Keratoconus is the noninflammatory progressive corneal thinning that is often of unknown etiology and is characterized by steepening and paracentral thinning, which results in irregular astigmatism and progressive myopia and this eventually leads to a decrease in visual acuity [1-3]. As these patients age, the probability of developing cataract increases, and cataract surgery may eventually be necessary. Performing cataract surgery in patients with keratoconus is very challenging due to the inaccuracies in calculating the intraocular lens (IOL) power. Current methods that are used to determine the IOL power may not be adequate for patients with keratoconus since their eyes have irregular, high astigmatism and an increased axial length [4]. Furthermore, IOL calculations are less accurate in patients with moderate to severe keratoconus than in those with mild keratoconus [5].
The following is a case report of a patient with severe keratoconus and cataract who had underwent cataract surgery after the implantation of keraring intracorneal ring segments (Mediphacos, Belo Horizonte, Brazil). The uncorrected visual acuity (UCVA), best spectacle-corrected visual acuity (BSCVA) and keratometric values remained stable for one month following the operation, and the remaining spherical aberration was minimal.
Case Report
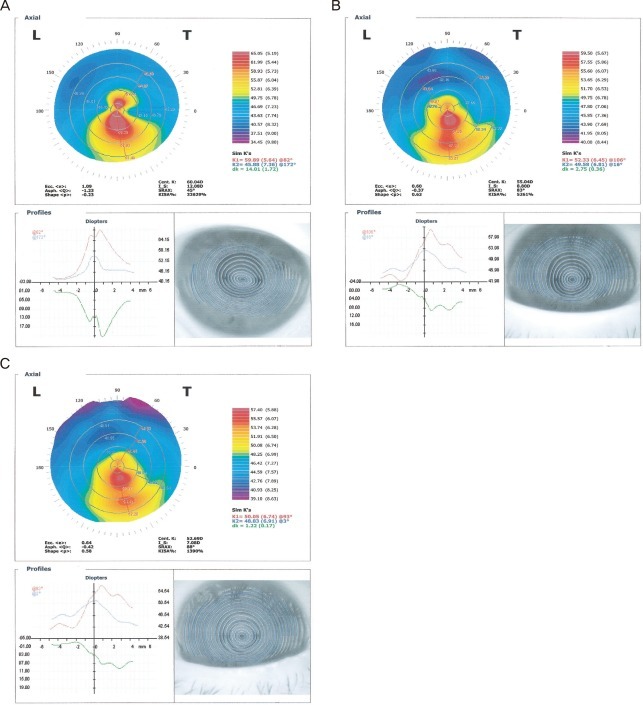
A 49-year-old man was referred to our clinic in September 2008 with a diagnosis of keratoconus and cataract. At that time, the manifest refraction values were 20 / 400 and 20 / 1,000, which yielded BSCVAs of 20 / 100 and 20 / 400, with manifest refractions of -5.00 -3.00 ├Ś 20┬░ and -8.00 -4.50 ├Ś 160┬░ in the right and the left eyes, respectively. Ultrasonic pachymetry was 433 ┬Ąm in the right eye and 398 ┬Ąm in the left eye. Keratometric readings were K1 = 61.15 ├Ś 105┬░ / K2 = 51.44 ├Ś 15┬░ for the right eye and K1 = 59.88 ├Ś 82┬░ / K2 = 45.88 ├Ś 172┬░ for the left eye. The axial length was 24.92 mm in the right eye and 25.09 mm in the left eye. Corneal topography (CT-1000; Shin-Nippon, Tokyo, Japan) was performed and showed characteristic keratoconus of 60.04 diopter (D, central K) and 32,629 (KISA%) (Fig. 1A). Grade 3 nucleosclerosis and cortical opacity were also noted in the left eye.
The keraring implantation on the left eye was carried out under sterile conditions and topical anesthesia in September 2008. The purkinje reflex was chosen as the central point and was marked with a Wavelength Allegretto Biomicroscope. A 5-mm marker was used to locate the exact ring channel. Tunnel depth was set as 75% of the thinnest corneal thickness on the tunnel location of the femtosecond laser.
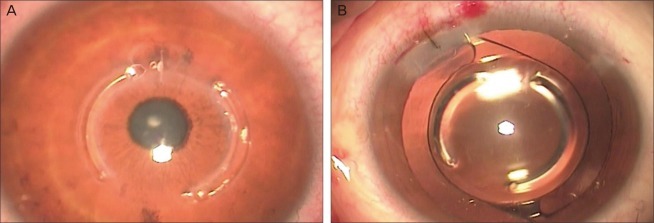
An incision was made on the steepest topographic axis. A 60-kHz femtosecond laser was used to create the ring channels. The inner diameter of the channel was set to 5.0 mm, and the outer diameter was set to 5.8 mm. The entry cut thickness was 1.20 ┬Ąm (at the steepest topographic axis), the ring energy that was used to create the channel was 1.40 ┬Ąj, and the entry energy was 1.40 ┬Ąj. Channel creation timing with the femtosecond laser was 10 seconds. An asymmetrical pair of kerarings was implanted immediately after the channel was created and before the disappearance of bubbles, which reveals the exact tunnel location. One segment was 250 ┬Ąm and the other segment was 150 ┬Ąm, and both were placed at 70┬░ (Fig. 2A). To avoid any injury to the incision site, we directly implanted the segment with the special keraring forceps. All of the procedures were uneventful.
