 |
 |
| Korean J Ophthalmol > Volume 24(1); 2010 > Article |
Abstract
Purpose
To describe a series of patients with lower eyelid epiblepharon associated with lower eyelid retraction.
Methods
We retrospectively reviewed the medical records of patients who underwent surgery for lower eyelid retraction, epiblepharon, or thyroid-associated ophthalmopathy (TAO) between October 1999 and March 2007. Patients with both lower eyelid retraction and epiblepharon on preoperative examination were included in this study.
Results
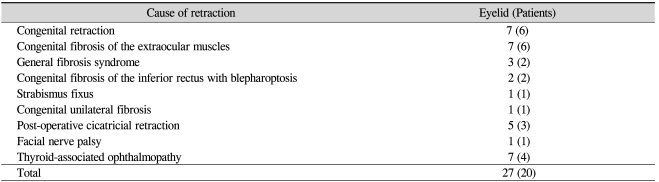
Twenty-seven eyelids of 20 patients with both lower eyelid retraction and epiblepharon were enrolled. The underlying causes of lower eyelid retraction included congenital retraction (seven eyelids), congenital fibrosis of the extraocular muscles (CFEOM; seven eyelids), TAO (seven eyelids), post-operative cicatricial retraction (five eyelids), and facial nerve palsy (one eyelid). Eight of 27 eyelids were successfully corrected after the repair of retraction without the repair of epiblepharon, regardless of the cause of lower eyelid retraction. Another four eyelids with epiblepharon associated with TAO resolved after only orbital decompression. Cilia-everting sutures were additionally applied for epiblepharon in another 14 eyelids, 12 of which did not require the excision of a skin fold or the orbicularis muscles. Only one eyelid with mild retraction and epiblepharon underwent simple epiblepharon repair. Recurrence of retraction or epiblepharon developed in three eyelids during follow-up.
Lower eyelid retraction describes an abnormality in which the resting position of the lower eyelid is too low. The normal position of the lower eyelid is at the level of the inferior limbus. Although there are many normal variations, lower eyelid retraction is clinically diagnosed when any sclera is visible between the inferior corneoscleral limbus and the eyelid margin or when the lower eyelid margins of the two eyes are at different levels [1].
Lagophthalmos, exposure keratopathy, conjunctivitis, and unnatural appearance are well known complaints and indications for surgical intervention in patients with lower eyelid retraction [2]. Inward rotation of the lower eyelashes, namely lower eyelid epiblepharon, can be found in the presence of lower eyelid retraction and can cause functional problems. However, this consideration has not been adequately addressed in the literature. To the best of the author's knowledge, only a few cases of acquired lower eyelid epiblepharon have been described in patients with thyroid eyelid retraction [3].
In this study, we report the clinical features, management, and outcomes in patients with lower eyelid epiblepharon associated with lower eyelid retraction.
We reviewed the medical records of all patients who underwent surgery for lower eyelid retraction or lower eyelid epiblepharon under the care of one surgeon (SIK) at Seoul National University Hospital between October 1999 and March 2007. We also reviewed the records of patients who were surgically treated for thyroid-associated ophthalmopathy (TAO) during the same period, regardless of the surgical procedure performed. We reviewed all TAO patients who underwent surgery because there is a possibility that eyelid retraction or epiblepharon in these patients can be resolved after orbital wall decompression without the need for lid surgery.
Patients with both lower eyelid retraction and epiblepharon on the preoperative examination were included as subjects of special interest to the authors. Patients with entropion, in which the eyelid margins were in-turning, were excluded. Patients with anophthalmic retraction were also excluded, because their cornea-touching cilia were thought to be attributable to entropion related to horizontal laxity and the effect of gravity of the prosthesis [4]. The protocol of this study was approved by the Institutional Review Board of Seoul National University Hospital.
We retrospectively studied each patient's past history, including trauma or surgery, findings on preoperative examinations, diagnosis, surgical procedures and intraoperative findings, and surgical outcomes and complications.
