 |
 |
| Korean J Ophthalmol > Volume 25(3); 2011 > Article |
Abstract
We investigated the case of a young man with blurred vision in his left eye. His visual acuity was slightly decreased, and ophthalmoscopy disclosed a gray-white lesion in the macula. He had no systemic or ocular history. On the visual field test, the threshold sensitivity was decreased in the corresponding region. Spectral domain optical coherence tomography (OCT) demonstrated a disruption in the photoreceptor inner and outer segment (IS/OS) junction and undulation of the retinal pigment epithelium (RPE) with backscattering. We re-examined the patient after two weeks and after three months without any treatment. Visual acuity and visual field results were gradually normalized, and OCT demonstrated the recovery of continuity in the photoreceptor IS/OS junction, as well as decreased RPE irregularity with minimal backscattering. We used spectral domain OCT instead of time domain OCT (OCT3) so that we could provide better image resolution of the acute retinal pigment epitheliitis (ARPE). Finally, we observed recovery of the functional and anatomical changes in the ARPE patient with a resolution of the condition within three months following the initial examination, using OCT and visual field tests.
Acute retinal pigment epitheliitis (ARPE) is a rare, self-limited macular disorder affecting healthy young adults [1-3]. Since 1972, when Krill and Deutman [1] first described ARPE as a subtle abnormality of the retinal pigment epithelium (RPE), several cases have been reported. The diagnosis of ARPE is made based on clinical suspicion, as well as fundus findings, which are characterized by the appearance of single or multiple dark gray pigmented spots surrounded by yellow-white haloes in the macular area at the level of the RPE. Some reports pertaining to ARPE have included other disease entities because ARPE has not been well described. Chittum and Kalina [2] attempted to define ARPE by describing its angiographic characteristics. More recently, Hsu et al. [3] first described the optical coherence tomography (OCT) findings in patients with ARPE. Herein, we describe the short-term serial changes in clinical features and Cirrus spectral-domain OCT (SD-OCT; Carl Zeiss Meditec, Dublin, CA, USA) findings in a patient with ARPE. Furthermore, we have identified the relationship between the functional and anatomical changes using visual field (VF) testing and SD-OCT.
An 18-year-old man was referred to our clinic for the evaluation of blurred vision involving the left eye that had manifested four days previous. He had no specific medical, ocular, or trauma history. He underwent a thorough ocular examination.
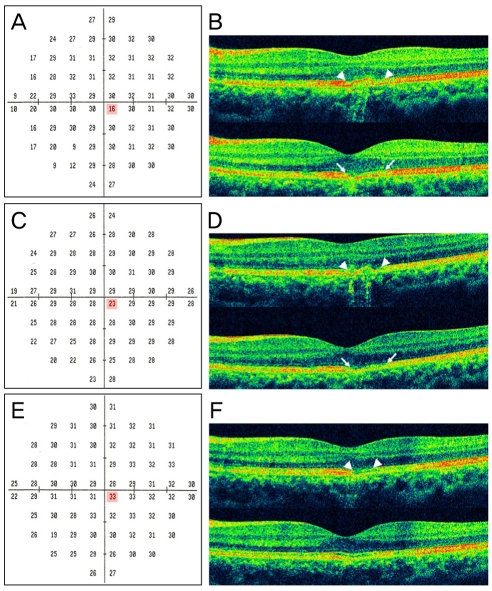
During his first visit, the subject's best-corrected visual acuity was 1.0 in the right eye and 0.9 in the left eye. The refractive error was -5.0 diopters in both eyes. The anterior segment ocular examination was normal. Ophthalmoscopy disclosed a gray-white lesion in the superior juxtafoveal region (Fig. 1A). On the VF test, the threshold sensitivity was decreased in the corresponding juxtafoveal region (Fig. 2A). VF (central 10-2 SITA-Standard strategy) was measured with a Humphrey Field Analyzer II (Zeiss-Humphrey, San Leandro, CA, USA) under continuous monitoring. The OCT demonstrated disruption in the photoreceptor inner and outer segment (IS/OS) junction and undulation of the RPE with backscattering (Fig. 2B). Two weeks later, the patient presented with a subtle improvement in symptoms. The visual field test revealed an increased threshold at the prior point (Fig. 2C), but the OCT findings did not reveal improvement compared to the initial findings (Fig. 2D). Three months later, the visual acuity had recovered to 1.0. The patient no longer complained of the previous symptoms. The lesion was diminished in size and intensity upon ophthalmoscopy (Fig. 1B). Visual field results were normalized (Fig. 2E). The OCT demonstrated a recovery of continuity in the photoreceptor IS/OS junction, as well as decreased RPE irregularity with minimal backscattering (Fig. 2F).
