Comparison of Fibrin Glue and Sutures for Conjunctival Wound Closure in Strabismus Surgery
Article information
Abstract
Purpose
To evaluate and compare the efficacy and tolerance of fibrin glue and sutures for closing conjunctival wounds in strabismus surgery.
Methods
In a prospective trial, we performed strabismus surgery using limbal incisions. Conjunctival wounds were closed with fibrin glue in 20 eyes of 20 patients (fibrin group) and 8-0 polyglactin suture in 20 eyes of 20 patients (suture group). Postoperative pain, tearing, and inflammation were compared at 1 day, 1 week, 3 weeks, and 6 weeks after surgery. Conjunctival incision healing was also investigated.
Results
One day and one week post-operatively, pain and tearing scores were lower in the fibrin group (p = 0.000, respectively). Mean surgery time was significantly shorter in the fibrin (48 ± 5 minutes) than the suture group (63 ± 7 minutes) (p = 0.000). Inflammation was significantly more severe in the suture group until 3 weeks postoperative (p = 0.000, respectively), but conjunctival healing did not differ between the groups. Hyperemia appeared more prominent in the fibrin group 3 and 6 weeks after surgery (p = 0.087 and 0.000, respectively). Two eyes in the fibrin group showed conjunctival gaps of more than 2 mm, which closed spontaneously by three weeks after surgery. No allergic reactions or infections developed.
Conclusions
Fibrin glue proved to be as effective as sutures in closing conjunctival wounds. It provides more comfortable early postoperative courses and might be considered as an alternative to sutures in strabismus surgery.
Polyglactin 8-0 suture is commonly used to close the conjunctiva in conventional strabismus and other ocular surgeries but can cause significant irritation and discomfort in the early postoperative period. Also, other suture-related complications might occur, such as prolonged inflammatory reaction at the suture site, suture granuloma or abscess, and giant papillary conjunctivitis [1]. To avoid these drawbacks, sutureless wound closure with fibrin-based tissue adhesives has gained increased acceptance in ocular surgeries including corneal perforation [2], leaking filtration blebs [3], conjunctival autograft for pterygium [4-6], cataract wound closure [7], pars plana vitrectomy [8,9], and conjunctivochalasis [10,11].
Fibrin sealant is biological glue made of fibrinogen and thrombin. The adhesive properties of fibrin glue have proven useful in preventing excessive bleeding and enhancing tissue adhesion in selective general and cardiovascular surgeries [12,13]. In strabismus surgery, fibrin glue has been tried to close conjunctival wounds [14-16] and attach extraocular muscle [17,18]. Many previous studies concluded that fibrin glue caused less postoperative discomfort and shortened surgical time, but few reports objectively compare fibrin glue and sutures along a time course of conjunctival wound healing.
In this prospective study, we evaluated the clinical efficacy and tolerance of fibrin glue for conjunctival wound healing in usual strabismus surgery and compared it with conventional suturing by analyzing objective parameters.
Materials and Methods
This prospective clinical study involved 40 patients who underwent primary strabismus surgery at Bucheon St. Mary's Hospital from July 1, 2007 to December 31, 2007. Subjects were chosen from patients diagnosed with esotropia or exotropia who were planning to undergo primary horizontal extraocular muscle surgery. Exclusion criteria included a history and/or signs of ocular inflammation or hypersensitivity to ocular drugs. Thirty-four patients had exotropia and 6 had esotropia. Written informed consent was obtained from the patients or parents. A random number was assigned to each patient before the operation and odd numbers were assigned to the fibrin group and even numbers to the suture group. Each group contained 20 eyes in 20 patients. Radial limbal conjunctival incisions were used in all patients.
Preparation of fibrin tissue glue
Fibrin glue is a tissue adhesive composed of two components that mimic natural fibrin formation. One component contains fibrinogen mixed with coagulation factor 13 and aprotinin, and the other contains thrombin and calcium chloride. When the two components are mixed, thrombin converts fibrinogen into fibrin which is then cross-linked by coagulation factor 13 to create a firm fibrin clot. The fibrin clot is stabilized by Aprotinin which also prevents rapid fibrinolysis. In this study, commercially available Greenplast® fibrin glue (Green Cross, Seoul, Korea) was prepared according to the manufacturer's instructions. Both components are placed in a dual injection system for simultaneous injection. A fibrin clot forms within 30 seconds of injection. A human thrombin solution (500 IU/mL) was used to ensure faster fibrin formation.