From October 1999 to March 2007, 60 patients with lower eyelid retraction and 497 patients with lower eyelid epiblepharon were surgically treated at Seoul National University Hospital. Among these, 23 eyelids of 18 patients exhibiting both lower eyelid retraction and epiblepharon were enrolled in the study, representing 30% of lower eyelid retraction cases and 3.6% of epiblepharon cases. Two patients (three eyelids) had been previously diagnosed with TAO. On the other hand, 50 patients with TAO were surgically treated during the same period. The operative indications varied for the cases, including eyelid retraction, strabismus, proptosis, and compressive optic neuropathy. Using this approach, two patients (four eyelids) were additionally found to have both lower eyelid retraction and epiblepharon on preoperative examination. These patients underwent orbital wall decompression in both eyes.
Patients ranged in age from 3 to 49 years (mean age, 17.3 years; sex ratio, M:F=8:12). The mean postoperative follow-up period was 20.05 months (range, 1 to 102 months).
The underlying causes of lower eyelid retraction included congenital retraction, congenital fibrosis of the extraocular muscles (CFEOM), post-operative cicatricial retraction, facial nerve palsy, and TAO (Table 1).
Congenital retraction was diagnosed only after other causes of eyelid retraction were excluded. There was no history of uneventful delivery or other trauma including surgery. No patients had abnormalities of the skin or conjunctiva of the lower eyelid, nor did they have proptosis. Seventh nerve and oculomotor nerve function were normal, and the findings of full ophthalmic examinations were normal, with the exception of bilateral congenital blepharoptosis and nasolacrimal duct obstruction in one patient and unilateral congenital nasolacrimal duct obstruction in one patient. No systemic abnormalities were detected, with the exception of one patient with Marfan syndrome, a clinical entity previously unknown to be associated with eyelid retraction [5].
Patients with CFEOM were diagnosed on the basis of downward fixation of one or both eyes and marked blepharoptosis with or without chin elevation. They were subsequently divided into five subgroups according to the classification of Harley et al. [6] (Table 1). The diagnosis of cicatricial retraction was made if there was a definite scar or symblepharon in the lower eyelid with a history of previous operation in the lower eyelid.
All patients underwent eyelid surgery under general (12 patients aged under 20 years of age) or local (six patients aged over 20 years of age) anesthesia. When surgery for lower eyelid epiblepharon associated with lower eyelid retraction was performed in the non-TAO group, correction of lower eyelid retraction with spacer grafts was initially performed. After that, epiblepharon procedures were added intraoperatively if the cornea-touching cilia were not sufficiently resolved. In the TAO group, there were two surgical options. If there was a possibility that orbital decompression would be requested functionally or cosmetically, orbital surgery was performed before any kind of lid surgery. If no orbital decompression was required, the lower eyelid retraction surgery was planned. Two patients who required orbital decompression received general anesthesia. The surgical procedures are described in Table 2. The grafts used for correcting lower eyelid retraction included 16 cases of autogenous ear cartilage, two Medpor® sheets (Porex Surgical Inc., College Park, GA, USA), and one preserved homologous sclera. However, in one case exhibiting a very mild degree of retraction, correction was performed only for the epiblepharon. Epiblepharon repair included cilia-everting suture techniques with or without the excision of skin and muscle [7, 8]. A horizontal skin incision was made 2 mm below the lower lid margin, after which dissection was performed between the lower tarsus and the pretarsal orbicularis oculi. Fixation of subciliary subcutaneous tissue to the inferior margin of the lower tarsus was accomplished with 8-0 nylon (approximately five interrupted sutures), and the skin was repaired.
In all but one patient with congenital retraction (seven eyelids in six patients), lower eyelid retraction repair was accomplished with an autogenous ear cartilage graft, and epiblepharon repair was performed (mean age, 11.7 years; sex ratio, M:F=3:3). The exception was a patient who had a very mild degree of retraction who underwent only epiblepharon repair with skin excision. The mean postoperative follow-up period was 19.8 months. All of the results were positive, and there were no complications, including recurrence (Fig. 1).
