Familial retinal arterial tortuosity (fRAT) is characterized by marked tortuosity of the second- and third-order retinal arterioles with normal first-order arterioles and normal venules. In most cases, systemic involvement of non-ocular vascular beds has not been demonstrated.1 However, in a few cases, other associated vascular anomalies have been reported, including malformations in the Kieselbach nasal septum, spinal cord vascular mass,2 and telangiectasis of bulbar conjunctiva.3 We present here a case of fRAT associated with an internal carotid artery aneurysm. To our knowledge, the present paper is the first such report.
Case report
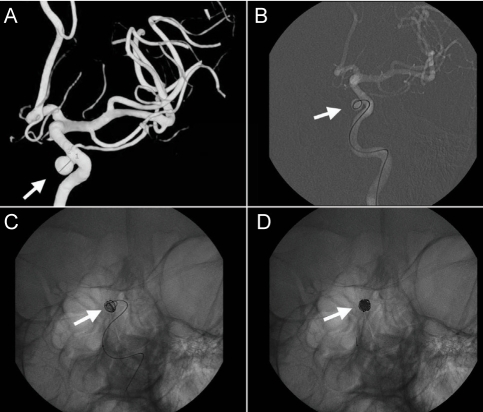
A 44-year-old woman presented with blurred vision in the left eye for 1 week. Best-corrected visual acuity was 20/20 in the right eye and 20/25 in the left eye. Ophthalmologic examination revealed marked tortuosity of the second- and third-order retinal arterioles in both eyes as well as retinal and preretinal hemorrhages near the fovea of the left eye (Fig. 1A, B). She had normal blood pressure, and normal blood glucose. She denied other past medical history and medications. In the course of observation, the preretinal hemorrhage spontaneously resolved without complication. Six months later, she returned with decreased visual acuity in the right eye. Best-corrected visual acuity was 20/50 in the right eye and 20/20 in the left eye. Fundus examination showed new retinal hemorrhages in the right macula (Fig. 1C, D). Since she complained of headache, computed tomography (CT) was performed, with and without contrast, in order to evaluate for intracranial hemorrhage or cerebrovascular disease. A left internal carotid aneurysm was detected on CT angiography (Fig. 2A). Coiling of the aneurysm was performed by transfemoral cerebral angiography (TFCA) (Fig. 2B-D). No other intracranial vascular lesion was found. After 1 month, the retinal hemorrhages resolved, and visual acuity returned to 20/20 in both eyes.
Discussion
Patients with fRAT suffer variable degrees of transient vision loss owing to retinal hemorrhages after minor stress or trauma.2 The prognosis is usually excellent. Although fRAT is generally considered to be an isolated retinal finding, a few cases with associated systemic vascular anomalies have been reported.2 More recently, a study of nailfold capillaroscopy in patients with fRAT revealed significant tortuosity of the capillaries in all fingers of the patients examined.4 Such evidence suggests that the vascular malformation may not be limited to the retina. We present a case of internal carotid aneurysm associated with a pattern of retinal arteriolar tortuosity pathognomic for fRAT, suggesting possible involvement of the cerebral circulation. Although cerebral arteriolar tortuosity was not demonstrated on TFCA or CT angiography, the resolution of these techniques is not sufficiently high to detect second- or third-order arterioles.
Occurrence of a carotid aneurysm was rare and incidence of the carotid aneurysm was reported from 0.1% to 4% of all peripheral arterial aneurysm.5 Also, fRAT is a rare disorder, and only approximately 100 cases have been published literature.3 Furthermore, the presented case patient did not have such etiology of aneurysm as atherosclerosis, hypertension, trauma, infection, and arteritis.5 These findings could suggest possible association of aneurysm and fRAT. Also the aneurysm might be a coincidental finding in a fRAT patient, especially since aneurysms are not usually seen in the retina with this condition and the ICA is a large arteriole and not 2nd or 3rd order branch.




 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print