Surgical technique
Horizontal strabismus surgery under general anesthesia was performed by a single surgeon (NYK). After making an 8 mm peritomy with two radial limbal conjunctival incisions, performed bilateral symmetrical extraocular muscle recession or resection, unilateral recession-resection procedure or unilateral large recession was performed. After completing the muscle surgery with the lid speculum in place, the conjunctival wound was closed without tension. Excessive Tenon's capsule was excised in all cases.
In the suture group, conjunctiva was closed with 4 to 6 stitches of interrupted 8-0 polyglactin suture (Vicryl®; Johnson & Johnson, Livingston, UK). Loose ends of the knot were cut shortly. When closing with glue (fibrin group), the location on the sclera where glue was intended to be applied was dried using a Weck-Cel sponge. One or two drops of both components were instilled simultaneously on the bare sclera near the limbus and just below the free edges of conjunctiva, which were held with forceps. Immediately after applying the glue, the conjunctival edges were pressed together with two forceps for two or three minutes to create firm adhesion along the entire length (Fig. 1). Excess glue was trimmed with scissors and a pressure patch was applied for 24 hours. Postoperatively, antibiotic and corticosteroid eye drops were applied four times daily for four weeks, then twice daily for two more weeks. Total surgical time was recorded for each patient and the conjunctival closure time of each wound was recorded later in ten patients from each group.
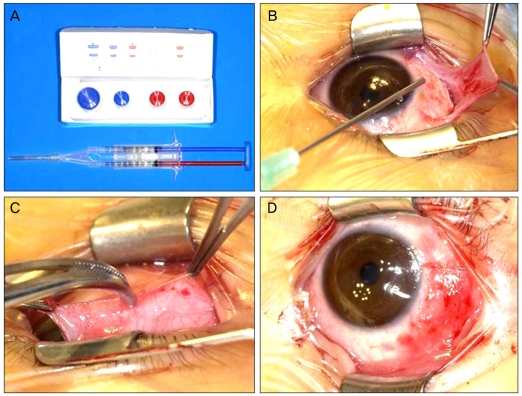
(A) Commercial fibrin glue (Greenplast®). (B) Application of Greenplast® on scleral corners along the free edges of the conjunctival flap. (C) Using two forceps, opposing edges of the conjunctiva are pressed and attached to each other. (D) Conjunctival wound closed using fibrin.
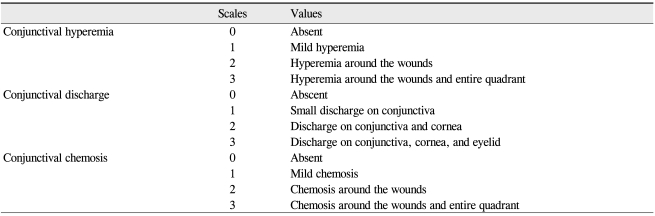
Postoperative pain, tearing, and the extent of inflammation were analyzed and compared at one day, one week, three weeks, and six weeks after surgery in both groups. For pain and tearing, patient's subjective discomfort was graded on a scale from 0-to-3 (0, total comfort; 1, minor discomfort; 2, moderate discomfort; 3, severe discomfort) [19,20]. We modified the facial pain scale-revised [21] to our 0 to 3 scale for patient and parents ease. When a subjective determination of comfort was difficult to obtain in young children, the parents were asked to provide an estimate. Using slit-lamp biomicroscope, we graded the conjunctival inflammation in the operated quadrant using a modified conjunctival inflammatory index [22,23] (Table 1) in which hyperemia, chemosis, and discharge were rated on a 0 to 3 scale (0, none; 1, mild; 2, moderate; 3, severe) for a maximum possible inflammation score of 9. Conjunctival incision healing was also investigated by measuring the largest gap size perpendicular to the incision line (in millimeters) using a slit-lamp beam [19,20]. These observations were conducted for all eyes, although only the right eyes were used in cases of bilateral surgery. Statistical analysis was performed with Mann Whitney U-test (SPSS; SPSS Inc., Chicago, IL, USA). A p-value of less than 0.05 was considered statistically significant.