Congenital fibrosis of the extraocular muscles (seven eyelids in six patients) patients underwent one of the following treatments: lower eyelid retraction repair with autogenous ear cartilage grafts and without epiblepharon repair (three eyelids in three patients); lower eyelid retraction repair with autogenous ear cartilage grafts and epiblepharon repair (three eyelids in two patients); and lower eyelid retraction repair using a scleral graft (one eyelid) (mean age, 12.7 years; sex ratio, M:F=4:2). The mean postoperative follow-up period was 30.3 months. Epiblepharon was well corrected immediately after the procedure. However, lower eyelid retraction remained in one case where a preserved scleral graft was used to correct lower eyelid retraction and epiblepharon, and scleral grafting was repeated two weeks after the first operation. However, in this patient, both retraction and epiblepharon recurred three years later. Autogenous ear cartilage grafting was performed, and there was no problem during the ensuing 51 months of follow-up. Another instance of retraction recurrence was observed after ten months in a patient who underwent repair of lower eyelid retraction with an autogenous ear cartilage graft and repair of epiblepharon. Another CFEOM patient (Fig. 2), who underwent repair of lower eyelid retraction with an autogenous ear cartilage graft and repair of epiblepharon without excision of the skin or orbicularis muscle, presented with cornea-contacting cilia after three months. The recurrent epiblepharon was treated with a repeat operation, including skin excision, and no recurrence was noted during 13 months of follow-up. There were no other complications other than an overcorrection of lower eyelid retraction.
All patients with cicatricial lower eyelid retraction and epiblepharon (five eyelids in three patients) had undergone previous operations on their lower eyelids, resulting in scars. Therefore, these patients required lengthening of the lower eyelids with spacer grafts in the form of autogenous ear cartilage (three eyelids in two patients) or Medpor® sheets (two eyelids in one patient), (mean age, 19.7 years; sex ratio, M:F=0:3). The results of autogenous ear cartilage grafting were positive during the next 12 months. However, the Medpor® sheets became displaced in both eyelids only two weeks after the operation. These sheets were removed, and retraction and epiblepharon immediately recurred in the left eyelid. However, the patient was lost to follow-up after three months.
The patient with facial nerve palsy (one eyelid in one patient) underwent lower eyelid retraction repair with an autogenous ear cartilage graft and underwent epiblepharon repair without skin or orbicularis muscle excision. The lower eyelid was well positioned after 24 months.
Finally, among the TAO patients (seven eyelids in four patients; mean age, 34.5 years; sex ratio, M:F=1:3), two patients were treated with bilateral orbital decompression because of compressive optic neuropathy or poor cosmesis secondary to proptosis. The other three eyelids (two patients) received direct autogenous ear cartilage grafts. No patients underwent procedures for epiblepharon repair. As shown in Fig. 3, the results were excellent. There was only one instance of lower eyelid retraction overcorrection, and this case presented with favorable cosmesis. Indeed, no recurrences or complications were associated with the orbital decompression procedure.
Eyelid retraction is defined as an abnormality in which the resting position of the upper eyelid is too high or that of the lower eyelid is too low. Most patients have the symptoms of exposure keratopathy such as foreign body sensation, redness, ocular pain, and/or tearing. Thus, other than surgical treatment for functional and cosmetic concerns, the medical treatment of eyelid retraction is also important in alleviating these symptoms and in protecting the globe from exposure and corneal breakdown [1]. Occasionally, other eyelid abnormalities such as entropion or ectropion are combined with retraction, as was seen in our series. Some patients with lower eyelid retraction also have epiblepharon, irrespective of the cause of their lower eyelid retraction, and this may directly irritate the cornea or may worsen the exposure keratopathy. Therefore, the possibility of combined eyelid abnormalities should receive adequate attention.
Epiblepharon is a common congenital eyelid abnormality in Asians, in which a fold of skin and the underlying orbicularis muscle overlap the eyelid margin and push the cilia against the cornea. However, congenital epiblepharon is usually not related to other eyelid abnormalities. Acquired epiblepharon is much less common and has been described only rarely in individual case reports [3, 9]. Epiblepharon combined with lower eyelid retraction is also not well documented.
We found that combined epiblepharon and lower eyelid retraction represented 30% of surgically treated lower eyelid retraction patients and 3.6% of surgically treated epiblepharon patients in this study. It is uncertain whether epiblepharon occurs secondary to lower eyelid retraction or whether patients incidentally have both congenital epiblepharon and lower eyelid retraction. Five cases of epiblepharon resolved after retraction repair, without the need for specific epiblepharon procedures. Epiblepharon was well corrected with only cilia-everting tarsal fixation sutures (ten cases) or with Quickert's sutures (two cases) in 12 of 14 cases, in which we did not perform excision of the redundant skin or the orbicularis muscle. Only one epiblepharon recurrence was noted during follow-up, and it was improved by excision of the skin and orbicularis muscle (Fig. 2). Therefore, combined epiblepharon and lower eyelid retraction may not result from excessive skin and orbicularis muscle, a well known cause of congenital epiblepharon in Asians. It is possible that epiblepharon is acquired rather than congenital, and that lower eyelid retraction is one of the causes of acquired epiblepharon.
