Various mechanisms have been reported as causes of late the laser in situ keratomileusis (LASIK) flap dislocations. The majority of them are blunt injuries, which are strong enough to threaten the integrity of the potential space of the LASIK interface in the eye [1]. This article presents a case of interface-captured foreign bodies after a mild traumatic scratch without any sign of flap displacement four years after LASIK surgery in the subject. The case was successfully managed by flap lifting and foreign body removal using interface irrigation.
Case Report
A 38-year-old woman underwent uneventful bilateral LASIK eye surgery with a superior hinge in August of 2005. The preoperative refraction was -6.25 Ds -0.75 Dc Ax 15 in the right eye and -3.00 Ds -0.75 Dc Ax 10 in the left eye. The procedure was performed using the Moria M2 microkeratome with bilateral 120 ┬Ąm LASIK flaps and NIDEK EC-5000 excimer laser. The ablation depth was 56.00 ┬Ąm in the right eye and 53.20 ┬Ąm in the left eye. The postoperative uncorrected visual acuity (UCVA) was 20 / 20 in both of the patient's eyes. The patient did not report any systemic disease, allergy or medication history. Four years after initial surgery, the right eye of the patient was scratched by a tree sprig during recreational mountain climbing. She did not wear protective goggles or glasses during mountain climbing. One morning after the accident, the patient visited the emergency room due to severe ocular pain and photophobia, as well as decreased visual acuity.
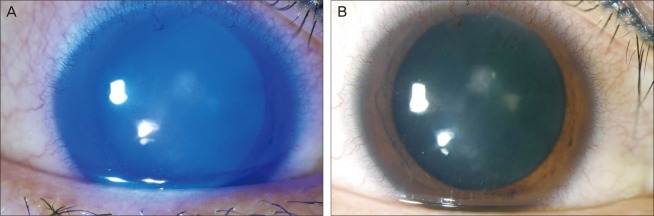
On examination, the UCVA was 0.125 in the right eye of the patient. Slit-lamp microscopy showed diffusely distributed opacities with crystalline materials in the LASIK interface (Fig. 1A and 1B). Fluorescein staining revealed a 3 ├Ś 1 mm sized corneal epithelial defect and surrounding linear infiltration without any displacement of the LASIK flap. No anterior chamber reactions were noted. Considering the patient's history of trauma from organic plant matter, the epithelial defect with infiltration was suspected of flap infection. Accordingly, smears and cultures were taken around the base and margin of the corneal epithelial defect. No microorganisms were identified with Gram or Giemsa stains and potassium hydroxide wet mounts. Medical treatments with broad-spectrum antibiotics, including moxifloxacin 0.5% (Vigamox; Alcon Laboratories, Fort Worth, TX, USA) and tobramycin 0.3% (Tobra; Daewoong, Seoul, Korea) were applied every hour with systemic intravenous third generation cephalosporin.
On hospital day two, the patient developed diffuse cornea edema. The UCVA in her right eye decreased to 0.02. The corneal epithelial defect was completely healed with stationary diffuse stromal opacities at the LASIK interface. The amount of crystalline materials had not increased. The next morning, the amount of crystalline materials was stationary, but the shape and the distribution of the materials had changed. The materials seemed to have rotated in a counterclockwise direction (Fig. 1C and 1D). Furthermore, culture results revealed no growth of microorganisms after 72 hours. Accordingly, these findings confirmed that the crystalline materials were foreign bodies rather than a sequela of infectious keratitis.
Surgery to remove the foreign bodies was performed under topical anesthesia. After placement of alignment markings, the lamellar flap was lifted with a spatula without difficulty. The stromal bed and lamellar flap were explored. Multiple crystalline foreign bodies were found and grasped from the stromal bed and undersurface of the lamellar flap with fine corneal forceps. Re-cultures were taken from the stromal bed and foreign bodies using sheep blood agar, chocolate agar, Sabouraud dextrose agar, and thioglycollate broth. After sufficient irrigation with balanced salt solution, no crystalline materials were found on the stromal bed or beneath the flap. The corneal alignment markings were checked to assure correct positioning of the flap. To prevent flap wrinkles, the corneal flap was wiped with a moistened microsurgical sponge and given three minutes to ensure flap adhesion.