Results
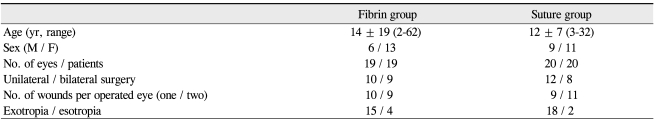
One eye of one male patient in the fibrin group was excluded due to conjunctival wound dehiscence caused by inadvertent removal of the patch one hour after surgery. Study subjects included 15 males and 24 females, ranging from two to 62 years of age (mean, 13.1 years). Ten patients in the fibrin group and 12 in the suture group received unilateral surgery. One patient in each group underwent large one muscle recession. Clinical characteristics of the patients are summarized in Table 2.
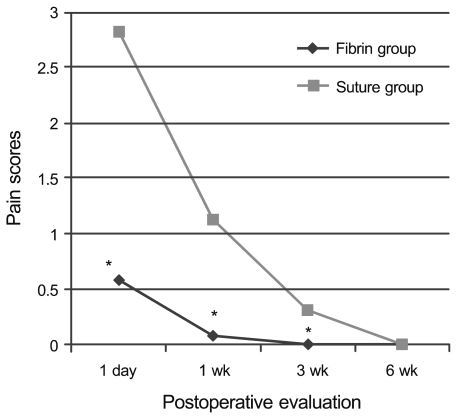
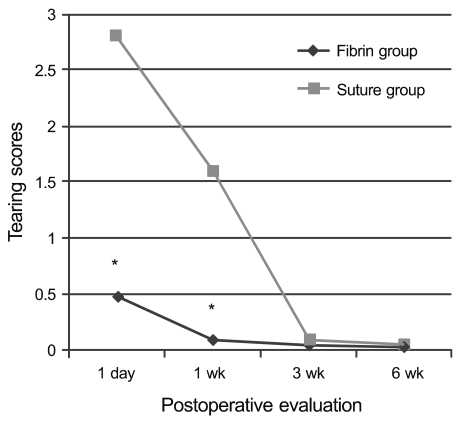
One day and one week postoperative, the pain and tearing scores were significantly lower in the fibrin group than in the suture group (p = 0.000, respectively) (Figs. 2 and 3). The mean duration of discomfort was 1.0 ± 0.2 days in the fibrin group and 3.1 ± 1.1 days in the suture group (p = 0.000). Patients in the fibrin group were easily able to open their eyes one day after surgery; this achievement was not possible until 2.7 days after surgery in the suture group. Postoperative pain was significantly decreased in the fibrin group and was sustained for three weeks after surgery. Postoperative tearing was also significantly less in the fibrin group during the two weeks after surgery.
Mean total surgery time was significantly shorter in the fibrin group (48 ± 5 minutes) than in the suture group (63 ± 7 minutes) (p = 0.000). The mean conjunctival closure time of ten patients in the fibrin group was 3.85 ± 0.9 minutes (range, 2 to 7), significantly shorter than that of the ten patients in the suture group (8.35 ± 0.6 minutes; range, 7 to 10) (p = 0.000).
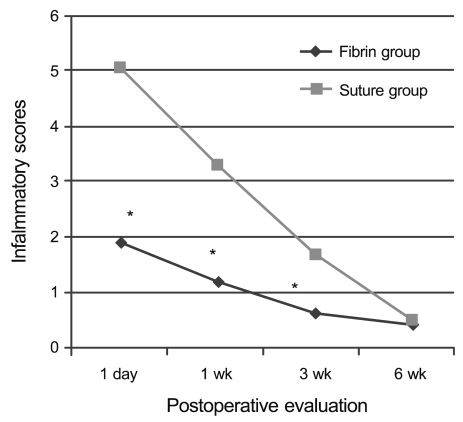
The inflammation was significantly more severe in the suture group for the first three postoperative weeks (p = 0.000, respectively) (Fig. 4), but the healing of conjunctival gap did not differ between the groups (Fig. 5). Three weeks after surgery, conjunctival incisions had successfully attached in all patients (Fig. 6) and remained intact throughout the follow-up period.
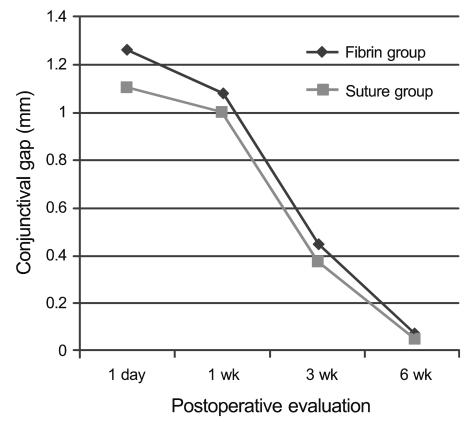
Mean postoperative conjunctival gap sizes at four follow-up time points. No significant differences were noted between the groups (p = 0.019, 0.240, 0.240, and 1.00 at each time point).