The surgical outcomes were satisfactory in all patients with TAO whose operations did not include epiblepharon procedures, four orbital decompressions and three lower eyelid retraction repairs (Fig. 3). Correction of proptosis or lower eyelid retraction also resulted in epiblepharon recovery. These results may account for the epiblepharon seen secondary to TAO. Chang et al. [3] have also described acquired epiblepharon in patients with TAO. They reported 16 eyelids (nine patients) with epiblepharon, of which nine lower eyelids resolved after lower eyelid retraction repair (four cases), orbital wall decompression (three cases), or radiotherapy (two cases). There were no surgical interventions directed at correction of epiblepharon, except for one lower eyelid crease repair and one temporary suture placement.
The pathogenesis of acquired epiblepharon has not been established, but it is thought that the relative forces between the anterior and posterior lamellae of the lower eyelid may play a role. Most patients in our study had a common intraoperative finding of lower eyelid tissue stiffness, so-called "fibrosis", secondary to congenital retraction, CFEOM, TAO, and cicatrization [5, 10, 11]. While the fibrotic characteristics of the posterior lamella may lead to lower eyelid retraction, the anterior lamella remains in a normal position and therefore overlaps the eyelid margin and pushes the cilia against the cornea. This mechanism is also supported by the high rate of patients with CFEOM in our study, a condition in which the displacement of muscle fibers by collagen fibers is the typical histopathologic finding [10]. Six of 20 patients were diagnosed with CFEOM, the most common cause of lower eyelid retraction other than congenital retraction. Indeed, there were three recurrences, which accounted for all of the recurrent cases in our study. These results may suggest that the idiopathic fibrotic processes of CFEOM contribute to both initial and recurrent epiblepharon and retraction.
A discrepancy of forces between the anterior and posterior lamellae has also been suggested in patients with anophthalmic retraction and entropion. The weight of the ocular prosthesis on the inferior fornix imposes a constant downward force on the posterior lamella, but the anterior lamella remains in position, resulting in lower eyelid retraction and entropion [4]. Indeed, Chang et al. [3] noted that absence of a lower eyelid crease, which is frequently observed in Asians, allows for extension of the orbital fat superiorly to the inferior border of the tarsus; this supports the anterior lamella. These investigators claimed that any increase in the support of the anterior lamella, especially in the setting of posterior lamellar retraction such as TAO, could lead to acquired epiblepharon.
There were limitations to our study. First, the sample size was relatively small. Second, we conducted a noncomparative study. While we included all patients with lower eyelid retraction or epiblepharon, there was only one patient who underwent epiblepharon repair without retraction repair. He had very mild retraction on preoperative examination, and the retraction resolved after dissection between the orbicularis muscle and the tarsus, so he did not require any further procedures. Finally, there were four patients who underwent unilateral retraction repair and bilateral epiblepharon repair. This suggests a lack of association between retraction and epiblepharon, which directly opposes our assumption. However, no or very little skin and orbicularis muscle were excised in the retracted eyelid, and there was no asymmetry between the eyelid positions after surgery. Thus, retraction is thought to have played a minor role in the epiblepharon formation, even though congenital epiblepharon was seen bilaterally.
In summary, epiblepharon can be seen in conjunction with retraction, especially in congenital retraction, CFEOM, or TAO. The fact that epiblepharon resolved after correction of lower eyelid retraction supports a causal role of eyelid retraction in the development of epiblepharon. It seems reasonable to initially surgically correct lower eyelid retraction and then to perform cilia-rotating tarsal fixation suture and excision of the skin and orbicularis muscle if requested.
Notes
This study was presented at the 98th Meeting of the Korean Ophthalmological Society, November 2007, Ilsan, Korea.
REFERENCES
2. Bosniak S. Principles and practice of ophthalmic plastic and reconstructive surgery. 1996. Philadelphia: WB Saunders; p. 438-466.
