009) (Figs. 1 and 2). The response of the drug was slightly more prompt in the cornea than in the conjunctiva. Representative anterior segment photographs of VKC and GVHD patients before and after tacrolimus treatment are shown in Figs. 3 and 4.

Palpebral conjunctival photo of a 14-year-old vernal keratoconjunctivitis patient. (A) Before treatment. Injected, engorged, and active giant papillae were noted. (B) After eight weeks of treatment, the active lesions look improved. (C) After six months of treatment. Giant papillae are flat and pale. The morphology of the papillae has changed, becoming reminiscent of a fibrotic scar.

Corneal photo of 33-year-old graft versus host disease patient. (A) Prior to treatment, a large-sized corneal epithelial defect was noted. (B) After eight weeks of treatment, corneal lesions were more obviously improved.
Prior to treatment with tacrolimus ointment, the instillation frequency of topical steroid was 4.3 ± 3.13 per day, but it could be discontinued at week eight after the beginning of treatment (p = 0.0078).
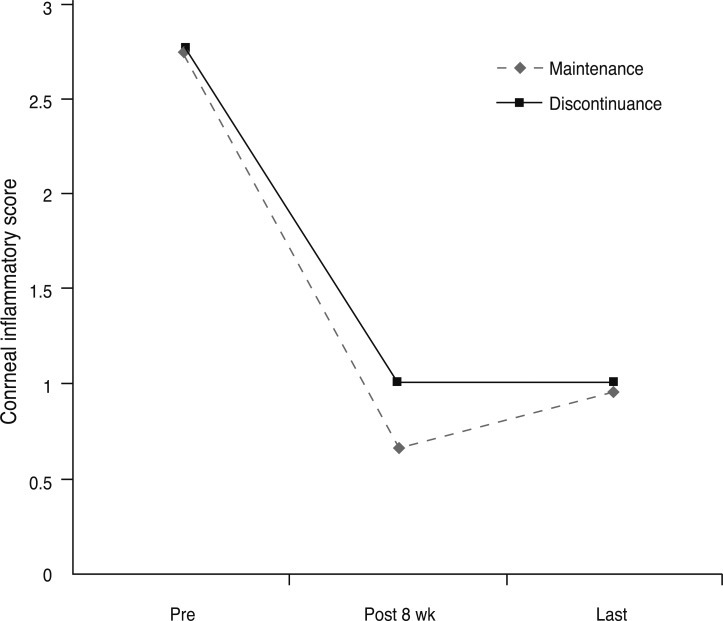
No difference in the clinical response was noted between VKC and GVHD patients at every follow-up visit (adjusted p > 0.05) (Figs. 5 and 6). Also, we compared the maintenance group and the discontinuance group, and noted no differences at pretreatment, week eight, and final follow-up at six months (adjusted p > 0.05) (Figs. 7 and 8).

The conjunctival inflammatory score change according to the diagnosis. No differences were noted to exist between vernal keratoconjunctivitis (VKC) and graft versus host disease (GVHD) at each time point (p > 0.05). Pre = pretreatment; Post = posttreatment.

