Effectiveness of Home-Based Pencil Push-ups (HBPP) for Patients with Symptomatic Convergence Insufficiency
Article information
Abstract
Purpose
To report the effectiveness of home-based pencil push-ups (HBPP) therapy for patients with symptomatic convergence insufficiency.
Methods
Data was collected prospectively on 16 patients who were diagnosed with convergence insufficiency beginning in January 2009. The study group was composed of ten male and six female patients. The duration of symptoms, refractive error, distant and near deviation angles, and near point of convergence (NPC) prior to and after 12 weeks of HBPP therapy were measured in all patients.
Results
The mean age of the patients was 19.3 years. The mean deviation angle of exophoria was 3 prism diopters (PD) at distant and 11.2 PD at near. The mean value of NPC prior to HBPP therapy was 36.3 cm; however, the near point of accommodation was within the normal range. After 12 weeks of HBPP therapy, the mean deviation angle of exophoria decreased to orthophoric at distant and 4 PD at near. The mean value of NPC decreased to 14.4 cm.
Conclusions
Twelve weeks of HBPP therapy appears to be an easy, cost-free and effective therapy for patients with symptomatic convergence insufficiency.
Convergence insufficiency is one of the most common causes of ocular discomfort and the most common cause of muscular asthenopia [1]. Symptoms of convergence insufficiency include eyestrain, headaches, blurred vision, diplopia, difficulty concentrating, movement of print while reading, and lack of comprehension after reading or performing close-up activities [2-4].
The various treatments of convergence insufficiency can be mainly grouped into two categories. Passive treatment, which helps to eliminate symptoms, includes base-in prism reading glasses. Active treatments, which improve both the symptoms and clinical signs, include home-based pencil push-ups (HBPP) therapy, office-based vision therapy using orthoptic training and surgery such as bilateral medial rectus resection [1,4,5]. Recent studies have suggested that HBPP therapy is the most commonly prescribed treatment by both ophthalmologists and optometrists for symptomatic convergence insufficiency in the United States [6,7]. The current study attempts to evaluate the effectiveness of HBPP therapy for Korean patients with symptomatic convergence insufficiency.
Materials and Methods
Data was collected prospectively on 30 patients diagnosed with convergence insufficiency in January 2009. All patients included in the study had exodeviation at least 4 prism diopters (PD) greater at near than at far, a remote near point of convergence (NPC) more than 6 cm, insufficient positive fusional vergence (PFV) less than 15 PD base-out break at near and normal range near point of accommodation (NPA).
Patients with abnormal NPA, amblyopia (≥2 line difference in best-corrected visual acuity between the two eyes), anisometropia (≥2 diopters [D] spherical equivalent difference between the two eyes), history of previous head trauma, previously treated with prism glasses, history of strabismus surgery, presence of ocular abnormalities, systemic diseases or medications known to affect accommodation or vergence were excluded. Overall, 16 patients met the criteria for inclusion in the present study. The authors followed the tenets of the Declaration of Helsinki throughout the study.
Data collected from the medical records included patient age, gender, visual acuity, refractive errors, angles of deviation at distance and near, duration of symptoms, NPC, NPA and PFV prior to and after 12 weeks of HBPP therapy.
The patients were instructed on the use of HBPP therapy prior to starting treatment, and patients or their parent(s) were required to demonstrate how to correctly perform HBPP therapy before leaving the clinic. Monthly hospital visits were scheduled, and the ability to perform and compliance with HBPP therapy were checked at each visit.
In the HBPP procedure, the patient is taught to hold a pencil at arm's length positioned approximately midway between the eyes. Then, the patient is instructed to look at and attempt to maintain a single image of the pencil while it is being moved toward the nose. The patient is told to continue moving the pencil toward the nose until it is no longer possible to view the pencil as a single image. At this point, the pencil should be positioned at the most close point at which a single image is achieved. If the patient is not able to regain a single image, the entire procedure must be repeated. The patients were taught to perform two sets of 20 push-ups per day for 12 weeks.
NPC and PFV were used as indicators of outcome. Outcomes were divided into three categories as follows. A successful outcome was defined as achievement of both normal NPC (<6 cm) and normal PFV (>15 PD). An improved outcome was defined as having at least one of the following; a normal NPC, an improvement of greater than 4 cm in NPC, a normal PFV or an increase of greater than 10 PD in PFV. Patients who did not meet the criteria for successful or improved outcome were considered to be non-responders.
Results
Table 1 shows descriptive data for the 16 patients in the present study. The mean age of the patients was 19 years (range, 7 to 34 years). The mean refractive error (spherical equivalent) was -1.6 ± 1.8 D in the right eyes and -1.4 ± 1.9 D in the left eyes. There was no difference in mean refractive error between the two eyes (p > 0.05). The average duration of symptomatic convergence insufficiency was 11.6 ± 2.3 months.
Fig. 1 illustrates the change in mean deviation angle of exodeviation prior to and after 12 weeks of HBPP therapy. The mean deviation angle at distance decreased from 3 PD to orthophoria, and the mean deviation angle at near decreased from 12 PD to 4 PD after HBPP therapy. The amount of decrease in exodeviation was greater at near than at distance. Fig. 2 illustrates the change in mean NPC prior to and after 12 weeks of HBPP therapy. The mean value of NPC decreased from 36.6 cm to 14.4 cm, and the mean value of PFV increased from 11.3 PD to 19.1 PD after 12 weeks of HBPP therapy.
