A Case of Cataract Surgery without Pupillary Device in the Eye with Iridoschisis
Article information
Abstract
Purpose
To introduce a case of iridoschisis patient who underwent cataract surgery successfully without pupil device.
Methods
A 64-year-old female who showed iridoschisis of her both eyes underwent cataract operation at her right eye without a pupillary device. The preoperative and postoperative ophthalmologic examinations including visual acuity, intraocular pressure, reaction of anterior chamber, and degree of damage on iris was evaluated respectively.
Results
Cataract surgery was performed under topical anesthesia through a clear corneal incision. Iris fibrils were held in place by ophthalmic viscosurgical device (OVD, sodium hyaluronate 3%-sodium chondroitin sulfate 4%, Viscoat®) that was injected into the anterior chamber. A small capsulorrhexis was made and the nucleus was delivered with low-power phacoemulsification, most of which was performed under the anterior capsule. The iris came into contact with the OVDs only and received no mechanical trauma. There were no intraoperative complications such as tear of the iris, hyphema, loss of mydriasis, or rupture of the posterior lens capsule. The edema of corneal stroma and inflammation of anterior chamber was shown at immediate-postoperative period, but completely subsided 2 weeks later. The visual acuity showed improvement from 20/400 to 20/30.
Conclusions
In iridoschisis patients, there is a risk of aspiration of iris fibers during cataract surgery. With adequate use of OVD and careful modulation of surgical devices, cataract surgery was successfully performed without using extra pupil-supporting device.
Iridoschisis is a rare disease with only few cases reported.1 Most of the patients are over 65 years old and the condition is usually bilateral. The etiopathogenesis is not clearly understood but has most commonly been considered as an age-related atrophy.2 This condition has been associated with glaucoma, ocular trauma or idiopathic atrophy of the iris stroma.3-6 Since Schmitt7 first reported iris splitting into 2 layers in 1922, there have been intermittent reports about iridoschisis with syphilitic interstitial keratitis, keratoconus, and most frequently, glaucoma.3-6
Because iridoschisis is associated with aging,6 cataract is often a concomitant issue, especially nuclear sclerotic cataract.8 Because it presents with 2 or more layers of iris tissue that is free-floating in the anterior chamber (AC), cataract operation in these patients needs special care.9 Iris fibrils can be attracted to the phaco tip or the irrigation & aspiration (I&A) needle by the fluidic negative forces.10
For protection of iris, there have been some challenges in cataract operation using various devices such as flexible iris hooks, iris retractors or pupil expanders (Graether pupil expander, Perfect Pupil system).2,9,11 Vinicius et al.12 described a technique in which the affected anterior iris stroma is removed using a vitreocutter just before cataract extraction.
In Korea, there have been no reports since Kim et al.13 reported two cases in 1995, and Kwak et al.14 reported a case associated with angle closure glaucoma in 1996.
We report a case of iridoschisis patient who underwent cataract surgery successfully with conventional surgical technique, and without any additional pupil-saving device as the first case in Korea.
Case Report
A 64-year-old female presented with gradual loss of vision in the right eye (OD) of one year duration. About six months ago, she had undergone intracapsular cataract extraction, anterior vitrectomy, and scleral fixation of intraocular lens (IOL) in the left eye (OS). At that time, she was suspected of iridocorneal endothelial syndrome (ICES).
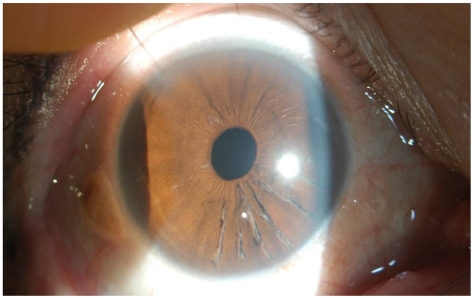
The preoperative best corrected visual acuities (BCVA) were 20/400 OD, 20/30 OS. Intraocular pressures (IOP) in each eye were 15 mmHg by applanation. The Slit lamp biomicroscopy of both eyes (OU) showed clear cornea, deep and clear AC, and the angle was wide open. Both eyes had splitting of the anterior layers of the iris with fibrillar degeneration extending from 3 to 6 o' clock OD, and from 4 to 6 o' clock OS. Additionally, there was diffuse atrophy of iris from 11 to 1 o' clock OS (Fig. 1). The underlying iris pigment epithelium appeared intact with no transillumination defect. The clinical appearance was consistent with iridoschisis OU. The right eye showed nuclear and cortical cataract associated with posterior subcapsular cataract, and the left eye was pseudophakia. Specular microscopy of the OD revealed regular, hexagonal shape of endothelial cells without any abnormalities like bullae or guttae, and the endothelial cell count was 2865 cells/mm2. The rest of the ocular examination was normal.