The corneal inflammatory score change according to the diagnosis. We noted no differences between vernal keratoconjunctivitis (VKC) and graft versus host disease (GVHD) at each time point (p > 0.05). Pre = pretreatment; Post = posttreatment.
The conjunctival inflammatory score change according to maintenance. At the final follow-up, no differences were noted between the maintenance group and the discontinued group (p > 0.05). Pre = pretreatment; Post = posttreatment.
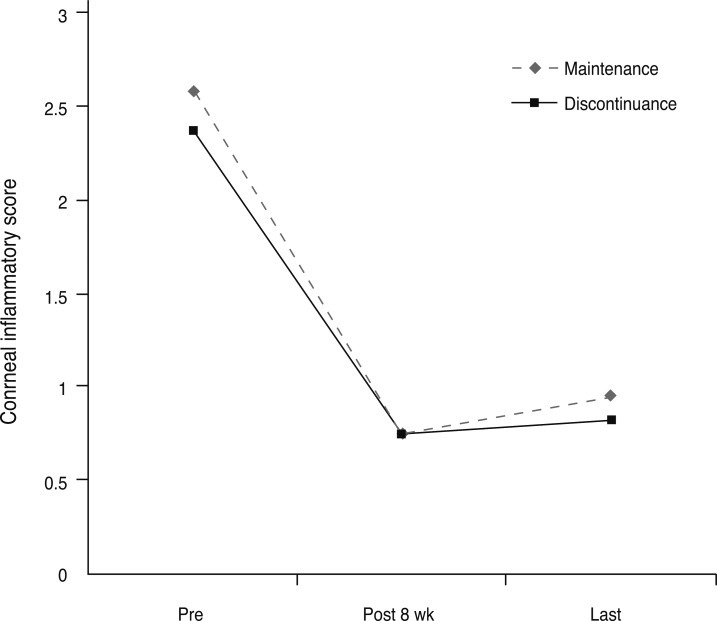
Corneal inflammatory score change according to maintenance. At the final follow-up, no differences were noted in the maintenance group and discontinued group (p > 0.05). Pre = pretreatment; Post = posttreatment.
Burning sensation in the eyelids and conjunctiva was observed in nine of 16 patients (56.3%). However, the majority of the patients reported that this effect was tolerable and disappeared after one to two weeks of continuous use.
Discussion
The present study proves that Tacrolimus 0.03% ointment is beneficial in severe VKC and chronic GVHD cases. Tacrolimus has a potent anti-inflammatory effect, and it is widely used for atopic dermatitis in dermatology departments. A literature search revealed few studies regarding the use of tacrolimus in ophthalmology applications and no study sought to determine the duration for which the ointment should be used. As we closely monitored the status of inflammation prior to and after treatment on a weekly basis, we were able to precisely determine the time at which the treatment begins to take effect, and also at what point treatment should be discontinued. All these findings are reported for the first time in the context of the use of tacrolimus in ophthalmology.
The Food and Drug Administration approved tacrolimus ointment for the treatment of moderate to severe atopic dermatitis [8]. Tacrolimus is available as 0.1% and 0.03% skin ointments. We chose the lower 0.03% tacrolimus concentration in this study as ocular absorption was theorized to be higher than cutaneous absorption.
Tacrolimus acts by blocking calcineurin, which is required for nuclear factor of activated T-cell-dependent T-cell activation or the induction of inflammatory cytokine arrays [11,13]. Though the mechanism of action is similar to its predecessor cyclosporine, it is more potent than the later in inhibiting calcineurin phosphtase [14]. The immune-suppressive effects of tacrolimus are not limited to T-lymphocytes alone, but also acts on B-cells and mast cells [15,16]. The rationale behind using tacrolimus was its higher potency than cyclosporine. Due to its lipophilic nature and high molecular weight, tacrolimus should penetrate the corneal epithelium with some difficulty [17]. On the other hand, the conjunctiva is up to 20 times more permeable to lipophilic and high molecular weight drugs [18]. Owing to these drug characteristics, we anticipated that the patients with conjunctival inflammatory conditions will respond better to topical tacrolimus than should patients with inflammatory conditions, such as penetrating keratoplasty rejection and uveitis. However corneal lesions demonstrated a faster response in one week than conjunctival lesions, which took two weeks for significant response (Figs. 1 and 2). We thought it would take more time for conjunctival improvement, because the lesions of the conjunctiva were more severe than that of the cornea both in GVHD and VKC patients.
Prior to undertaking this prospective study, we performed a pilot study on another group of VKC and GVHD patients. According to the results of our unpublished data, the use of topical tacrolimus resulted in a statistically meaningful reduction of inflammation in the initial four weeks of the after-application period, but there was very slow improvement in the later four weeks. Thus, from the prospective designing stage of the present research, we decided to observe the inflammation progress for at least an eight-week period following its application.
No score differences in corneal and conjunctival inflammation were noted according to the type of disease. Accordingly, it became apparent that tacrolimus ointment reacted well in both VKC and GVHD disease conditions, and no distinctions could be detected between the disease groups (Figs. 5 and 6).
On comparing the maintenance and discontinuance groups, no difference was detected between the groups over the next four-month observation period (Figs. 7 and 8). Considering this and the off-label use of tacrolimus ointment, we recommend a two-month schedule of tacrolimus, although additional and long-term studies with larger population concerning the valid application/discontinuation period are warranted at this point. However, as shown in Fig. 3, the six-month application of tacrolimus ointment to VKC patients resulted in giant, flat, pale papillae, which subsequently assumed a morphology reminiscent of a fibrotic scar. The long-term use of the ointment may alter the shape of these giant papillae, and such effects are likely to yield positive results for the future treatment of VKC patients.
This dermatologic formulation yields a viscous, stiff ointment which can be difficult for patients to use on the ocular surface [19]. According to the dermatological reports, serious adverse effects are recurrent herpetic lesions and skin cancer [20].
According to Joseph et al. [9] there is an increased risk of human simplex virus keratitis associated with topical tacrolimus use, so patients with atopic keratoconjunctivitis or previous history of herpes infection should be monitored carefully. In our study, we observed no herpetic keratitis. However, caution must be taken when positing herpetic keratitis as a possible complication. Another study found that 13% of atopic keratoconjunctivitis patients developed herpes simplex virus keratitis [21]. In a case series by Miyazaki et al. [11], tacrolimus was effective in patients with peripheral ulcerative keratitis and atopic keratoconjunctivitis without any adverse effects and elevation of IOP similar to our study.
Additionally, this research faced limitations in recruiting and maintaining a sufficient number of patients, as it involved the use of an unapproved ointment. Accordingly, only a limited number of patients participated in this experiment and the experiment could not continue for a sufficient period; therefore, long-term observations were not feasible. Such circumstances require further verification of the effectiveness of the present research via future large-scale experiments. This study is based on the subjective judgment of an observer; going forward future studies should require a more objective test result like a tear break-up time, Shirmer test, and impression cytology.
Also, this ointment is approved only for dermatologic use, hence this study is limited to being an off-labeled test and this formulation is not suitable for long term ocular use. However, previous studies support evidences of using it to treat various ophthalmic diseases [9-11]. Previously, tacrolimus eye drops have been used as an in-hospital prescription, and it was evaluated by Fujisawa Healthcare in clinical trials for VKC [11,22]. Therefore, we can expect more extensive use of the tacrolimus agent for ophthalmic applications in the future.
As per Food and Drug Administration guidelines, tacrolimus should be utilized only for short periods, it should be avoided in patients with compromised immune systems, and a minimum quantity necessary to control the patient's symptoms should be applied. However, topical tacrolimus is a very effective medication for immuno-mediated anterior segment inflammatory disease. The clinical improvement of the patients was better than when they received steroid therapy and it was well sustained after the steroid was discontinued. Therefore, it appears that topical tacrolimus, despite its limitations, may in many cases prove to be an effective substitute for topical steroid treatments.
Notes
No potential conflict of interest relevant to this article was reported.