 |
 |
| Korean J Ophthalmol > Volume 24(2); 2010 > Article |
Abstract
Purpose
Impending central retinal vein occlusion is associated with mild or no loss of vision; however, its progress and vision prognosis have not been clearly defined until now. Therefore, we studied the progress and prognoses in patients with impending central retinal vein occlusion.
Methods
For this study, we selected ten subjects who had been diagnosed with impending central retinal vein occlusion, and we retrospectively reviewed their progress and prognoses.
Results
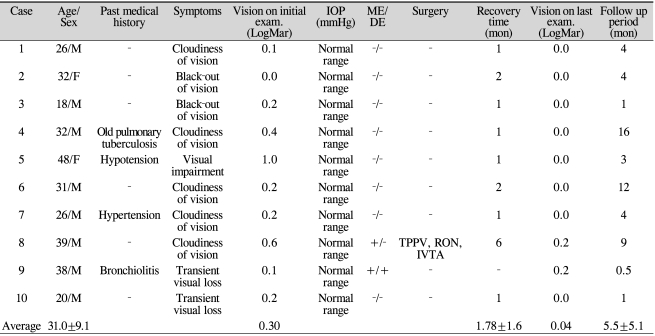
The average age of the subjects was 31.0 years (18 to 48 years). Eight patients were male and two were female. The average observational period was 5.5 months. Six out of ten subjects were found to have no underlying systemic disease, four subjects had underlying disease. All ten patients were affected unilaterally. When initially tested, the affected eyes showed an average vision of LogMar 0.30. The final vision test revealed an average of LogMar 0.04, which indicates good progress and prognosis. In one patient, retinal hemorrhage and macular edema progressively worsened after the diagnosis, and the patient was treated with radial optic neurotomy.
Conclusions
The cases of impending central retinal vein occlusion that we observed seemed to primarily affect young patients with generally good prognoses. However, in some cases, the degrees of obstruction and hemorrhage increased as time progressed. This suggests that impending central retinal vein occlusion could develop into the prodromal phase of an acute attack.
Central retinal vein occlusion mainly affects people over 60 years of age, and it can cause loss of vision due to retinal hemorrhage [1-2]. Many classifications of central retinal vein occlusion have been published, but the most noticeable report was published by Magargal et al. [3] in 1982. They classified central retinal vein occlusion into ischemic, non-ischemic, and intermediate. Later, Gass created a new classification of impending central retinal vein occlusion, which has little or no loss of vision [4]. However, the progress and prognosis of vision for impending central retinal vein occlusion has not been reported. Therefore, we performed this study on the natural progress and visual prognosis of impending central retinal vein occlusion.
We selected patients who were diagnosed with impending central retinal vein occlusion from January 2003 to March 2007 in Wonju Christian Hospital, and we retrospectively studied their medical records. By Gass' definition, impending central retinal vein occlusion has mild or no loss of vision with venodilation and retinal dot hemorrhages under fundus examination [4]. In all patients, slitlamp examination, intraocular pressure, gonioscopy, refraction, visual field, funduscopy, and fluorescein angiography were performed as part of a physical examination. To determine any underlying systemic disease, blood test, neurologic examination including brain computed tomography scan, carotid artery ultrasonography, cardiovascular examination including blood pressure measurement, and electrocardiography were performed.
In ten patients with impending central retinal vein occlusion, eight were male (80%) and two were female (20%). The age distribution was between 18 and 48 years, with impending central retinal vein occlusion usually affecting a relatively young age group averaging 31.0┬▒9.1 years of age. All ten subjects were affected unilaterally. The ocular pressures in all subjects were found to be normal. On fundus examination, mild venous dilation and retinal hemorrhage were observed. The initial vision for the affected eyes was LogMar 0.30, and the final vision was LogMar 0.04. Eight out of ten patients showed good visual progress (Table 1).
The average recovery time was 1.8 months. Two subjects showed worsening of symptoms during the study period. One case had progressed to central retinal vein occlusion, and after treatment with vitrectomy, radial optic neurotomy and intravitreal injection of triamcinolone, the patient's vision improved. The other patient was not treated due to the short follow-up period. Four patients had hypotension, hypertension, pulmonary tuberculosis, and bronchiolitis, respectively. The other six patients had no specific systemic disease and no abnormalities on neurologic examination.
An 18-year-old male patient with no specific history was admitted due to complaints of amaurosis fugax in his left eye. Blood test and neurologic exam did not reveal any abnormality. The initial LogMar vision was 0.2. On fundus examination, venous tortuosity and dilation in the central retinal vein were found. He was followed for one month without any particular treatment. The LogMar vision after one month was improved to 0.0, and venous tortuosity and congestion in the central retinal vein disappeared completely (Fig 1).
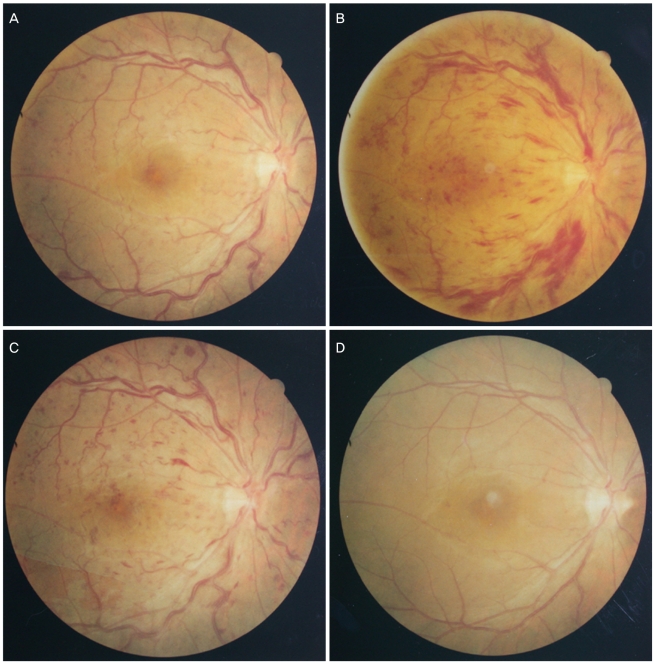
A 31-year-old male patient with complaints of mild vision loss in his left eye visited the hospital. No specific history was discovered. Blood test and neurologic examination showed no specific finding. The initial vision was LogMar 0.2, and on fundus examination, venous tortuosity, venous dilation, dot hemorrhages, and cotton-wool spots were observed. The patient was followed for two months without treatment, after which his vision improved to 0.0 and the previously observed central vein and retinal lesions improved (Fig 2).