On the first postoperative day, the patient's UCVA was 0.03 and she reported decreased corneal irritation. On examination, her cornea showed slightly decreased interface opacities with cleared crystalline debris (Fig. 2A and 2B). On postoperative day three, culture results from specimens taken in the operating room revealed a species of Staphylococcus epidermidis that was sensitive to ciprofloxacin. Accordingly, treatments of topical tobramycin ceased, moxifloxacin continued, and topical prednisolone acetate 1% (Pred Forte; Allergan, Irvine, CA, USA) was added four times a day. One month after surgery, the patient's UCVA was 0.8 with cleared LASIK interface. No signs of epithelial ingrowth or flap striae were noted.
Discussion
The LASIK interface between the flap and stromal bed is a relatively vulnerable area because there is minimal wound healing except at the edges of the flap [2]. The longest period of time between initial surgery and traumatic flap complication previously reported was seven years after an uneventful LASIK correction [3]. If flap dislocation occurs, several complications such as infective keratitis, diffuse lamellar inflammations, and epithelial ingrowth may exacerbate the condition and threaten the vision of subjects [4,5].
Many cases have been reported regarding late onset flap dislocation and related problems [1-3]. To our knowledge, however, this is the first case report of interface-captured foreign bodies after a mild corneal scratch without any sign of flap displacement. The foreign bodies were associated with Staphylococcal keratitis
In this case, the crystalline materials at the LASIK interface occurred with signs of infection (specifically, an epithelial defect with surrounding infiltration). No flap dislocation was noted. Hence, it was not clear whether the crystalline materials were foreign bodies or a sequela of infective keratitis. Because the distribution of the materials rotated in a counterclockwise direction three days after the initial trauma, the change confirmed that the materials were foreign bodies rather than inflammatory sequela. The reason that the distribution changed seems to be related to the gradual weakening of the adhesive force of the stromal lamellae by inflammatory reactions in the interface.
Three days after the insult, surgical flap lifting with irrigation was performed. A study by Chang et al. [6] reports that any early flap lift and repositioning performed within three days of the onset of symptoms may be associated with better visual outcome in the treatment of infections following LASIK. Some foreign bodies, such as certain metals and vegetable materials, are highly inflammatory. Accordingly, the risk of microbial contamination should be assessed especially carefully in foreign body-related injuries. In this case, the crystalline foreign bodies seemed to be the source of inflammation. After removal of the foreign bodies, the inflammatory reaction rapidly subsided. In this case, further analysis of the foreign particles could not be performed because the amount of foreign materials was limited. After the smears and cultures were done at the LASIK interface, additional sample material could not be collected.
The mechanism of how the foreign bodies get into the LASIK interface without apparent flap dislocation is still unknown. A study by Maurice and Monroe [7] reveals that the adhesive force of healed stromal lamellae is approximately one-quarter to one-half of the adhesive force of normal stromal lamellae. Thus one possible explanation is that among the various mechanisms of late LASIK flap dislocations previously reported [1], a sharp ocular trauma with high velocity may open the potential space and leave foreign body debris at the LASIK interface, even if the force is not strong enough to dislocate the LASIK flap.
This case has several interesting clinical implications. Mild traumatic corneal insults, such as scratches, may threaten the integrity of LASIK interface, as well as introduce infective keratitis up to several years after initial surgery. Further, any subsequent inflammatory reaction at the interface may weaken the adhesive force of the flap interface. In addition, if foreign bodies are suspected to be the cause of an inflammatory reaction, early flap lifting with irrigation is imperative to prevent further complications, including the progression of infective keratitis, epithelial ingrowth, and diffuse lamellar keratitis.




 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print






