 |
 |
| Korean J Ophthalmol > Volume 24(6); 2010 > Article |
Abstract
A 60-year-old diabetic patient transferred to our retina clinic for a regular follow-up for diabetic retinopathy. He had uneventful cataract surgery at the time of pars plana vitrectomy in the right eye due to diabetic retinopathy at a private ophthalmologic hospital. Six months after the surgery, neovascular glaucoma with hyphema developed in the right eye and an Ahmed valve was implanted at our hospital. Ten months after cataract surgery, we found opacification of the intraocular lens (IOL) which was causing significant visual disturbance. At the time, the best corrected visual acuity (BCVA) in the right eye was hand motion. The IOL was explanted 45 months after the operation. Five months after explantation, the BCVA was 0.06. Unfortunately, pathologic analysis was not performed. Patient-related factors such as an anterior chamber reaction caused by hyphema might have been responsible for the opacification. To our knowledge, there are no previous reports of opacification of the Akreos Adapt IOL.
The opacifications of an intraocular lens (IOL), necessitating the removal or exchange of the implanted IOL, has been reported in some hydrophilic acrylic IOLs [1-11]. According to associated studies, granular deposits responsible for the opacification were found on the optical surface or within optical material several months or several years after the operation [11]. With an immunohistochemistry or surface analysis, the surface deposition of minerals has been reported. Some studies also reported that there was a correlation between the opacification and the constituents in the optical device. However, little is known about the mechanisms by which the opacification of hydrophilic acrylic IOLs occurs. We observed a case of the opacification of a hydrophilic acrylic IOL (Akreos Adapt, Bausch & Lomb, Rochester, NY, USA). To our knowledge, there was no prior report of an opacification in that IOL.
A 55-year-old man with a 28-year history of diabetes was referred to our retina clinic for a regular ophthalmic examination for diabetic retinopathy. At the time of the first visit, the patient presented with proliferative diabetic retinopathy in both eyes and clinically significant macular edema. The patient was also receiving peritoneal dialysis for chronic renal failure. He had undergone pars plana vitrectomy for proliferative diabetic retinopathy in combination with phacoemulsification and implantation of a hydrophilic acrylic IOL in the capsular bag of the right eye at another hospital two months prior. In addition, the patient received panretinal photocoagulation. At the time of his first visit, the best corrected visual acuity (BCVA) was 0.08 in the right eye. Four months later, the BCVA of the right eye had decreased to a finger count at 10 cm and the intraocular pressure was 38 mmHg as measured by applanation tonometer. The patient was diagnosed with neovascular glaucoma accompanied by hyphema. He underwent Ahmed valve implantation through pars plana vitrectomy at our hospital immediately after the diagnosis of neovascular glaucoma. Thereafter, the corrected visual acuity of the right eye was maintained at 0.08.
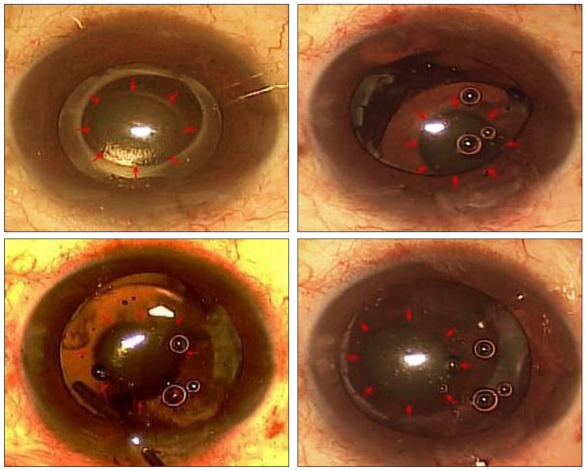
IOL opacification, causing decreased visual acuity, was found five months following the surgery for glaucoma (ten months following the implantation of the IOL) during monitoring of the clinical course (Fig. 1). There was a concurrent presence of microhyphema as we monitored the clinical course. However, after the disappearance of hyphema, his visual acuity of the right eye dropped to hand motion and did not improve. The IOL was explanted from the right eye 45 months after implantation. For the explantation of the lens, the fibrotic anterior capsule was released by endoscissors under viscoelastics. The haptics were separated from the optics and two of them were explanted. The other two haptics were not explanted because we were concerned about zonular dialysis. The optics were relieved from the capsular bag by manual dissection with a spatula and viscodissection. It was then cut into small pieces with DeWecker scissors. The IOL was explanted, piece by piece, through a 3.0 mm corneal incision. A hydrophobic acrylic IOL (YA-60BB; hoya Inc., Tokyo, Japan) was then implanted into the sulcus. There was a well-circumscribed centrally and paracentrally located opacification of the original IOL optic. The opacification was generalized, white, homogenous and it affected the entire surface inside of the IOL. Postoperatively, the patient did not exhibit specific complications and the visual acuity improved to 0.04. Six months after the operation, the corrected visual acuity was maintained at 0.06 due to macular edema.
