 |
 |
| Korean J Ophthalmol > Volume 22(1); 2008 > Article |
Abstract
Purpose
To report a case of bilateral ophthalmic artery occlusion in rhino-orbito-cerebral mucormycosis.
Results
An 89-year-old man with poorly controlled diabetes developed sudden bilateral ptosis, complete ophthalmoplegia of the right eye, and superior rectus palsy of the left eye. Brain and orbit magnetic resonance imaging showed midbrain infarction and mild diffuse sinusitis. On the 2nd day of hospitalization, sudden visual loss and light reflex loss developed. There were retinal whitening, absence of retinal arterial filling, and a total lack of choroidal perfusion on fluorescein angiography of the right eye. The left eye showed a cherry red spot in the retina and the absence of retinal arterial filling and partial choroidal perfusion on fluorescein angiography. On rhinologic examination, mucormyosis was noticed. Despite treatment, visual acuity and light reflex did not recover and he died 4 days after admission.
Rhino-orbito-cerebral mucormycosis (ROCM) is a fatal fulminant opportunistic infection leading to death in some cases, which mostly occurs among patients with a weakened immune system. This case involved bilateral ophthalmic artery occlusion with third nuclear, as well as fourth and sixth cranial nerve palsies of the right eye, which is a rare initial presentation of mucormycosis.
An 89-year-old man presented with sudden onset of bilateral ptosis on November 2, 2005. He had a one week history of xerostomia. Three days prior to hospitalization, the patient was diagnosed with diabetes mellitus and had a history of surgery for gastric cancer, which occurred four years ago. His fasting glucose level and postprandial (2 hr-after-meal) glucose level were 196 mg/dL and 300 mg/dL, respectively.
His visual acuity was 20/100 in both eyes. The right pupil was mid-dilated and had no light reflex. Complete ophthlamoplegia of the right eye and superior rectus palsy of the left eye were observed. Bilateral ptosis, mild proptosis, and periorbital puffiness were also observed. His anterior segment examination was notable for moderate nuclear sclerotic cataracts and mild chemosis, while fundoscopic examination revealed no specific abnormal finding.
Brain and orbit magnetic resonance imaging (MRI) revealed no specific abnormal findings in the cavernous sinus and orbit, except bilateral midbrain infarction and mild diffuse sinusitis (Fig. 1). Based on the brain MRI finding, the bilateral ptosis and superior rectus palsy of the left eye were regarded to be caused by 3rd nuclear palsy. The results of CSF analysis showed that white blood cell count and protein were elevated and intravenous antibiotics were given for a central nervous system infection.
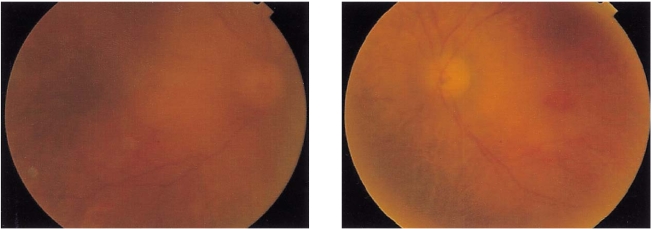
On November 3, 2005, the visual acuity of both eyes decreased to perception of hand motion and bilateral complete ophthlamoplegia developed (Fig. 2). Anterior segment examination revealed no specific change compared with the previous finding. Fundoscopic examination revealed that the optic disc was pale and the posterior pole was generally edematous in both eyes. A cherry-red spot was found in the left eye (Fig. 3). Fluorescein angiography (FAG) demonstrated that retinal vessels were not imaged, even 10 minutes after injecting the dye.
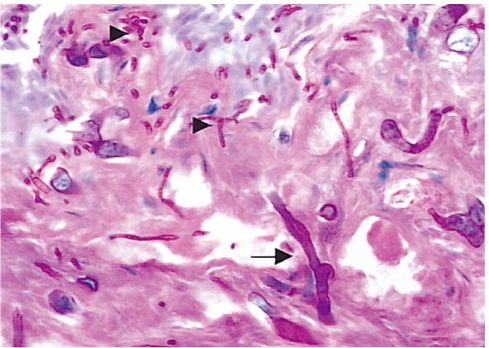
Choroidal perfusion was not found in the right eye and partial choroidal fluorescence was observed in the left eye (Fig. 4). Thus, he was diagnosed with simultaneous bilateral ophthalmic artery occlusions. On the same day, rhinologic examination revealed a destructed nasal septum, black necrotic lump in the nasal cavity and an ulcer on the hard palate, which was confirmed as murcomycosis upon biopsy (Fig. 5).
Based on the clinical findings and biopsy result, ROCM was diagnosed and Amphotericin B (50 mg/day) was intravenously administered. Although extensive local excision was required, the patient and his guardian rejected to have surgery. On November 6, 2005, the patient died.
