Orbital Metastatic Angiosarcoma
Article information
Abstract
We report a case of a 48-year-old man who developed metastatic angiosarcoma in her left orbit. A 48-year-old man was first sent to us for a check up of proptosis of the left eye. A left orbital tumor was recognized on orbital computed tomography scans. The open biopsy showed angiosarcoma. Chest X-ray films and thoracic computed tomography showed an abnormal mass in the left inferior lung field. Angiosarcoma was confirmed by transbronchial lung biopsy. In summary, we believed that the orbital tumour was an initial symptom of the metastasis ensuing from the lung angiosarcoma.
The first descriptions of orbital and ocular metastases were made by Horner in 1864 and Perle in 1872 [1,2]. These metastases constitute 0, 5-5, 0% of all orbital tumours [3]. For the majority sites responsible for these metastases, they are carcinoma, the breast and the lung are the first primary sites responsible for these metastases (breast carcinoma in woman and lung or digestive cancer in man), however, metastatic orbital tumors presenting as the first sign of disseminate cancer are a rare event [1-3]. Angiosarcomas comprise 1% of all soft tissue sarcomas, with an orbital incidence of 3% of those cases. The majority is primary angiosarcoma; only two previous case of metastatic angiosarcoma to the orbit has been described [2]. Treatment options and efficacy is not well understood.
Case Report
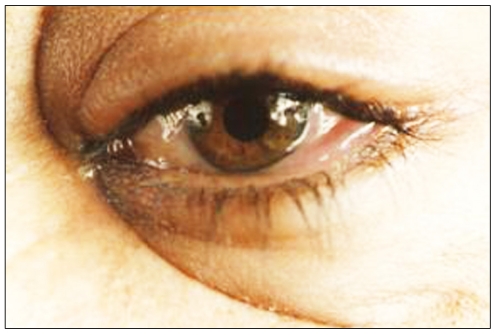
A 48-year-old man smoking for 30 years was due to a pack a day presented a one-month history of exophthalmia, chemosis (Fig. 1) and diplopia. An ophthalmic examination shows a visual acuity as 20/20 in OD, and in 15/20 OS check pupils is normal and exophthalmometry shows 6 mm proptosis in OS. Motility examination on admission demonstrated a left oculomotor limitation in all direction, accompanied with pain and a ledger left ptosis. The fundus examination was normal. A neurological examination on admission demonstrated a left oculomotor palsy, accompanied with pain.
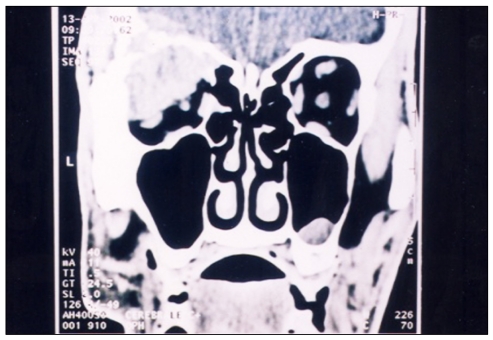
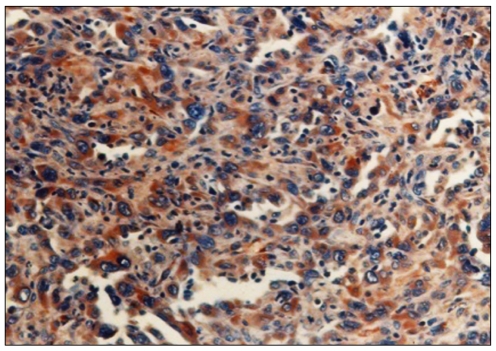
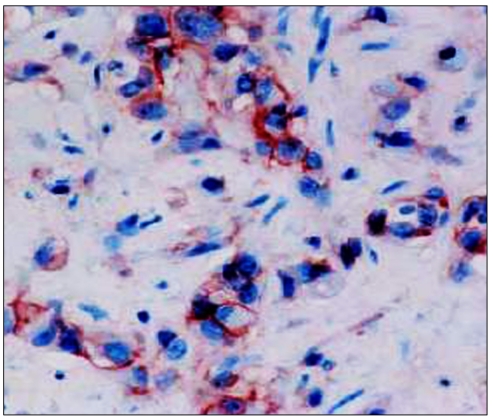
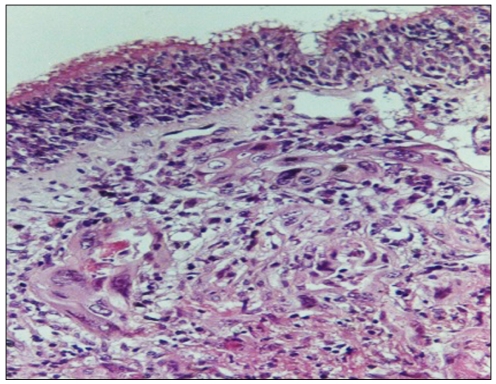
Computed tomography (CT) showed a left superior orbital mass causing bone destruction, was extended to brain (Fig. 2), the radiologist suspected a metastasis with unknown primary site. Therefore, a more thorough systemic evaluation was started to detect primary malignancy. The immunohistologic staining of the incisional biopsy specimen showed angiosarcoma, the tumor cells were positive for factor VIII and CD31 (Figs. 3-5). The biopsy was complicated by inflammatory edema of the orbit (Fig. 6). A chest X-ray film completed by thoracic CT has shown an abnormal mass in the left posterior and inferior lung field (Fig. 7). Angiosarcoma has been diagnosed by transbronchial lung biopsy in immunohistological study (Fig. 8). The left orbital tumor was thought to be a metastasis caused by the lung cancer.
