Frontoethmoidal Mucocele Presenting as Progressive Enophthalmos
Article information
Abstract
In this case report we describe a 27-year-old man who presented with progressive enophthalmos for 5 months without any other associated ocular symptoms such as pain, diplopia, or visual disturbance. Computed tomography showed that his progressive enophthalmos originated from a frontoethmoidal mucocele and this caused destruction of the lamina papyracea and shrinkage of the ethmoidal air cell. Finally the enlarged orbital space caused an inward deviation of the eyeball. Endoscopic marsupialization was successfully performed by an otolaryngologist and did not result in any ophthalmologic sequelae. Although frontoethmoidal sinus mucoceles mostly frequently originates from orbital mucoceles, enophthalmic manifestations are very rare. Enophthalmic conditions are not as responsive to surgical interventions as exophthalmic conditions.
For patients presenting with enophthalmos, it is important to consider a broad differential diagnosis, including orbital trauma, chronic sinusitis, malignant infiltration, contracture and atrophy of the orbital contents (e.g., Wegener's granulomatosis, external beam irradiation, sclerosing orbital tumor, etc.), systemic inflammation (scleroderma) and pseudoenophthalmos [1]. Very rarely, silent sinus syndrome arising from chronic maxillary sinusitis is related to progressive enophthalmos and hypoglobus [2]. A few recent case reports have described ethmoidal involvement in silent sinus syndrome and the patients described had enophthalmic conditions that did not improve after functional endoscopic surgery [3,4]. Frontoethmoidal mucoceles are relatively rare and in some cases patients experience ophthalmic manifestations, including orbital displacement, proptosis, restricted ocular movement, diplopia and eyelid swelling [5]. We encountered an unusual case of frontoethmoidal mucocele that initially presented as progressive enophthalmos, yet there was no symptomatic improvement following successful endoscopic marsupialization.
Case Report
A 27-year-old man visited our ophthalmology clinic for an evaluation of the enophthalmos of his right eye that had worsened over the previous 5 months. He had no significant history of systemic or ocular disease, previous trauma, sinus diseases or surgery. The patient denied clinical symptoms such as pain, diplopia, or visual changes. The ophthalmic examination showed that his best-corrected visual acuity was 20 / 20 in both eyes. The pupillary light reflex showed equal reactive size with no afferent pupillary defect in both eyes. The ocular alignment examination showed that his ductions were full, his primary alignment was orthophoric and there were no deviating lesions.
The Hertel exophthalmeter examination with a base of 96 mm showed 10.0 mm in his right eye, and 14.0 mm in his left eye. The intraocular pressure was 16 mmHg in his right eye and 13 mmHg in his left eye. A computed tomography scan revealed a large filling lesion of soft tissue density in the right frontal and ethmoid sinuses, which possibly originated from a mucocele. A magnetic resonance image showed a lesion that had T2 low signal intensity and T1 high signal intensity, which may have been due to protein content and a chronic state of sinusitis, suggesting that it was most likely a frontoethmoidal mucocele (Fig. 1). We concluded that this lesion was a chronic mucocele and we referred the patient for otolaryngologic consultation.
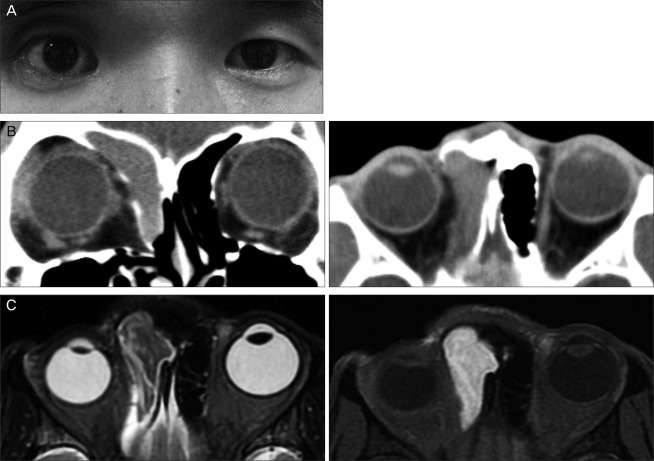
(A) Preoperative view of a 27-year-old man with right frontoethmoidal mucocele. Note the marked enophthalmos of right globe. (B) Preoerative computed tomography imaging: note the large right space occupying lesion from the frontal sinus extending toward ethmoid sinus. A destructive lesion of the lamina papyracea was found in the coronal view. (C) Preoperative magnetic resonance image imaging: the lesion showed T2 low signal intensity and T1 high signal intensity, which reflected the chronic state of frontoethmoidal mucocele.