Typical ROCM initially involves general weakness, headache in the occipital area, fever and bloody rhinorrhea. Subsequently, facial and/or orbital cellulitis, ptosis, and ophthlamoplegia occur.1 In this case, 3rd nuclear palsy, 4th, and 6th cranial nerve palsies of the right eye initially developed and subsequently, ophthalmolplegia of the left eye and bilateral ophthalmic artery occlusions followed.
Ferry et al.2 reported 16 patients with rhino-orbito-cerebral mucormycosis. In their report, rhinologic symptoms were mostly common initial symptoms (11 cases), while ocular pain and facial cellulitis were observed in 6 and 5 cases, respectively. This patient did not complain of rhinologic symptoms, although rhinologic examination revealed a black eschar in the nasal cavity.
Absence of a cherry red spot in the retina and FAG finding of the right eye are consistent with concomitant choroidal and retinal ischemia. Although a cherry red spot in the retina was present in the left eye, retinal arterial imaging was not found, and partial choroidal perfusion was observed. The lack of sign of anterior segment ischemia can be explained by incomplete ophthalmic arterial occlusion. Also, the 3rd cranial nerve palsy of the right eye may have been caused by orbital ischemia, infarction of the midbrain, or both. In this case, the brain MRI revealed no specific abnormal findings in the cavernous sinus and orbit, except bilateral midbrain infarction. It suggested that midbrain infarction caused the ophthalmoplegia; however, ocular ischemia secondary to invasion of the orbital artery cannot be excluded as the cause of ophthalmoplegia. The mechanism of orbital ischemia is that the hyphae have a marked tendency to invade and thrombose arteries.3,4 In this case, the orbital apex was not involved according to radiologic examination. Direct vascular invasion most likely caused ophthalmic ischemia and ophthalmoplegia. A case of unilateral orbital infarction syndrome associated with rhino-orbito-cerebral mucormycosis has been reported in Korea.5 When the eye is infected, the choroids usually exhibit the greatest number of organisms, the fungi having entered the globe via the ciliary arteries.3,4
As is the case with acute central retinal artery obstruction, retinal opacification is also present with acute ophthalmic artery obstruction. However, the latter it is usually more pronounced, both in the severity and the extent of the area involved. The presence of a cherry red spot with an acute ophthalmic artery obstruction is variable. With an ophthalmic artery obstruction, the presence or absence of a cherry red spot is probably determined by the degree of choroidal hypoperfusion, the rapidity of onset of vascular compromise, and the duration of the insult.
The most common causes of ophthalmic artery and/or central retinal artery occlusion are embolization from ulcerated plaques of the carotid artery and atherosclerotic occlusion of the internal carotid artery. However, it is extremely rare for either one of these etiologies to cause bilateral visual loss. Brown et al.6 reported a case of acute simultaneous bilateral obstruction of central retinal and posterior choroidal circulations in atrial fibrillation and typhoid fever. A case of virtually simultaneous bilateral ophthalmic artery occlusions was reported in a patient with acquired immunodeficiency syndrome and central nervous system lymphoma. In ROCM, visual loss usually has been attributed to ophthalmic artery and/or central retinal artery occlusions; however, most previous reports covered unilateral or sequential ophthalmic artery and/or central retinal artery occlusions.
Physicians should be alerted to rhino-orbito-cerebral mucormycosis in patients who present with ocular abnormalities, including orbital cellulitis, ptosis, and ophthlamoplegia, and have diabetes mellitus or a weak immune system. A high index of suspicion is very important for the early diagnosis of this very progressive disease. Our case illustrates that patients with rhino-orbito-cerebral mucormycosis can have bilateral ophthalmic artery occlusion and loss of vision within a few days.
Notes
Presented at the 95th Meeting of the Korean Ophthalmological Society, Pusan, Korea, April 14, 2006.
REFERENCES
1. Vessely VB, Zitsch RP 3r, Estrem SA, Renner G. Atypical presentations of mucormycosis in the head and neck. Otolaryngol Head Neck Surg 1996;115:573-577.