To date, the exchange of IOLs due to postoperative opacification has been reported in many cases. These hydrophillic acryl IOLs include Hydroview (Bausch & Lomb) [1,2], ACRL-60 (Ophthalmed Inc., Carlsbad, NM, USA) [12], MemoryLens (Ciba Vision, Duluth, GA, USA) [3-5] and AquaSense (Ophthalmic Innovations International, Ontario, CA, USA) [9,10]. Several tens of cases of postoperative opacification have also been reported following the use of SC60B-OUV (Medical Developmental Research, Clearwater, FL, USA) [6-8]. In addition, two cases of postoperative opacification after implantation of Centerflex 570H (Rayner, East Sussex, UK) have been reported [13]. It is theorized that the deposition of minerals, including Ca2+, on the optical surface of IOLs produces the opacification. In the case outlined here, IOL opacification developed in the optical substance of Akros Fit (Bausch & Lomb) [14]. However, no clinically notable decrease of visual acuity was noted. Therefore, an exchange of IOLs was not performed.
It is important to note that histopathological assessments were not performed for IOL that were removed in the current study. Considering that the clinical characteristics of the current case are analogous to previous reports, the deposition of minerals, including Ca2+, on the surface of optical part is assumed to be the causative factor [1-12,14]. Werner et al. [1] showed that the opacification of IOLs that were implanted in the eye following cataract surgery was not associated with the substance used during surgery. Recently, Sher et al. [15] suggested that the intraoperative use of Viscoat (Alcon, Fort Worth, TX, USA) has a facilitating role in the development of late opacification of the Hydroview (Bausch & Lomb) IOL.
Based on results of studies that have been conducted up to the present, a higher rate of opacification was observed in patients with systemic diseases such as diabetes [2,15]. Ha et al. [16] reported that all three patients with Ca2+ deposition on the surface of their hydrophilic acrylic IOLs had a proliferative diabetic retinopathy. Pombo et al. [17] suggested that the occurrence of proliferative ophthalmic diseases is associated with some growth factors and some of these exist within the vitreous body. In cases of proliferative diabetic retinopathy, adenosine triphosphate is released from the retinal vascular cells during hypoxia. This triggers the increased Ca2+ influx. Besides, in the vitreous body of patients with proliferative diabetic retinopathy a higher concentration of protein is identified. This is involved in the production of angiotensin I and elevates the concentration of serum Ca2+. With the activation of some growth factors within the vitreous body, inositol phosphate is synthesized and cellular proliferation provoked. According to Werner et al. [6] five of eighteen patients who developed opacification of IOLs following cataract surgery were noted to have diabetes. However, the authors noted that no methods were available to establish a correlation between these complications and diabetes. Interestingly, in cases in which the disease duration of diabetes is prolonged the opacification occurs rapidly. In patients who had a proliferative diabetic retinopathy opacification developed more rapidly and with a greater severity. In the current case, there was a 28-year history of diabetes and proliferative diabetic retinopathy in both eyes. The type and duration of the diseases might be associated with the development of opacification in this case. It may also be that the inflammatory responses due to the anterior chamber bleeding that developed during the clinical course in some cases affected the opacification of IOLs. Further histopathological studies are warranted to analyze the opacification of the Akreos Adapt IOLs. With the high frequency of postoperative opacification observed, it may be better to use hydrophobic acrylic IOLs rather than hydrophilic ones.
We report our case of the opacification of the hydrophilic Akreos Adapt IOL, which was not previously reported. In patients with diabetes mellitus, the substances forming IOLs must be considered for cataract surgery. Further histopathological studies are warranted to analyze the causes of opacification of the hydrophilic Akreos Adapt IOL.
Notes
This article was presented as a poster in parts at the 100th autumn meeting of Korean Ophthalmological Society, November 2008, Goyang, Korea and the ASCRS symposium on Cataract, IOL and Refractive Surgery, San Francisco, CA, USA, April 2009.
REFERENCES
1. Werner L, Apple DJ, Escobar-Gomez M, et al. Postoperative deposition of calcium on the surfaces of a hydrogel intraocular lens. Ophthalmology 2000;107:2179-2185.