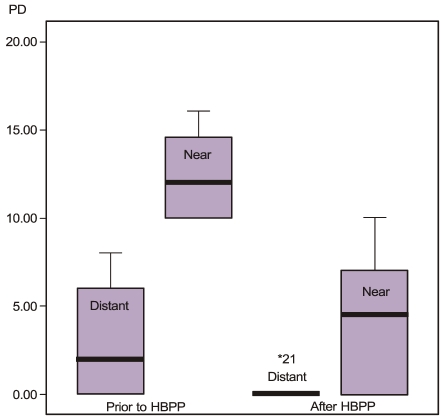
After 12 weeks of home-based pencil push-ups (HBPP) therapy, the mean angle of exodeviation decreased from 3 prism diopters (PD) to orthophoria at distance and from 12 PD to 4 PD at near.

The mean value of near point of convergence (NPC) decreased from 36.6 cm to 14.4 cm after 12 weeks of home-based pencil push-ups (HBPP) therapy.
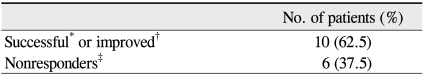
Table 2 demonstrates outcome measures of the patients enrolled in the present study. After 12 weeks of HBPP therapy, ten patients (62.5%) were categorized as either successful or improved, and six patients (37.5%) were categorized as non-responders. No adverse event that included eyes or vision was reported during the 12 weeks of HBPP therapy.
Discussion
HBPP therapy is a simple, cost-free and easily taught procedure that involves fewer follow-up visits than does office-based therapy (four visits during 12 weeks versus 12 visits in 12 weeks) [4-9]. Therefore, HBPP therapy is the most commonly prescribed treatment for symptomatic convergence insufficiency in the United States [6,7]. In addition, HBPP therapy is an especially useful treatment for Korean patients with convergence insufficiency because there is no official system of licensure for orthoptists in Korea. However, no published report previously existed on the result of HBPP therapy for patients with symptomatic convergence insufficiency in Korea.
Prior to starting the present study, the authors expected to observe somewhat different results from those of other studies due to the differences in ethnicity and notoriously higher near-work demands for Korean students.
The effectiveness of the 12-week HBPP therapy in Korean patients with symptomatic convergence insufficiency was evaluated. The results from the present study indicated that 62.5% of the patients showed either successful or improved outcomes after 12 weeks of HBPP therapy. The effectiveness rate observed in the present study was relatively higher than the results of the Convergence Insufficiency Treatment Trial study group, which reported that only 20% to 43% of the patients showed successful or improved outcomes after 12 weeks of HBPP therapy [4,8,10]. According to these previous reports, HBPP or other home-based therapy was no more effective in decreasing signs or symptoms than was placebo therapy. Placebo response rates for a variety of medical conditions have been reported to range from 15% to 58%, with an average placebo effectiveness of 35% [11]. Thus, the effectiveness of HBPP therapy in the present study appears to be irrelevant to the placebo effect.
The baseline characteristics of the current study are comparable to those of previous studies. The mean deviation angle of near exophoria (12 PD vs. 9 to 11 PD), and PFV values at near (11.3 PD vs. 11.8 to 13 PD) were similar between the patients enrolled in the present study and those in other studies [4,8-10]. However, differences were found in the mean NPC and patient age. The mean NPC in the present study was 36.6 cm, which was a significantly worse value than 13.5 cm to 14 cm observed in other studies [4,8-10]. The mean age was 19 years in the present study and the range (7 to 34 years) was wider than the 12 to 24 years seen in other studies [4,8-10]. Additionally, the patients were all from a single ethnic group. The above-mentioned subject characteristics may be the cause of the different success rates between the current study and other studies.
There were several different characteristics between the successful or improved group and the non-responders group in the present study. The improved patients were relatively young (less than 17 years) and had smaller exophoria (≤12 PD) at near fixation. However, four of the non-responder patients were older than 18 years and all six had larger exophoria (>12 PD). These results correspond with those of a previous study which reported that convergence insufficiency is able to be more effectively treated in children than in adults [9]. Therefore, the patient's age and extent of exophoria at near fixation may be prognostic factors of HBPP therapy for convergence insufficiency.
A positive aspect of the present study is that stricter inclusion criteria were used compared to those in other studies. The patients with abnormal NPA were excluded in order to rule out convergence insufficiency associated with accommodative insufficiency. This may be a possible explanation for the relatively higher success rate observed in the present study as these patients do not respond well to any type of orthoptic training [1]. The possibility of inclusion of such patients in other studies cannot be excluded because the NPA values of the patients were not mentioned.
However, the present study has important limitations mostly due to a small sample size and lack of symptom level measurement using the questionnaire. In addition, the patients were not divided into children and young adult groups as they were in other studies. The current study was not designed to demonstrate maximal improvement with HBPP therapy, and a treatment duration longer than 12 weeks may have resulted in additional changes in signs and symptoms. Furthermore, a much larger prospective study will be necessary to acquire the clinical profiles of Korean patients with symptomatic convergence insufficiency.
The current study is the first report to evaluate the effectiveness of a 12-week HBPP therapy in Korean patients with symptomatic convergence insufficiency. In summary, the study demonstrates that HBPP therapy is an easy, cost-free and effective therapy for patients with symptomatic convergence insufficiency.
Notes
No potential conflict of interest relevant to this article was reported.
This paper was presented in part at the 102nd annual meeting of the Korean Ophthalmological Society, November, 2009 in Goyang, Korea.