The otolaryngologist performed endoscopic sinus drainage surgery during which a bulging mococele that originated from the right frontal sinus and extended toward the anterior ethmoidal sinus; this mucocele was filled with a white to yellowish mucous discharge. The lamina papyracea had a nearly total bony defect, but the orbital muscle was not exposed. All of the mucous material was removed by curved suction and part of the middle turbinate was resected using straight cutting and the mucosal cavity was enlarged by marsupialization.
Eight months after surgery, the lesion was completely resolved, but the patient still complained of an enophthalmic condition (Fig. 2). At that time, the Hertel examination with the same base (96 mm) showed 11.0 mm in his right eye and 14.0 mm in his left eye, including that a 3.0 mm enophthalmic condition remained. We discussed the need for orbital reconstruction with the otolaryngologist, but we collectively decided not to perform additional ocular reconstruction surgery because we were concerned that the ocular reconstructive material might result in a recurrent mucocele [6,7]. Institutional review board approval was obtained in Seoul St. Mary's Hospital.
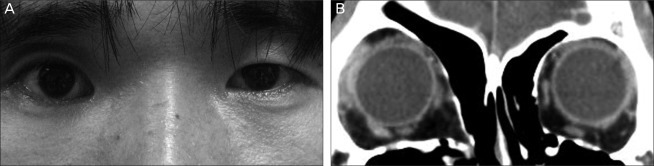
(A) Postoperative view after 8 months showed that 3.0 mm enophthalmos of the right globe still remained. (B) Postoperative computed tomography imaging at same time showed resolution of the bony pseudocapsule and reformation of the orbit, which resulted in the deviation of right medial wall toward the ethmoidal sinus.
Discussion
Frontoethmoidal mucoceles are cystic, slowly expanding lesions that usually originate from the frontal or ethmoidal sinuses. They may also involve the orbital space and cause a downward and lateral globe displacement with proptosis [5]. These mucoceles may be accompanied by ophthalmic manifestations such as displacement of the eyeball, proptosis, restricted ocular movement, diplopia, lid swelling, chemosis, optic neuropathy, decreased vision and increased intraocular pressure [8-10]. More rarely, a frontoethmoidal mucocele may be accompanied by "dynamic proptosis" which presented spontaneous and dynamic proptosis in both eyes, pulsatile in nature [11]. To our knowledge, however, this is the first case of frontoethmoidal mucocele presenting with an enophthalmic condition that gradually worsened over 5 months, which was not recovered frorn a successful endoscopic surgery.
Following endoscopic or external surgical removal of most of the frontoethmoidal mucoceles that has orbital involvement, most patients show a good recovery and improvements of their ophthalmic symptoms such as proptosis, limitations in eye-movement, and increased intraocular pressure [6,8-10]. Patients presenting with an enophthalmic condition, however, do not show symptom improvement after successful sinus surgery [5,9,10]. Ophthalmic enophthalmic conditions are usually caused by orbital blow out fractures, which result in enlargement of the orbital space [1]. In our patient, the bulging frontal sinus mucocele grew toward the ethmoidal sinus, destroying the lamina papyracea, and the ethmoidal air cells became hypoventilated. The frontal sinus mucocele finally resulted in ethmoial atelectasis. During this time, the enlarging the orbital space and the deviated medial wall bony component made the eyeball deviate inward, similar to the effect of a right orbital medial wall fracture. These ethmoidal bony defects and the shrinkage of ethmoidal air cells were confirmed by the otolaryngologist who performed the functional endoscopic surgery.
Enophthalmos of a sinus origin is associated with silent sinus syndrome and this is an uncommon condition. It usually presents with progressive enophthalmos and hypoglobus due to the gradual collapse of the orbital floor and with opacification of the maxillary sinus that is then followed by subclinical maxillary sinusitis [2]. Patients with ethmoidal silent sinus syndrome have recently been described in other studies; in these patients, enophthalmos resulted from the negative pressure in the anterior ethmoidal air cells on the defective side, and this increased orbital volume and markedly reduced the sinus volume [3,4].
The cosmetic problems of patients with enophthalmos may be corrected by orbital reconstructive surgery. In our patient, this would have consisted of reduction of the intraorbital contents and insertion of alloplastic material into the right medial wall, which had been almost totally destroyed by the melting effect of the sinus mucocele. But the orbital reconstructive material can cause recurrent sinus mucoceles by blocking the outflow of sinus mucous material [6,7]. Thus, after consultation with the patient's otolaryngologist, we concluded that an additional operation should await improvements of the symptoms.
Most patients with ocular symptoms associated with sinus mucocele show good recovery after correction of the sinus lesion [9,12]. We encountered a patient with enophthalmos associated with a frontoethmoidal mucocele. However, the patient's symptoms were not recovered after successful surgical removal of the mucocele.
Notes
No potential conflict of interest relevant to this article was reported.