2. Pandey SK, Werner L, Apple DJ, Gravel JP. Calcium precipitation on the optical surfaces of a foldable intraocular lens: a clinicopathological correlation. Arch Ophthalmol 2002;120:391-393.


3. Tehrani M, Mamalis N, Wallin T, et al. Late postoperative opacification of MemoryLens hydrophilic acrylic intraocular lenses: case series and review. J Cataract Refract Surg 2004;30:115-122.


4. Neuhann IM, Werner L, Izak AM, et al. Late postoperative opacification of a hydrophilic acrylic (hydrogel) intraocular lens: a clinicopathological analysis of 106 explants. Ophthalmology 2004;111:2094-2101.


5. Hunter B, Werner L, Memmen JE, Mamalis N. Postoperative localized opacification of the new MemoryLens design: analyses of an explant. J Cataract Refract Surg 2005;31:1836-1840.


6. Werner L, Apple DJ, Kaskaloglu M, Pandey SK. Dense opacification of the optical component of a hydrophilic acrylic intraocular lens: a clinicopathological analysis of 9 explanted lenses. J Cataract Refract Surg 2001;27:1485-1492.


7. Macky TA, Werner L, Soliman MM, et al. Opacification of two hydrophilic acrylic intraocular lenses 3 months after implantation. Ophthalmic Surg Lasers Imaging 2003;34:197-202.


8. Frohn A, Dick HB, Augustin AJ, Grus FH. Late opacification of the foldable hydrophilic acrylic lens SC60B-OUV. Ophthalmology 2001;108:1999-2004.


9. Izak AM, Werner L, Pandey SK, Apple DJ. Calcification of modern foldable hydrogel intraocular lens designs. Eye (Lond) 2003;17:393-406.


10. Werner L, Hunter B, Stevens S, et al. Role of silicon contamination on calcification of hydrophilic acrylic intraocular lenses. Am J Ophthalmol 2006;141:35-43.


11. Werner L. Causes of intraocular lens opacification or discoloration. J Cataract Refract Surg 2007;33:713-726.


12. Kim HG, Lee SH, Choi YJ. Late postoperative opacification of the foldable hydrophilic acrylic intraocular lens, ACRL-160. J Korean Ophthalmol Soc 2003;44:315-320.
13. Hong JW, Roh IH, Bae SR. Opacification of hydrophilic acrylic intraocular lens. Korean J Optom Vis Sci 2007;6:68-71.
14. Kotagiri AK, Nyunt KM, Fox P. Surface deposits on the optic of an Akreos Fit IOL. J Cataract Refract Surg 2007;33:1678-1679.


15. Sher JH, Gooi P, Dubinski W, et al. Comparison of the incidence of opacification of Hydroview hydrogel intraocular lenses with the ophthalmic viscosurgical device used during surgery. J Cataract Refract Surg 2008;34:459-464.


16. Ha MS, Kang BD, Myung NH, Chang MH. Postoperative deposition of calcium on the surface of a hydrophilic acrylic IOL in diabetic patients. J Korean Ophthalmol Soc 2002;43:375-380.



 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print