3. Chang EL, Hayes J, Hatton M, Rubin PA. Acquired lower eyelid epiblepharon in patients with thyroid eye disease. Ophthal Plast Reconstr Surg 2005;21:192-196.


4. Moon JW, Choung HK, Khwarg SI. Correction of lower lid retraction combined with entropion using an ear cartilage graft in the anophthalmic socket. Korean J Ophthalmol 2005;19:161-167.


5. Collin JR, Allen L, Castronuovo S. Congenital eyelid retraction. Br J Ophthalmol 1990;74:542-544.



6. Harley RD, Rodrigues MM, Crawford JS. Congenital fibrosis of the extraocular muscles. J Pediatr Ophthalmol Strabismus 1978;15:346-358.


7. Woo KI, Yi K, Kim YD. Surgical correction for lower lid epiblepharon in Asians. Br J Ophthalmol 2000;84:1407-1410.



8. Khwarg SI, Choung HK. Epiblepharon of the lower eyelid: technique of surgical repair and quantification of excision according to the skin fold height. Ophthalmic Surg Lasers 2002;33:280-287.


10. Roh YB, Kim JH, Oum BS, Baek SY. Clinical and histological study of extraocular muscle in congenital fibrosis syndrome. J Korean Ophthalmol Soc 1996;37:1907-1914.
Fig.┬Ā1
Congenital lower eyelid retraction and epiblepharon. (A) Lower eyelid retraction and epiblepharon were observed in the preoperative photograph of a nine-yr-old boy. (B) Bilateral autogenous ear cartilage grafting and cilia-everting suturing were performed. After one month, the retraction and epiblepharon were resolved. (C) An eight-yr-old girl had unilateral retraction in the right lower eyelid and bilateral epiblepharon. (D) She underwent autogenous ear cartilage grafting in her right lower eyelid. Epiblepharon repair was performed on both eyelids during the operation. The postoperative results were good.
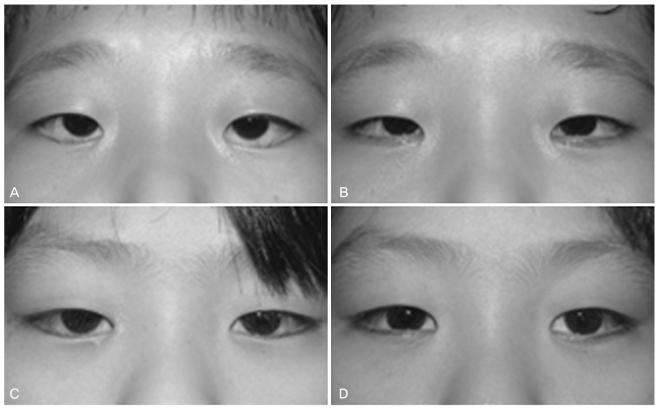
Fig.┬Ā2
Congenital fibrosis of the extraocular muscles. (A) A five-yr-old boy had lower eyelid retraction and epiblepharon, hypotropia and exotropia, and blepharoptosis in the left eyelid. He first underwent lower eyelid retraction repair using an autogenous ear cartilage graft. The surgeon then concluded that epiblepharon procedures were necessary. Cilia-everting tarsal fixation sutures were placed. (B) Epiblepharon recurred at four months postoperatively, although the lower eyelid was well positioned. (C) The patient underwent repeat epiblepharon repair on his left eyelid, including skin and orbicularis muscle excision. The photograph, taken only one week post-operatively, noted well-everted cilia and a prominent incision line along the lower eyelid margin. However, the line faded during follow-up.
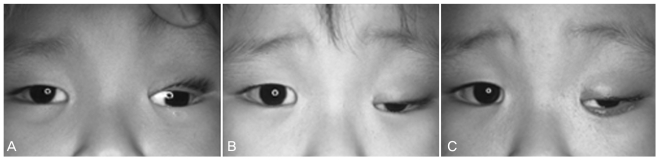
Fig.┬Ā3
Thyroid-associated ophthalmopathy (TAO). The patient complained of a proptotic and surprised look, although her hyperthyroidism was well controlled. (A) She was noted to have proptosis and lower eyelid retractions with epiblepharon. (B) Orbital decompression was performed in order to improve her appearance, and the outcome was good. There were no complications during eight months of follow-up.





 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print