ARPE is an acute, transient, foveal disturbance of unknown cause and which affects young adults. Because of scarce case reports and an infrequent prevalence of the disease, the diagnosis can be difficult without suspicion. Fluorescein angiography (FA) is a critical test for the differential diagnosis of ARPE. Unfortunately, we could not obtain FA data because t he patient had signs of an anaphylactic reaction, such as dizziness and difficulty breathing, immediately after the fluorescein injection. Therefore, we made a diagnosis based on the fundus findings in combination with the OCT and other characteristics of the disease.
White dot syndromes, especially multiple evanescent white dot syndromes (MEWDS), should be considered in the differential diagnosis of ARPE. White dot syndromes are characterized by multifocal white lesions and are accompanied by mild vitritis [4]. Our patient was relatively young and had no signs of intraocular inflammation. MEWDS differs from ARPE in that the lesions are located outside the macula in the posterior pole, and electroretinogram (ERG) findings are abnormal [4]. The main lesions responsible for MEWDS cause damage to the photoreceptor outer segment but not the RPE [5]. In our case, there was a single white dot lesion that was limited to the juxtafoveal region; also, ERG, which was performed on the first visit, showed normal findings. In acute posterior multifocal placoid pigment epitheliopathy (APMPPE), multiple, large placoid lesions start in the posterior pole and extend to the post-equatorial fundus, often accompanied by prodromal flu-like symptoms. Our patient's lesions were discrete clusters of a few subtle, small grey spots that resolved without scarring within three months after onset. In contrast, the lesions in patients with APMPPE are replaced by RPE changes upon resolution [4]. The OCT demonstrated RPE involvement, which was similar to the previously reported OCT findings [3]. Based on these findings, other diseases were ruled out and the patient was diagnosed with ARPE.
Hsu et al. [3] first described the OCT findings of patients with ARPE using time domain OCT (OCT3; Carl Zeiss) as a hyper-reflectivity involving the outer nuclear layer, photoreceptor, and RPE. Hyper-reflectivity has not yet been evaluated with SD-OCT. In our case, we found a definite disruption in the IS/OS junction, as well as an undulation of the RPE according to SD-OCT. Because SD-OCT can provide better image resolution than OCT3, we believe that the disruption of the IS/OS junction with SD-OCT presented as a hyper-reflectivity of the outer retina with OCT3. As reported by Hsu et al. [3], the thickness of the hyper-reflectivity decreased with increased resolution, and we found a decreased length of the IS/OS disruption based on the serial observations of the OCT findings. The RPE irregularity also decreased as the symptoms improved and as the threshold of the visual field increased. On the basis of these findings, the morphologic changes in inflammation related to ARPE do not seem to be permanent.
Fig. 1
Fundus photographs of 18-year-old man. (A) A fundus photograph showed a gray-white lesion in the superior-juxtafoveal region. (B) Three months later, the lesion was diminished in size and intensity.

Fig. 2
Eighteen-year-old man: optical coherence tomography (OCT) and visual field. (A) The visual field revealed decreased threshold sensitivity in the macula. (B) OCT demonstrated disruption in the photoreceptor inner and outer segment junction and undulation of the retinal pigment epithelium (RPE) with backscattering. (C) Two weeks after onset, an increased threshold was revealed in the prior point. (D) OCT did not reveal any improvement compared to the initial findings. (E) Three months later, the visual field was normalized. (F) Recovered continuity in the photoreceptor inner and outer segment junction and decreased RPE irregularity with minimal backscattering were demonstrated upon OCT. To determine the serial changes in the lesion, OCT findings were obtained in the identical region of the macula. Acquisition photos were acquired with a five-line raster scan, which consists of five horizontal lines, separated from one other by 0.25 mm. We present only two lines of the raster scan because the other three raster scan lines showed normal findings.



 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print