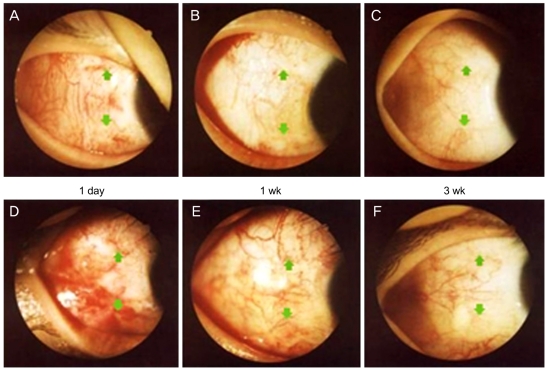
Photographs of conjunctival healing in the fibrin (A-C) and suture groups (D-F) at postoperative time points. Arrows indicate conjunctival incision lines.
No patients showed wound dehiscence. No cases in the fibrin group required additional sutures to close the conjunctival wound. Two eyes (10.5%) in the fibrin group developed conjunctival defects greater than 2 mm, but secondary re-epithelization and spontaneous healing occurred within three weeks without additional sutures. All patients in the fibrin group had some prominent conjunctival vascular engorgement at three and six weeks (p = 0.087, and 0.000, respectively), but it resolved gradually and spontaneously. There was no prolapse of Tenon's capsule through the conjunctival incisions. No allergic reactions or infections occurred in the postoperative period. The perilimbal conjunctival incision retracted in 26.3% (5 / 19) of the fibrin group and in 15% (3 / 20) of the suture group at six weeks.
Discussion
Proper management of the conjunctiva is essential for successful strabismus surgery. Polyglactin 8-0 sutures are commonly used but it can cause irritation and discomfort during the early postoperative period and may delay normal life activities; young children may not even be able to open their eyes. When handling thin, atrophic, weakened, senile, or scarred conjunctiva, suturing may be time-consuming and may involve a risk of tearing.
Tissue adhesives effectively attach opposing wound edges and may avoid suture-related problems. Fibrin glue is a biological tissue adhesive composed of fibrinogen and other components. The glue mimics the physiologic coagulation process, so it is biodegradable and aids wound healing without inducing toxic or foreign body reactions [13,24]. The fibrin clot is reabsorbed during wound healing within days to weeks depending on the surgery, the amount of glue used, and the proteolytic activity of the treated site [16]. Fibrin glue has many advantages that make it ideal for use in ophthalmic surgery. First, it is biocompatible, non-toxic, and may be used beneath a superficial covering such as structural filler, as an alternative to sutures, or as a barrier that facilitates epithelial wound healing [13,24]. Second, fibrin glue creates a two-dimensional seal, while sutures only provide a focal seal [25]. Third, the coagulation time of fibrin glue can be controlled during surgery by controlling the thrombin concentration, and its rapid coagulation could shorten the operation time. Recently fibrin glue has been studied for many ophthalmic uses [2-11], including scleral closure in cataract surgery and pars plana vitrectomy [26,27].
After Zauberman and Hemo [14] used non-commercial fibrin glue for conjunctival closure in ten recession and resection procedures, Biedner and Rosenthal [15] compared fibrin glue and 9-0 polyglactin suture for conjunctival closure in strabismus surgery and confirmed suturing caused more discomfort and inflammation during the early postoperative period. However this study was conducted in only six patients and followed-up 2 weeks after surgery. Similarly, Dadeya and Ms [28] applied fibrin glue to one eye and 6-0 vicryl sutures to the other in 19 patients who underwent bilateral symmetrical horizontal muscle recession. These patients reported increased discomfort and inflammation during the early postoperative period due to sutures (ocular discomfort in 8 of 19 (42.1%) sutured eyes but in no fibrin glued eyes). Mohan et al. [16] also concluded that fibrin glue is a better alternative to polyglactin sutures for conjunctival closure following strabismus surgery. All of these studies were conducted during the early postoperative period with few patients.