2. Ferry AP, Abedi S. Diagnosis and management of rhino-orbitocerebral mucormycosis. Ophthalmology 1983;90:1096-1104.


3. Onerci M, Gursel B, Hosal S. Rhinocerebral mucormycosis with extention to the cavernous sinus. Rhinology 1991;29:321-324.

4. Bendet E, Talmi YP, Kronenberg J. Rhino-orbito-cerebral mucormycosis. Otolaryngol Head Neck Surg 1996;114:830-832.


Fig.┬Ā1
Brain and orbit magnetic resonance imaging (A. T2 weighted image, B. pre-enhanced T1 weighted image, C. gadolinium-enhanced T1 image) revealed no specific abnormal findings in the orbit, except mild diffuse sinusitis.
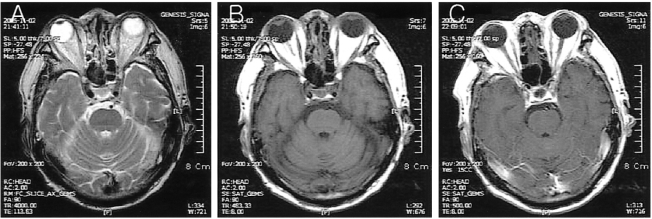
Fig.┬Ā2
On the day after initial presentation, his visual acuity of both eyes decreased to perception of hand motion and bilateral complete ophthlamoplegia developed. Arrows represent direction of ocular movement.
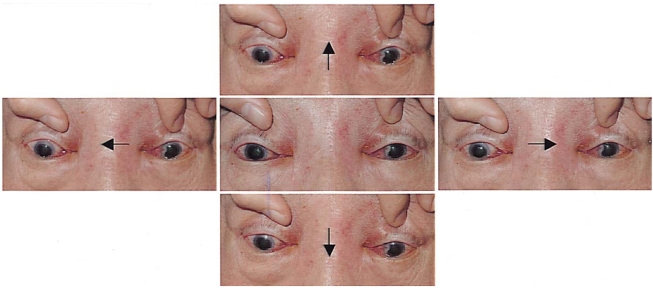
Fig.┬Ā3
Fundus photographs on the day after initial presentation: (Left) Right eye (Right) left eye, Both eyes show retinal whitening and optic disc edema, the left eye shows a cherry-red spot.
- TOOLS
-
METRICS

- Related articles
-
Branch Retinal Artery Occlusion in Patient with COVID-19: Case Report2021 December;35(6)
Central Retinal Arterial Occlusion in Granulomatosis with Polyangiitis2018 December;32(6)
Central Retinal Artery Occlusion by Left Atrial Myxoma2017 February;31(1)
Bilateral Lateral Rectus Resection in Patients with Residual Esotropia.2004 December;18(2)




 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print