The left eye was examined three months after implantation of the segments, in December 2008, and the results were UCVA of 20 / 100 and BSCVA of 20 / 50 with a manifest refraction of -4.00 -1.25 ├Ś 50┬░. The keratometric reading at this time was K1 = 52.33 ├Ś 106┬░ / K2 = 49.58 ├Ś 16┬░. The central keratometry reading shifted from 60.04 D to 55.04 D postoperatively (Fig. 1B).
Clear-cornea phacoemulsification and IOL implantation of the left eye were performed in December 2008. IOL power was calculated using standard keratometry and the SRKII formula. All of the procedures were uneventful (Fig. 2B). One month (January 2009) after the cataract surgery, the UCVA of the left eye was 20 / 30, and the BSCVA was 20 / 25 with a manifest refraction of -0.75 -0.75 ├Ś 10┬░. The keratometric reading was K1 = 50.05 ├Ś 93┬░ / K2 = 48.83 ├Ś 3┬░, and the postoperative central keratometric reading was 52.69 (Fig. 1C).
Discussion
Cataract surgery in patients with keratoconus is challenging due to the inaccuracies involved in estimating the IOL power in these patients who have irregular astigmatism and high myopia [4]. The authors have been disappointed in the refractive outcomes of the cataract surgeries that are performed on these patients, especially in those with moderate or severe keratoconus. The latest report shows that patients with mild keratoconus have a mean postoperative spherical aberration of -1.44 ┬▒ 1.69 D, which is significantly lower than those with moderate keratoconus, who have a mean postoperative SE of -5.85 ┬▒ 3.94 D (p = 0.05) [5]. Therefore, visual acuity or satisfaction after cataract surgery in patients with mild keratoconus are better than that in moderate and severe keratoconus.
This report demonstrates that cataract surgery after implantation of intracorneal ring segments is an effective treatment option in those with severe cases of keratoconus and cataract. The dramatic change in visual outcome and the stability of the results in terms of BSCVA and corneal topography after the keraring implantation and cataract surgery shows that this is a suitable and effective treatment for severe cases of keratoconus with cataract.
Keraring implantation has recently been proposed and investigated as an additive surgical procedure for all stages of keratoconus correction [6-9]. Kerarings are newly developed segments made of poly (methyl methacrylate) and are characterized by a triangular cross-section that induces a prismatic effect on the cornea. Their apical diameter is 5 mm, and the flat basis width is 0.6 mm with variable thickness (0.15 to 0.30 mm thickness with 0.5 mm steps) and arc lengths (90 degrees, 160 degrees, and 210 degrees). The optical zone that is provided by the keraring segments is 5.0 mm in diameter. Keraring is an efficient method for keratoconus correction, as it significantly decreases the SE by decreasing both the spherical and cylindrical components [10]. It also significantly decreases the keratometric values (Kmax, Kmin, and Kaverage) and significantly increases both the UCVA and BSCVA as well as improving the corneal topography [10-12]. When dealing with an irregular "asymmetrical" corneal surface, asymmetrical implantation provides better results by unequal flattening of the two opposite hemimeridians, as previously reported [7,8]. Also, Kwitko and Severo [13] have reported that the "central keratoconus group," which is also known as keratoconus with central cones, had significantly better results after symmetrical implantation. This is why we implanted asymmetrical kerarings in the left eye of our patient.
Sequential keraring implantation and cataract surgery have many advantages. First, the calculation of the IOL power can be more accurate due to the reduced astigmatism as a result of using the keraring. Intrastromal corneal ring segments have an "arc-shortening effect" on the corneallamellae and flatten the central cornea [14]. We used standard keratometry and the SRKII formula to perform the IOL power calculation. The standard and corneal topography-derived keratometry provide the most accurate IOL power when using the SRKII formula for patients with mild keratoconus, and no differences between standard and corneal topography-derived keratometry were not readily apparent [4,5]. However, the best method of measuring keratometry after a keraring implantation in a keratoconus individual has not yet been studied. Perhaps newer methods of evaluating corneal power, such as Scheimpflug photography and optical coherence tomography, will improve the accuracy of IOL calculation in the future.
Second, kerarings do not disturb the surgical field during the cataract operation. The main advantages of the intracorneal ring segments are that they are safe, reversible and stable [8].
Third, this procedure can allow severe keratoconous patients to delay or avoid penetrating keratoplasty altogether [6]. Due to the severity of our case, we believe the only treatment alternative would have been to perform a penetrating keratoplasty along with the cataract surgery. Penetrating keratoplasty is an invasive surgical option that has been associated with unpredictable refractive outcome, induced irregular astigmatism, graft rejection, shortage of suitable donor tissue, recurrence of keratoconus in the donor graft, and development of cataract or glaucoma, which makes it a suboptimal treatment [15,16]. However, prospective, randomized studies are needed to validate intracorneal ring implantation as an alternative to corneal grafting in cases that have both severe keratoconus and cataract.
Although our case has the limitation of having only a four month follow-up period after keraring implantation and a short observation period, this single case constitutes an example of the role this procedure may play in the treatment of patients that have keratoconus and cataract. Therefore, we suggest cataract surgery implantation of the intracorneal ring segment to be included in the treatment protocol for those with severe keratoconus and cataract, as it has fewer complications and provides a more accurate calculation of the IOL power.



 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print






