Optic nerve gliomas (ONGs) are the most common tumors of the optic pathways in childhood. They are usually diagnosed early in life, at a median age of 4.5 years, and rarely present after age 10. The prognosis is highly variable. ONGs are usually slow-growing tumors that sometimes regress spontaneously, but can occasionally progress rapidly [1]. The signs and symptoms that occur in patients with ONGs include decreased visual function, proptosis, optic disc swelling or pallor, and strabismus. Chronic compression of the vessels may give rise to central retinal vein occlusion, venous stasis retinopathy, optociliary shunt vessels, and rarely, rubeosis iridis with neovascular glaucoma (NVG) [2]. NVG is a rare complication of ONGs, two different cases have been reported. We report a case of NVG that developed in a patient who underwent stereotactic radiosurgery for an ONG.
Case Report
A 13-year-old girl was referred to our glaucoma clinic for uncontrolled intraocular pressure (IOP). She had a history of bilateral lateral rectus and inferior oblique muscle resection at 3 years of age to treat exotropia, with bilateral inferior oblique muscle overactivity detected at 3 months of age. Her visual acuity had been 20/80 (OD), 20/50 (OS), and corrected to 20/25 (OU) when she was 3 years old.
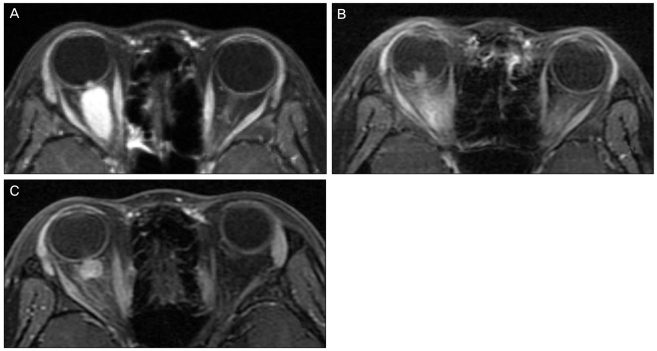
Eight years later, the exotropia recurred, and the visual acuity of her right eye decreased to 20/630 with correction. A relative afferent pupillary defect was detected in the right eye. Fundus exam revealed severe optic nerve swelling but no vascular abnormalities. Visual evoked potentials were significantly reduced in the right eye. Orbit magnetic resonance imaging (MRI) revealed an ONG on her right optic nerve extending from the optic canal to the disc (Fig. 1A). She underwent a craniotomy and complete tumor removal. The histologic findings were compatible with pilocytic astrocytoma (World Health Organization grade I). Postoperative MRI showed marked regression of the tumor along the optic nerve, although an 8×8×6 mm nodular lesion remained, and enhanced streaky densities were observed in the intraconal space.
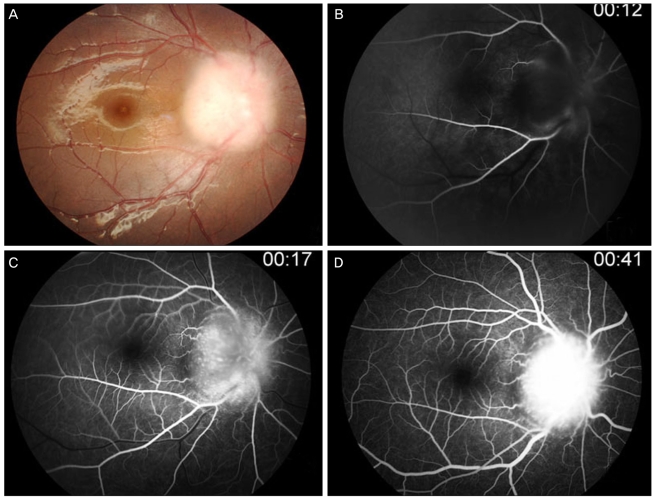
Two years after the surgical removal, tumor extension through the posterior wall of the right orbital groove was found on MRI (Fig. 1B). The fundus showed severe optic nerve swelling, but no vascular changes were observed (Fig. 2).
She underwent stereotactic image-guided robotic radiosurgery using the CyberKnife for the recurrent lesion. This was treated with 16 Gy in total, divided among four doses. Following the stereotactic radiosurgery, the intraglobular enhancing mass regressed completely. However the retroglobular enhancing nodule was reduced in size, but not totally resolved (Fig. 1C).
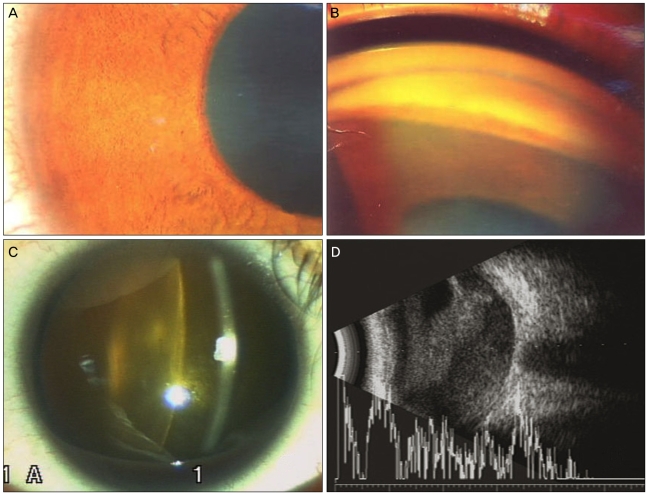
Eight months after the stereotactic radiosurgery, she was referred to our glaucoma clinic for uncontrolled IOP reaching 80 mmHg and ocular pain that had developed 3 days earlier. Her visual acuity was no light perception in the right eye and 20/20 in the left eye. The intraocular pressure was 34 mmHg with glaucoma medications. Slit lamp examination revealed rubeosis iridis, nucleosclerosis, and vitreous hemorrhage (Fig. 3). Follow-up MRI showed no tumor progression. With maximum medical treatment, the IOP was decreased to 34 mmHg without pain.
Discussion
Neovascular glaucoma is a rare complication of ONG with only two reported cases. The first case demonstrated NVG following vascular occlusive or ischemic change originating from small gliomas [3,4]. The second case resulted from a mass effect sufficient to induce both proptosis and vascular occlusion [5]. However, in our case, NVG developed after successful reduction of the tumor size with stereotactic radiosurgery.
The pathogenesis of NVG associated with ONGs is not fully understood. Compression by the periorbital mass in the limited intraorbital space and retinal invasion by the tumor can result in retinal vascular occlusion or ischemia and the release of angiogenic factors. Complications after surgery or irradiation can also give rise to NVG. In our case, the mass was reduced in size following stereotactic radiosurgery. Therefore, it was unlikely that a mass effect caused the vasculopathy. Although many possibilities exist, the most likely causative factor is a radiation effect. The formation of a cataract supports this possibility.
Most ONGs are benign astrocytomas with a prediction for expansive versus infiltrative growth. Therefore, radical removal is the treatment of choice, especially for intraorbital ONGs. Radiotherapy or chemotherapy is recommended when progression occurs after surgical removal [6]. Currently, however, stereotactic radiosurgery is used more frequently to avoid surgical complications. Although several reports have presented NVG as a complication after stereotactic radiosurgery for intraocular tumors [5], no report has described NVG after stereotactic radiosurgery for an ONG.
We suggest that ONGs be irradiated very selectively and followed carefully for unwanted complications such as NVG, even after a successful reduction in tumor size.



 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print






