 |
 |
| Korean J Ophthalmol > Volume 24(6); 2010 > Article |
Abstract
Purpose
To compare the intraoperative performances and postoperative outcomes of cataract surgery performed with longitudinal phacoemulsification and torsional phacoemulsification in moderate and hard cataracts.
Methods
Of 85 patients who had senile cataracts, 102 eyes were operated on using the Infiniti Vision System. Preoperative examinations (slit lamp examination, mean central corneal thickness, and central endothelial cell counts) were performed for each patient. Cataracts were subdivided into moderate and hard, according to the Lens Opacities Classification System III grading of nucleus opalescence (NO). Eyes in each cataract group were randomly assigned to conventional and torsional phaco-mode. Intraoperative parameters, including ultrasound time (UST), cumulative dissipated energy (CDE), and the balanced salt solution plus (BSSP) volume utilized were evaluated. Best corrected visual acuity (BCVA) was checked on postoperative day 30; mean central corneal thickness and central endothelial cell counts were investigated on postoperative days 7 and 30.
Results
Preoperative BCVA and mean grading of NO showed no difference in both groups. Preoperative endothelial cell count and central corneal thickness also showed no significant difference in both groups. In the moderate cataract group, the CDE, UST, and BSSP volume were significantly lower in the torsional mode than the longitudinal mode, but they did not show any difference in the hard cataract group. Torsional group showed less endothelial cell loss and central corneal thickening at postoperative day seven in moderate cataracts but showed no significant differences, as compared with the longitudinal group, by postoperative day 30.
Phacoemulsification is the main procedure of modern cataract surgery. Ultrasonic (US) energy during phacoemulsification can carry the risk of endothelial cell loss and tissue damage, especially in hard cataracts. In the conventional US mode, the phaco tip moves forward and backward, and the US energy comes from longitudinal movement of the tip. The jackhammer effect plays an important part, and the cavitation effect plays minimal role in longitudinal phacoemulsification [1]. The longitudinal mode can produce a repulsion effect, because the phaco tip pushes the nucleus away when it moves forward. However, the torsional ultrasound features oscillating rotary or side-to-side movement, and reduces the repulsion of the lens fragments, therefore improving the followability of nuclear material into the phacoemulsification tip [2]. The OZil (Infinity Vision System; Alcon Laboratories, Fort Worth, TX, USA) torsional platform includes a dedicated handpiece that produces rotary oscillations of the phacoemulsification tip with a frequency of 32 Kz [3].
In previous reports, the torsional phacoemulsification using OZil torsional equipment provided a lower level of US time and energy, and more effective phacoemulsification than the conventional methods [3,4]. We designed a study to compare the intraoperative and postoperative clinical performances between torsional and conventional phacoemulsification to verify the efficiency of torsional phacoemulsification in moderate and hard cataracts.
This randomized comparative study was conducted from July 2007 to February 2008. Patients with a diagnosis of senile cataract were randomly assigned to the conventional US group or the torsional US group.
Exclusion criteria included: patients with a history of ocular inflammatory disease or previous intraocular surgery, patients with an endothelial cell count of less than 1,500 cells/mm2 before surgery, and patients who underwent eventful cataract operation. After informed consent was obtained, standard preoperative examinations were performed.
The grading of cataracts was determined according to the Lens Opacities Classification System III. Eyes with nuclear opalescence (NO) grades between 2 and 5 were included in the study. The examined eyes were subdivided into moderate (NO2 Ōēż, Ōēż NO4) and hard (NO4 <, Ōēż NO5) cataracts.
