The Development of Recurrent Choroidal Neovascularization in a Patient with Choroidal Coloboma
Article information
Abstract
We report a case of recurrent choroidal neovascularization (CNV) in an eye with chorioretinal coloboma. A 36-year-old woman presented complaining of decreased visual acuity (VA) in her left eye. Best corrected visual acuity (BCVA) was 20/200 and iris coloboma was observed. Funduscopy and fluorescein angiography (FA) showed CNV in the superior extrafoveal region with chorioretinal coloboma reaching just inferior to the optic disc. No other cause for CNV was observed except for the chorioretinal coloboma. BCVA improved to 20/30 after laser photocoagulation. She revisited our clinic for deteriorating VA (20/400) in the same eye 3 years after treatment. Funduscopy and FA demonstrated recurrent CNV with subfoveal hemorrhage. Photodynamic therapy (PDT) was followed by three consecutive intravitreal bevacizumab injections (IVB) for the subfoveally-located CNV. However, the CNV persisted with the appearance of a fresh subretinal hemorrhage. Additional PDT was combined with IVB on the same day 6 months after the initial PDT. The CNV regressed 3 months after treatment and has not recurred as of 8 months after the last treatment. The patient's BCVA improved to 20/60. This case suggests that PDT combined with IVB can be an alternative treatment for the management of recurrent CNV after laser photocoagulation in eyes with chorioretinal coloboma.
Choroidal coloboma results from incomplete closure of the embryonic fissure. Choroidal neovascularization (CNV) secondary to choroidal coloboma usually develops at the edge of the coloboma and extends into the macula [1,2]. We report a case of choroidal coloboma with CNV that initially developed in the superior extrafoveal macular region and recurred 3 years after thermal laser photocoagulation. The recurrent CNV was successfully treated by combining photodynamic therapy (PDT) with intravitreal injections of bevacizumab (IVB).
Case Report
A 39-year-old woman was seen in our clinic due to decreased visual acuity in her left eye. Her best corrected visual acuity (BCVA) was 20/20 in the right eye and 20/200 in the left eye. She had unilateral coloboma in the iris, lens, and choroid. Her refractive error was -0.25 diopters spherical equivalent in both eyes. Fundus examination revealed a yellow ovoid lesion with subretinal fluid in the surrounding retina in the superior extrafoveal region distant from the choroidal coloboma (Fig. 1A). Fluorescein angiography (FA) revealed CNV with profuse leakage. Subretinal fluid was noted in the surrounding retina. No specific cause of CNV was noted except for the choroidal coloboma. The patient received direct thermal laser photocoagulation to the lesion and her BCVA subsequently improved to 20/30.
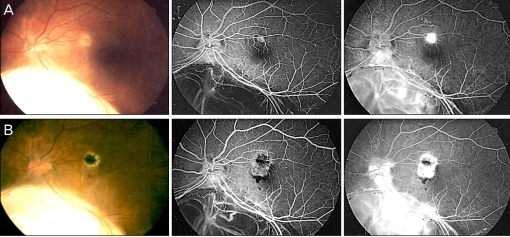
(A) Fundus photograph and fluorescein angiography showing an inferior choroidal coloboma with choroidal neovascularization and subretinal hemorrhage. (B) Fundus photograph and fluorescein angiography showing recurrent choroidal neovascularization around the previous laser scar.
The patient revisited our clinic because of a decrease in visual acuity to 20/400 in her left eye 3 years after the thermal laser photocoagulation. Fundus examination revealed recurrent CNV with subfoveal hemorrhage at the edges of the photocoagulation scars (Fig. 1B). We confirmed the recurrence of CNV by FA. PDT was followed by three consecutive IVBs at 6-week intervals because the recurrent CNV lesion involved a subfoveal region. However, the CNV persisted and a fresh subretinal hemorrhage developed (Fig. 2). The second round of PDT was combined with IVB on the same day at 6 months after the initial PDT. The CNV regressed 3 months after the second combined treatment and had not recurred as of 8 months after treatment (Fig. 2E and 2F). BCVA in the left eye had improved to 20/60 at the most recent visit, 13 months after initial therapy.
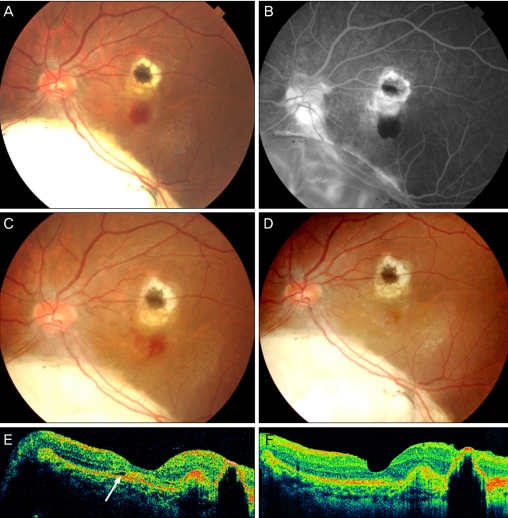
(A) Fundus photograph demonstrating the inferior choroidal coloboma with choroidal neovascularization (CNV), subretinal hemorrhage (SRH), and laser photocoagulation scarring. (B) Fluorescein angiography (late phase) showing hyperfluorescence from CNV. (C) Fundus photograph showing newly-developed SRH and CNV. (D) Fundus photograph showing fibrotic CNV scarring. (E) Vertically scanned image of Stratus OCT showing subretinal fluid (arrow). (F) Vertically scanned image of Cirrus OCT demonstrating resolution of the subretinal fluid.
Discussion
Choroidal coloboma is an inferiorly located congenital lesion characterized by absence of the normal retina, retinal pigment epithelium, and choroids. The pathogenesis of CNV secondary to choroidal coloboma has been speculated to be related to anatomic disruptions at the edge of the coloboma because the CNV usually occurs inferior to the fovea [1]. However, in this case, the CNV developed superior to the fovea, away from the coloboma. The presence of choroidal coloboma may induce ischemic conditions not only in the intercalary membrane [3] but also in the normal retina, which may facilitate the development of CNV. It is also possible that the CNV had an idiopathic origin because other causes of CNV, such as myopia and inflammation, were not noted.
In this study, CNV recurred 3 years after a good initial response to thermal laser photocoagulation. The recurrent CNV associated with the choroidal coloboma was successfully treated by combining PDT with IVB. Previous studies have reported that thermal laser photocoagulation is effective in treating CNV secondary to choroidal coloboma [1,4] and that PDT has good therapeutic efficacy in laser-induced or idiopathic subfoveal CNV [5]. Although the recurrent CNV in this patient did not respond well to PDT alone, the CNV subsided after combined treatment with PDT and IVB. This difficulty in treatment may be attributable to a defect in the macula. In summary, this case suggests that CNV associated with choroidal coloboma can develop away from the coloboma and that combining PDT with IVB may be beneficial for the management of recurrent CNV after thermal laser photocoagulation in patients with ocular coloboma.
Acknowledgements
This study was supported by grant from the Korea Healthcare Technology R&D Project (A080588), Ministry for Health, Welfare and Family, Republic of Korea.
Notes
No potential conflict of interest relevant to this article was reported.