The patient received radiation therapy for the metastatic orbital tumor with a total dose 2,000 cGy in 10 fractions of 200 cGy per fraction and chemotherapy (cisp1atin 100 mg/m2 IV; day 1 + etoposide 100 mg/m2; days 1-3 repeated every 4 weeks for 2 months) for the lung cancer. However, he died 3 months after initial treatment because of the progression of the primary lesion as Weil as the progressive systemic metastasis in the brain.
Discussion
Angiosarcomas are malignant neoplasms derived from endothelial cells of arteries, or veins. The origin of these tumors is unknown. The metastatic orbital angiosarcomas is exceptional, we believe this is the third reported case of metastatic angiosarcoma to the orbit [1,2].
The confirmation is done by histopathologic evaluation, when cytokeratin is negative or focally positive with vimentin reactivity, a vascular tumor should be suspected and confirmed with vascular markers, CD31, CD34, and factor VIII [3]. These are the endothelial-specific immunologic markers with variable specificity and sensitivity. Factor VIII-related antigen, in spite of its high specificity, is believed to be relatively insensitive, particularly in malignant vascular tumors. CD34 was reported to be a specific and sensitive endothelial marker, but it also reacts with nonvascular soft tissue neoplasm, including epitheloid sarcoma, malignant peripheral nerve sheath tumor, leiomyosarcoma, and clear cell sarcoma. CD31 has been shown to be a highly specific and sensitive endothelial marker that reacts rarely and only weakly with nonvascular tumours [3].
The optimal therapy for angiosarcoma is not established. Resection, radiation, or combined resection and radiation were used in treating the angiosarcoma of the cranium, complete surgical resection in other sites followed by radiation therapy results better in long-term control of disease thane surgery alone. There may be reduction in recurrence with adjuvant chemotherapy, although the most active agents are not known [1]. Paclitaxel appears to be highly specific in dermal angiosarcoma, but is palliative [4]. Chemotherapy may be a useful adjunct to surgery and/or radiation therapy in the management of angiosarcoma; however, chemotherapy alone is unlikely to be curative [1]. Nevertheless, we believe that angiosarcoma of the orbit may have a worse prognosis than angisarcoma of bones other than the cranium, because the tumour may secondarily involve the brain and the patient dies with increased intracranial pressure [5], as did our case.
Notes
No potential conflict of interest relevant to this article was reported.