All surgeries were performed using the Infiniti Vision System (Alcon Laboratories), and the same US and fluidic settings were used by a single experienced surgeon (KMK). All patients received sub-tenon anesthesia with 2% lidocaine prior to surgery. A 2.75-mm self-sealing clear corneal incision was made on the temporal or superior side and a solution of sodium hyaluronate 3.0% and chondroitin sulfate 4.0% (Viscoat) was used in the surgery. A routine phaco-chop technique was used either with the US pulse mode (60 p/sec) or torsional continual mode. The microtip 0.9 mm angled Aspiration Bypass System phaco tip (15 degrees) was used with a standard setting. For the torsional mode, 100% amplitude was selected. For the US pulse mode, a maximum power of 60% and pulse frequency of 60 pulses per second were selected. The vacuum limit was 400 mmHg, and the aspiration flow rate was 40 mL/min. Balanced salt solution (BSS plus; Alcon Laboratories) was used as irrigation solution. An intraocular lens was inserted with the injector through the main incision wound into the capsular bag and the posterior chamber. No sutures were performed on the clear corneal wound.
The main system parameters were mean US time (UST), cumulative dissipated energy (CDE), and the amount of BSS plus utilized. The UST, CDE, and BSS plus amount values, which were automatically calculated by the device, were checked respectively. After the surgery, levofloxacin (Cravit┬«, Santen, Osaka, Japan), diclofenac sodium (Diclan┬«, Hanlim Pharm., Seoul, Korea), and prednisolone acetate eye drops (Flarex┬«, Alcon Laboratories) four times a day for two weeks were prescribed. Patients were examined on postoperative days 1, 7, and 30. The postoperative best corrected visual acuity (BCVA) was documented. The central corneal thickness was measured using US pachymetry (Quantel Medical, Clermont-Ferrand, France) and the central endothelial cell count was measured using a non-contact special microscope (Noncon Robo SP 8000TM; Konan, Hyogo, Japan) at preoperative, and postoperative days 7 and 30. The center method was used for cell counting and about 50 to 80 cells were counted manually in 0.03 mm2 of the central corneal endothelium in a single exam. Endothelial cell loss (ECL) was evaluated as follows: ECL = (preoperative cell count-postoperative cell count)/preoperative cell count ├Ś 100%)
Statistical analysis was performed using SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA). Comparisons between the two groups were performed using independent t-test or Mann-Whitney test, while analysis of preoperative and postoperativeerative changes in same group were performed using Wilcoxon test. A p < 0.05 was considered statistically significant.
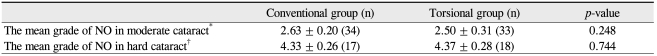
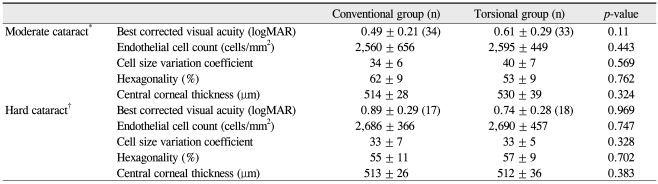
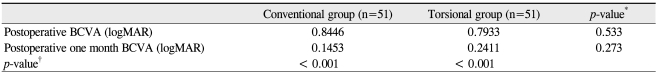
A total of 102 eyes (85 patients), 51 in the US group and 51 in the torsional group were enrolled in the study. The mean age of all patients was 66.0 ┬▒ 9.8 years (standard deviation, SD). The mean age of patients in the conventional and torsional groups were 66.8 ┬▒ 10.8 years (SD) and 65.4 ┬▒ 9.4 years (SD) (p = 0.753), respectively. Thirty eight patients were male and 64 were female. The nuclear opalescence grades are shown in Table 1. There were no differences of mean grade in nuclear opacity in both groups (moderate cataract, p = 0.248; hard cataract, p = 0.744). Preoperative BCVA, central endothelial cell count, cell size variation coefficient, hexagonality, and central corneal thickness were not significantly different between the conventional and torsional groups (Table 2).
In moderate cataract, the mean UST (39.1 ┬▒ 9.1 in the torsional group, 61.3 ┬▒ 10.0 in the conventional group; p = 0.023), CDE (2.40 ┬▒ 0.64 in the torsional group, 5.30 ┬▒ 1.65 in the conventional group; p = 0.014), and BSS plus usage amount (140.4 ┬▒ 17.0 in the torsional group, 251.3 ┬▒ 31.6 in the conventional group; p = 0.010) were significantly lower in the torsional group. However, there was no significant difference between the two groups in treating hard cataracts (Table 3).
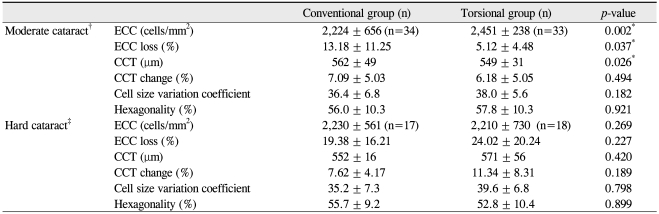
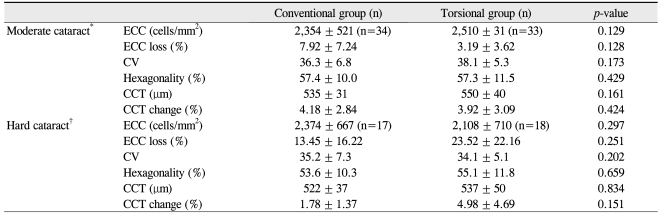
In moderate cataracts, endothelial cell count (ECC) loss (5.12 ┬▒ 4.48% in the torsional group, 13.18 ┬▒ 11.25% in the conventional group; p = 0.037) and central corneal thickness (CCT; 549 ┬▒ 31 in the torsional group, 562 ┬▒ 49 in the conventional group; p = 0.026) at the one week postoperative exam were significantly lower in the torsional group than in the conventional group, which turned out to be not significantly different by one month after operation. Meanwhile, in hard cataracts, ECC loss and CCT showed no differences between the two groups until one month after operation (Table 4). The cell size variation coefficient and hexagonality of the endothelium also showed no significant differences in the two groups at postoperative one week and one month exams (Tables 4 and 5). Intraoperative complications, postoperative anterior chamber reactions more than grade 2, and corneal edema, which obscure iris details, were not observed in either group.