A 39-year-old male patient without any specific history visited the hospital with the chief complaint of vision loss in his right eye. The initial vision was LogMar 0.6. Under fundus examination, venous tortuisity, dilation, and retinal h emorrhages were observed. After two weeks of admission, the retinal hemorrhage was aggravated, and the vision was down to LogMar 1.0. The patient was treated with vitrectomy, radial optic neurotomy and intravitreal injection of triamcinolone. After two weeks of treatment, the retinal hemorrhage improved. After six months, the retinal hemorrhage subsided (Fig 3). The retinal venous tortuisity and dilation in the central retinal vein improved, and the LogMar vision also improved to 0.2.
A 38-year-old male patient with a history of bronchiolitis visited the hospital due to vision loss in the right eye. The initial LogMar vision was 0.1. On fundus examination, papilledema was discovered together with retinal venous tortuisity, dilation, and retinal dot hemorrhages in central retinal vein occlusion. The patient was followed without specific treatment. Two weeks after the visit, the vision was aggravated to 0.2, with macular edema and papilledema (Fig 4).
Central retinal vein occlusion has a wide range of manifestations, from mild and sporadic retinal hemorrhage to vitreous hemorrhage. Since Leber [5] first described the clinical manifestation of central retinal vein occlusion as retinal apoplexy in 1854, scholars have suggested multiple classifications of the disease. Hayreh et al. [6] classified central retinal vein obstruction into two categories, venous stasis retinopathy and hemorrhagic retinopathy. Venous stasis retinopathy is a mild form without central retinal vein occlusion, and hemorrhagic retinopathy is a severe form with central retinal vein occlusion. The two different types have a different fundus finding, clinical manifestation and prognosis [6]. Magargal et al. [3] added an intermediate category into the original classification of Hayreh et al. and at the same time classified it into three types based on ischemic and hyperpermeable conditions. Gass et al. [4] reported impending or incipient central retinal vein occlusion. By Gass' definition, impending central retinal vein occlusion has no or mild loss of vision with venodilation and retinal dot hemorrhage under fundus examination [4]. This condition has also been defined as a lesion with transient vision loss [4]. Gass et al. [4] considered impending central retinal vein occlusion as a risk factor for the development of central retinal vein occlusion. However, no confirmed theory has been published regarding the natural progress of impending central retinal vein occlusion.
Mancall [7] suggested that in the case of central retinal vein occlusion, the left eye is more frequently involved in males. However, Raitta [8] reported no discrepancies between left and right involvement or in male and female prevalence. In this study, we found that impending central retinal vein occlusion is more prevalent in males. No difference in prevalence was found between the left and right eyes.
Factors known to cause central retinal vein occlusion include hypertension, diabetes mellitus, atherosclerosis, hyperlipidemia and primary open angle glaucoma [1]. Zegarra et al. [9] reported that hypertension, atherosclerosis and diabetes mellitus accompany central retinal vein occlusion in 57%, 34%, and 34% of cases, respectively. Other studies have discovered that hematologic disease, paraproteinemia, vasculitis, and autoimmune disease accompanying changes in coagulation mechanism and viscosity of blood are often associated with central retinal vein occlusion [10-13]. In our study, four patients had systemic disease including hypertension, hypotenstion, bronchiolitis and pulmonary tuberculosis. Hypertension, diabetes mellitus, hyperlipidemia, and other factors are relatively less associated with the occurrence of central retinal vein occlusion than they are with increased age [14]. Most of our patients were rather young, so they did not have general systemic risk factors of central retinal vein occlusion, except for hypertension.
Central retinal vein occlusion in young individuals usually has a good prognosis and a decreased risk for serious vision loss. In this study, we found that most patients recovered without any specific treatment, with only two patients developing aggravated disease. In the case of one patient, treatment with vitrectomy, radial optic neurotomy, and intravitreal injection of triamcinolone improved the condition.
We conclude that most cases of impending central retinal vein occlusion have a good prognosis. On the other hand, we found that the disease can advance to the prodromal phase of central retinal vein occlusion with intensifying obstruction and hemorrhages. Therefore, it appears that this disease may have the potential for bidirectional progress.
REFERENCES
1. The Eye Disease Case-Control Study Group. Risk factors for central retinal vein occlusion. Arch Ophthalmol 1996;114:545-554.


