Spontaneous Resolution of Intravitreal Steroid-Induced Bilateral Cytomegalovirus Retinitis
Article information
Abstract
A 73-year-old woman underwent vitrectomy and intravitreal triamcinolone acetonide (IVTA) of the right eye and cataract surgery with IVTA of the left eye, for bilateral diabetic macular edema. The patient presented with visual loss in both eyes three-months postoperatively. The fundoscopic examination revealed white-yellow, necrotic peripheral lesions in the superotemporal quadrant of both eyes. Although bilateral acute retinal necrosis was suspected, azotemia resulting from diabetic nephropathy limited the use of acyclovir. Antiviral treatment was not started. A sample of the aqueous humor for polymerase chain reaction (PCR) analysis was obtained. One week later, the PCR results indicated the presence of cytomegalovirus (CMV). Since the retinal lesions did not progress and did not threaten the macula, the patient was followed without treatment for CMV. The retinal lesions progressively regressed and completely resolved in both eyes by six months of follow-up. Patients with IVTA-induced CMV retinitis may not require systemic treatment with ganciclovir.
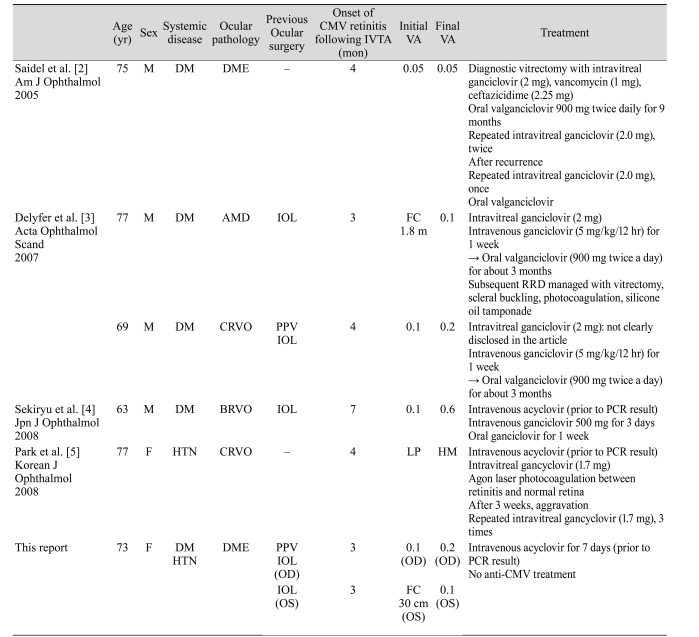
Cytomegalovirus (CMV) retinitis is the most common opportunistic ocular infection in immunocompromised patients [1]. However, CMV retinitis can develop in immunocompetent patients after an intravitreal triamcinolone acetonide (IVTA) or after implantation of fluorocinolone acetonide [2-6]. All patients with such problems have been successfully treated with intravitreal and/or intravenous, and oral administration of ganciclovir (Table 1). Spontaneous resolution of CMV retinitis has been reported in infants with congenital infection and in patients receiving highly active antiretroviral therapy (HAART); however, spontaneous resolution has not been previously reported in a patient with intravitreal steroid-induced CMV. Here we report such a case [7,8].
Case Report
A 73-year-old woman with a history of well-controlled type 2 diabetes mellitus and hypertension presented to the clinic with visual loss in both eyes in July 2008. The vision was 20 / 200 in both eyes. There were no other abnormalities in the anterior segments of the eyes, other than visually significant cataracts, bilaterally. The fundus examination with the indirect ophthalmoscope revealed the presence of a moderate nonproliferative diabetic retinopathy and macular edema in both eyes. Optical coherence tomography showed macular thickening in both eyes with a taut posterior hyaloid membrane of the macula in the right eye. In July of 2008, phacoemulsification and intraocular lens implantation were performed, as well as vitrectomy with removal of the posterior hyaloid and internal limiting membranes, as well as endolaser treatment of the right eye. At the end of the vitrectomy, IVTA (4 mg) was administered. One week later, phacoemulsification, intraocular lens implantation, and IVTA administration (4 mg) were performed on the left eye. The postoperative clinical course was fair. In August of 2008, the vision improved slightly to 20 / 100 with improvement of the macular edema in both eyes.
Three-months later, in October of 2008, the patient presented with 'cloudy vision' in both eyes that developed two weeks previously. The visual acuity was 20 / 200 in the right eye and counting fingers at 30 cm in the left eye. The intraocular pressure (IOP) was 30 mmHg in the right eye and 42 mmHg in the left eye. The slit lamp examination demonstrated fine keratic precipitates of the corneal endothelium, 3+ inflammatory cells, 2+ flare in the anterior chamber, and moderate vitreous haze in both eyes. The fundus examination revealed white-yellow, necrotic peripheral retinal lesions in the superotemporal quadrant of both eyes (Fig. 1A and 1B).

(A,B) A 73-year-old woman, who underwent vitrectomy with intravitreal triamcinolone acetonide (IVTA) in the right eye and cataract surgery with IVTA in the left eye for bilateral diabetic macular edema, presented with visual loss in both eyes at three months post surgery. The fundus examination revealed white-yellow, necrotic peripheral lesions in the superotemporal quadrant of both eyes. The clinical impression was bilateral acute retinal necrosis. (C,D) Aqueous humor analyzed by polymerase chain reaction. The results were available seven days later and demonstrated the presence of cytomegalovirus. Meanwhile, despite no specific anti-cytomegalovirus treatment, the peripheral retinal lesion did not progress, and did not threaten the macula in both eyes. The patient was followed closely. (E,F) Six months later, the retinal lesions regressed completely with subsequent development of pigmentary changes of both eyes. A mild vitreous haze was still present in the left eye.