In both the conventional and torsional groups, best-corrected visual acuities (logarithm of the minimum angle of resolution [log MAR]) at the one month postoperative exam were significantly better than preoperative BCVA (log MAR). These improvements were quite similar between groups (Table 6).
Our study showed that torsional phacoemulsification in moderate cataracts was equally effective and a safer procedure, as compared with conventional phacoemulsification. The aim of the recent phacoemulsification research is to reduce phaco energy and shorten the phaco time [5,6]. Numerous methods to minimize the phaco energy have been designed. Examples include non-ultrasonic energy devices, such as NeoSoniX-generated tip rotation [7], and pulse water-jet technology, such as Aqualase [8]. Several chopping techniques have also been developed with the aim of lowering phaco energy and phaco time [9-14].
In torsional phacoemulsification, the side-to-side stroke has a cutting effect, which induces no repulsion. Although the frequency of torsional phacoemulsification is lower (32 kHz) than traditional phacoemulsification (40 kHz), the reduction of the repulsive effect and cutting in the lateral direction by torsional phacoemulsification make it efficient. However, there have been debates about the comparative efficacy and safety of torsional mode US in hard nucleus cataracts, as compared to longitudinal mode.
Recently, many authors have suggested a better efficiency by the torsional mode rather than longitudinal mode. It has been demonstrated that CDE and endothelial cell loss in torsional mode were lower than those with conventional mode in cataracts of all NO grades [3]. Also, a superior efficiency and safety of torsional phacoemulsification was demonstrated in hard nucleus samples [4]. Our result presented a significantly lower CDE, less BSS plus volume used, and lower phaco time in torsional mode for moderate cataracts, as well as lower endothelial cell loss during the early postoperative period, with no difference observed at one month. This result implies that torsional phacoemulsification is more efficient and is at least equally safe, as compared to conventional phacoemulsification in moderate cataracts. The BSS plus volume used in torsional mode was significantly lower than that in conventional mode in only moderate cataracts. It seems plausible that increasing nuclear followability might lower phaco time in torsional mode, resulting in a reduction of the BSS plus amount utilized. Lower CDE and phaco time are considered to be involved in lower endothelial cell loss in moderate cataracts. While, there were no statistically significant differences in all mechanic and biologic parameters in hard cataracts, endothelial cell loss tended to increase in torsional mode, which did not correspond with previous reports [3,4]. It is possible that the shearing effect might not be as effective as the Jackhammer effect in hard cataracts, because US power in torsional phacoemulsification does not act on the nucleus perpendicularly. The harshness of phacoemulsification in hard nucleus samples might be due to more repulsion, resulting in endothelial damage in both phaco-modes. To verify the safety and efficiency of torsional mode in hard nucleus samples definitively, a large number of comparative studies would be required.
Considering the frequency of torsional (32 kHz) and longitudinal (40 kHz) mode and cutting pattern (torsional mode cuts both sides, while longitudinal mode cuts forward uni-direction), the CDE in torsional phacoemulsification would theoretically be 40% of the value in longitudinal phacoemulsification, based on the same phaco time. This finding may suggest that the CDE in torsional mode was less than the longitudinal mode in moderate cataract.
This study is limited by a small sample size in hard cataracts. Nevertheless, the findings have meaningful clinical relevance to support the efficiency and safety of torsional phacoemulsification in medium density cataracts. In conclusion, torsional phacoemulsification was revealed to be more efficient and safer in moderate cataracts, as compared with conventional longitudinal phacoemulsification.
REFERENCES
1. Zacharias J. Role of cavitation in the phacoemulsification process. J Cataract Refract Surg 2008;34:846-852.