2. Gutman FA. Evaluation of a patient with central retinal vein occlusion. Ophthalmology 1983;90:481-483.


3. Magargal LE, Donoso LA, Sanborn GE. Retinal ischemia and risk of neovascularization following central retinal vein obstruction. Ophthalmology 1982;89:1241-1245.


4. Gass JD. Stereoscopic atlas of macular disease: diagnosis and treatment. 1997. 4th ed. St Louis: Mosby; p. 546-555.
5. Leber T. Graefe-Seamisch handbuch der gestamtem augenheikunde. 1877. Leibzig: Englelmann; p. 551.
6. Hayreh SS. So-called 'central retinal vein occlusion'. II. Venous stasis retinopathy. Ophthalmologica 1976;172:14-37.


8. Raitta C. Central venous and retinal venous occlusion. Acta Ophthalmol Suppl 1965;83:1-123.
9. Zegarra H, Gutman FA, Conforto J. The natural course of central retinal vein occlusion. Ophthalmology 1979;86:1931-1942.


10. Lahey JM, Tunc M, Kearney J, et al. Laboatory evaluation of hypercoagulable state in patients with central retinal vein occlusion who are less than 56 years of age. Ophthalmology 2002;109:126-131.


11. Williamson TH, Rumley A, Lowe GD. Blood viscosity, coagulation, and activated protein C resistance in central retinal vein occlusion: a population controlled study. Br J Ophthalmol 1996;80:203-208.



12. Cobo-Soriano R, Sanchez-Ramon S, Aparicio MJ, et al. Antiphospholipid antibodies and retinal thrombosis in patients without risk factors: a prospective case-control study. Am J Ophthalmol 1999;128:725-732.


Fig.┬Ā1
Case 3. (A) Fundus findings of slightly tortuous and engorged retinal veins at first visit. (B) After one month, the retinal venous tortuosity and engorgement were no longer present.
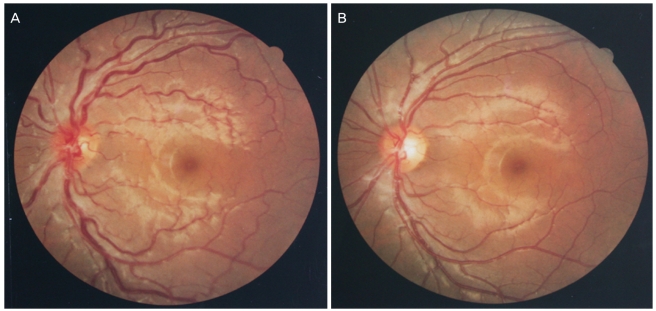
Fig.┬Ā2
Case 6. (A) Fundus findings of flame-shaped retinal hemorrhage, moderated retinal venous engorgement, cotton-wool spots and dot hemorrhage at first visit. (B) After two months, the fundus returned to its normal appearance.

Fig.┬Ā3
Case 8. (A) Fundus findings of some dot retinal hemorrhages and moderated retinal venous engorgement at first visit. (B) After two weeks, the flame-shaped retinal hemorrhages and vascular tortuosity increased. Vitrectomy, radical optic neurotomy and intravitreal triamcinolone injection were performed. (C) Two weeks after radial optic neurotomy, retinal hemorrhage and tortuosity decreased. (D) After six months, the fundus returned to its normal appearance.




 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print