As bilateral acute retinal necrosis was suspected, starting intravenous treatment with acyclovir was considered. However, the patient refused hospital admission and further treatment. Moreover, azotemia resulting from diabetic nephropathy limited the use of acyclovir. Therefore, antiviral treatment was not started and the patient was closely monitored. A diagnostic aqueous humor sample for polymerase chain reaction (PCR) analysis was obtained. PCR was carried out to test for varicella zoster virus, herpes simplex virus type 1 and 2, and CMV. Topical anti-glaucomatous and steroid medications were used for treatment.
The PCR results, available seven days later, confirmed the presence of CMV. The infectious disease consultant reported that systemic CMV infection was not possible and recommended antiviral therapy with ganciclovir for the CMV retinitis. However, one week had elapsed and the IOP and inflammatory reaction of the anterior chamber and vitreous had decreased, the peripheral retinal lesion did not increase, and the macula was not threatened in either eye (Fig. 1C and 1D).
The CMV retinitis was likely caused by the local (intraocular) immunosuppression caused by the IVTA and the immunosuppression might have reduced over time (already 3 months since the IVTA was administered in both eyes). The CMV retinitis did not threaten the macula. Since starting treatment with ganciclovir was not urgent, the patient was closely followed without any anti-CMV medications. The plan was close observation while maintaining the topical anti-glaucomatous and steroid therapy.
In November of 2008, two months after the initial presentation, the inflammatory reaction of the anterior chamber appeared to be resolved and the vitreous haze was much improved in both eyes. The IOP was 24 mmHg in the right eye and 28 mmHg in the left eye with topical application of timolol and dorzolamide. The necrotic retinal lesion regressed slightly without any progression of the margin of the lesion in both eyes.
In April of 2009, six months after initial presentation, the visual acuity was 40 / 200 in the right eye and 20 / 200 in the left eye. The anterior chamber reactions had resolved and the inflammatory retinal lesions regressed completely with the subsequent development of retinal pigmentary changes in both eyes. A mild vitreous haze was still present in the left eye (Fig. 1E and 1F).
Discussion
CMV is a ubiquitous infectious agent commonly found in the human population. Primary infection may produce mononucleosis-like symptoms. However, in immunocompetent individuals marked constitutional symptoms of infection are rare. CMV infection occurs in 4% of live-born infants and 50% to 80% of adults. Moreover, PCR-based studies indicate that some seronegative adults are chronic virus carriers [9-12]. The site of chronic infection continues to be debated. Sites reported have included monocytes [9], bone marrow-derived myeloid progenitors such as granulocyte-macrophage progenitor cells [13,14], endothelial cells and the smooth muscle cells of blood vessels [15-18]. In murine studies, the possibility of the retina as a site of chronic infections has been proposed [19]. However, Vogel et al. [20] showed that the human eye (retina) is not a specific site for chronic CMV and that CMV retinitis is more likely due to infiltration of virus-infected circulating cells during immunosuppression. It is assumed that CMV spreads hematologically (in mononuclear and polymorphonuclear leukocytes and/or endothelial cells) to infect the retina after reactivation [21,22]. Studies on patients with CMV retinitis have shown that retinal vascular endothelial cells can be infected with CMV in vivo. Therefore, it was assumed that CMV infected the retinal vascular endothelial cells, leading to infection of the surrounding glial and neuronal cells followed by the retinal pigment epithelium [23].
Considering the wide use of IVTA, CMV retinitis could become a not-so-rare, significant complication attributable to local immunosuppression. The clinical course of the case reported here suggests that systemic treatment with ganciclovir may not be mandatory; its use should take into consideration such factors as host immunity, macular involvement, the elapsed interval after IVTA, history of vitrectomy, and coexisting diabetic nephropathy, which can be aggravated by ganciclovir.
In previous reports, immunocompetent patients with CMV retinitis attributable to IVTA have been managed with intravenous ganciclovir similar to the treatment of immunocompromised patients (Table 1). However, the patient reported here was not treated with antiviral therapy. The IVTA-induced local (intraocular) immunosuppression was thought to decrease with time and that close observation without ganciclovir was appropriate in this patient; the intraocular concentration of triamcinolone is measurable for up to three months in the absence of a vitrectomy, and the elimination half-life would be much shorter in vitrectomized eyes after IVTA [24,25].
Immunity plays a significant role in the pathogenesis of CMV retinitis in patients with acquired immunodeficiency syndrome. Prior to the introduction of HAART, the treatment of CMV retinitis included an induction phase and maintenance phase with ganciclovir. Subsequently, prolonged use of ganciclovir was found to cause systemic adverse effects such as hematological abnormalities (neutropenia, thrombocytopenia and anemia) and renal impairment [26,27]. After the introduction of HAART with subsequent immune recovery, CMV retinitis may not recur even after maintenance anti-CMV therapy is discontinued. In addition, as this case illustrates, active CMV retinitis may spontaneously resolve in some patients that never receive specific anti-CMV treatment [28].
Notes
No potential conflict of interest relevant to this article was reported.