In our study, we compared 8-0 polyglactin sutures with commercial fibrin glue using limbal conjunctival incisions over a longer follow-up time, until conjunctival healing was complete. As in usual clinical situations, recession or resection procedures were performed and in order to produce more objective results, we selected one eye from each patient rather than comparing outcomes on both eyes in the same subject. Similar to previous reports, fibrin glue prevented early postoperative discomfort and suture-related complications in our study. Postoperative pain and tearing were significantly reduced, and patients in the fibrin group were able to return to normal activities the day after surgery without severe discomfort. Inflammation was also significantly decreased in the fibrin group during the early postoperative period.
We investigated conjunctival incision healing during a six-week time course. The healing process of the conjunctiva takes a similar time course to that in suture closure. Conjunctive reattachment with fibrin glue was shown to be reliable. It is well known that fibrin glue has a lower tensile strength and slower polymerization compared to those of synthetic adhesives [13,18]. Fibrin glue does not permit strong adhesion immediately after surgery because of its low tensile strength but can withstand the force induced by conjunctival wounds during follow-up in our study. Spierer et al. [17] performed reattachments of rabbit extraocular muscles using fibrin and reported that the tensile strength of the fibrin did not overcome the muscle's contracture in smaller recessions, thus causing posterior displacements of the inserted muscle.
The main finding of our study was that the adhesiveness of fibrin glue for conjunctival wound was successful in a manner comparable to 8-0 polyglactin sutures. The conjunctiva was well apposed without any dehiscence by one day postoperatively and thereafter in all patients in the fibrin group. Krzizok [29] used Beriplast (Beriplast® P; Aventis Behring, Marburg, Germany) for conjunctival closure in 100 eye muscle surgeries, ten scleral buckling procedures, and 20 pars plana vitrectomies and reported effective sutureless surgery. He concluded that fibrin glue was time saving and effective, especially in thin atrophic conjunctiva in adults, but warned of limited use of fibrin sealant in children because of extensive Tenon's fascia. We did not experience extrusion of Tenon or conjunctival dehiscence in our study and speculate that the removal of sufficient anterior Tenon and the use of a pressure patch may contribute to successful conjunctival reattachment.
When using fibrin glue in fornix incision, Erbagci and Bekir [30] did not observe any difference between thin adult conjunctiva and thick pulpy conjunctival wounds in children. Consistent with other reports [14-16,28-30], the use of fibrin glue in our study diminished conjuctival closure time by approximately 4.5 to 5 minutes, and the duration of surgery was shortened by 72% compared to that of the suture group. Using commercial fibrin glue and a dual injector system provides more simple and quick handling of conjunctiva in strabismus surgery.
Until recently, preparation time, curing time, and cost have precluded the practical use of fibrin glue. Now the development of commercial fibrin glue with a dual injector system, reliable serologic tests, and well-established methods for sterilization make it a much more practical application. However, use of fibrin glue may theoretically transmit disease and/ or cause an anaphylactic reaction, although we are unaware of any such cases. In this study, none of the patients showed allergic reaction or viral infection during the follow-up period.
Although fibrin glue showed successful adhesiveness and tolerance in wound closure, many patients in the fibrin group expressed foreign body sensation and light conjunctival hyperemia during the early healing period. The only adverse postoperative occurrence in this study was some perilimbal conjunctival retraction, which occurred more frequently in the fibrin group but was not significant. We speculate that this reaction was due to the low tensile strength of fibrin glue, which cannot endure the traction power of tissue edema or fibrosis during wound healing. Even in the conventional limbal approach using sutures, the edges of the conjunctival flap sometimes retracted from the limbus before it formed sufficient adhesions to the underlying sclera, even after proper closure. This retraction was usually well tolerated in most cases, and the thickened conjunctival became smooth and sufficiently flattened as the wound healed. We believe that gluing is more difficult in medial conjunctival wounds, especially when resecting the medial rectus muscle, because of the extensive Tenon and muscle bump.
The small sample size is an obvious limitation of this study. A large, randomized, and long-term follow-up study is needed. Histopathologic studies concerning the effects of fibrin glue on episclera and conjunctiva in humans as well as the effects of re-operation after gluing will be needed.
In conclusion, our results indicate that the use of fibrin glue decreases early postoperative pain and tearing, postoperative inflammation and surgical time, and provides a more comfortable course for conjunctival closure after strabismus surgery. Therefore, this procedure should be considered as an alternative to sutures. Before application in children with extensive Tenon's capsule, sufficient excision of the anterior Tenon is recommended.
Notes
No potential conflict of interest relevant to this article was reported.
Presented in part as a poster at the 32nd Meeting of the European Strabismological Association in Munich, Germany, September 7-10, 2008.