2. Davison JA. Cumulative tip travel and implied followability of longitudinal and torsional phacoemulsification. J Cataract Refract Surg 2008;34:986-990.


3. Liu Y, Zeng M, Liu X, et al. Torsional mode versus conventional ultrasound mode phacoemulsification: randomized comparative clinical study. J Cataract Refract Surg 2007;33:287-292.


4. Zeng M, Liu X, Liu Y, et al. Torsional ultrasound modality for hard nucleus phacoemulsification cataract extraction. Br J Ophthalmol 2008;92:1092-1096.



5. Domingues FG, Moraes HV Jr, Yamane R. Comparative study of the density of corneal endothelial cells after phacoemulsification by the "divide and conquer" and "quick chop" techniques. Arq Bras Oftalmol 2005;68:109-115.


6. Xie LX, Yao Z, Huang YS, Ying L. Corneal endothelial damage and its repair after phacoemulsification. Zhonghua Yan Ke Za Zhi 2004;40:90-93.

7. Vasavada AR, Raj SM, Lee YC. NeoSoniX ultrasound versus ultrasound alone for phacoemulsification: randomized clinical trial. J Cataract Refract Surg 2004;30:2332-2335.


8. Mackool RJ, Brint SF. AquaLase: a new technology for cataract extraction. Curr Opin Ophthalmol 2004;15:40-43.


9. Verg├®s C, Llevat E. Laser cataract surgery: technique and clinical results. J Cataract Refract Surg 2003;29:1339-1345.


10. G├╝ell JL, V├Īzquez M, Lucena J, et al. Phaco rolling technique. J Cataract Refract Surg 2004;30:2043-2045.


Table┬Ā1
Nuclear opalescence grading distribution and mean nuclear opalescence (NO) grading of all patients
Table┬Ā2
Preoperative best corrected visual acuity, endothelial cell status, and central corneal thickness
Table┬Ā3
Cumulative dissipated energy (CDE), ultrasound time (UST), and balanced salt solution (BSS) amount in the two groups during surgery

- TOOLS



 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print