Pupil dilation is performed using 3 drops of tropicamide 0.5% and phenylephrine hydrochloride 0.5% at 5-minute intervals 1 hour prior to surgery. Intraoperative pupillary diameter was about 5~6 mm. Topical anesthesia was applied using Alcaine® and 3% Lidocaine, and a paracentesis was done at 10 o' clock. A 2.75 mm main clear corneal incision was performed using the keratome blade. A dispersive ophthalmic viscosurgical device (OVD), sodium hyaluronate 3%-sodium chondroitin sulfate 4% (Viscoat®, Alcon) was injected through the clear corneal wound to stabilize the anterior chamber and protect the iris stroma by displacing aqueous from the AC and pushing the iris strands from the pupillary aperture. An anterior continuous curvilinear capsulorhexis not exceeding over the pupillary margin was performed using the 26 G needle and capsular forceps. After hydrodissection and hydrodelineation, careful phacoemulsification was performed (Allergan Sovereign® Phaco System, SOV680330) for nucleus removal with special care not to touch the iris tissue. Aspiration was used to clean residual cortical fibers from the capsular bag. When a loss of the protective effect of viscoelastic material was observed during surgery, Viscoat® was reinjected additionally to inhibit iris fibril movement with the BSS stream.
The maximum limit of the vacuum was 300 mmHg and the aspiration rate, 20 cc/mmHg. The height of the irrigation bottle is maintained less than 60 cm to minimize the turbulence within the chamber. Total US time was 48 seconds with a mean final rate of 10% of potency.
The capsular bag was inflated with viscoelastics, and a single-piece acrylic intraocular lens (Acry-Sof® SA60AT, Alcon) was inserted. The IOL was safely placed in the capsular bag and centered, followed by aspiration of the residual viscoelastics. If there were some movement of iris fibrils, additional viscoelastics was inserted.
Finally, BSS Carbacol (carbachol 0.01%, Miostat®) was used to constrict the pupil.
Postoperatively, the inflammatory response in the AC was moderate, some fibrillar materials were seen. The cornea showed some Descemet folds, and the pupil was round and undamaged (Fig. 2).
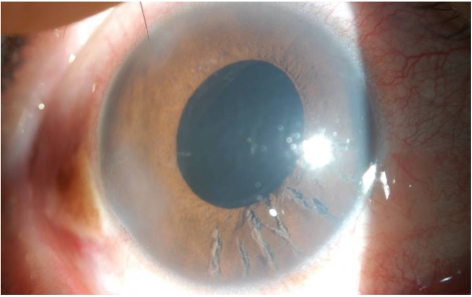
Three days after cataract operation, corneal stromal edema and inflammation of anterior chamber began to decrease.
One week after surgery, the uncorrected visual acuity was 20/100 OD, and improved to 20/30 on the two weeks postoperative day. There were traces of cells in the AC, but no fibrillar materials were seen (Fig. 3).
The patient's last visit was 1 month after surgery when UCVA was 20/40, and BCVA 20/20. The cornea, AC and iris were clear and intact without any inflammatory sequalae.
Discussion
Iridoschisis is a very rare condition resulting in one or more layers of the anterior iris surface. A localized area of iris stroma is cleaved in two with the anterior atrophic portion disintegrating into fibrils. The separated stromal fibers go through a degenerative process in which they detach and free float in the anterior chamber, creating a "shredded wheat" appearance. The condition primarily affects the inferior iris quadrants and rarely superior quadrants.9-13
Glaucoma occurs in 50% of the cases and is of the angle closure type.15 Whether iris changes are responsible or iridoschisis occurs more frequently in eyes that are predisposed to angle closure is unclear.16 While primary angle closure glaucoma has been implicated in iridoschisis formation, the affected fibers may bow forward, leading to anterior synechiae and angle closure glaucoma.5,6,14,15 In the present case, the anterior chamber angle was wide open and the IOP were within normal limits.
It is a matter of concern that the clinicians are prone to misdiagnose this condition, especially in the case with dark colored iris. It may be related to relatively low incidence in Asian race. In Korea, there have been only three cases of report in 1990's.13,14 Differential diagnosis must include Axenfeld-Reiger anomaly, ICES, or other conditions which accompany the degenerative change of iris stroma.
An abnormal corneal endothelium that migrates across the chamber angle on to the surface of the iris is the common feature of the ICE syndromes.17 The iris in ICES is usually atrophic rather than split, and peripheral anterior synechiae (PAS) extends to Schwalbe's line. The pupil may be ectopic and displaced towards PAS. Specular microscopy has shown the abnormal corneal endothelial cells, so called "ICE cells", which are pleomorphic and resemble corneal guttata. It occurs mostly unilateral and the clinical symptoms are presented earlier than iridoschisis (about 3rd or 4th decades). Axenfeld-Rieger syndrome is a rare congenital anomaly which is presented at birth. There is hypoplasia of the iris stroma with filaments connected to abnormal peripheral cornea.18 In this case, the clinical features most coincidence with iridoschisis, rather than ICES or Axenfeld-Reiger syndrome. The onset of symptom was over 60 years of age. The condition was bilateral and there was no PAS or connection of iris fibrils with peripheral cornea. Specular microscopy showed normal shape and count of corneal endothelial cells. Considering that our patient had been diagnosed as bilateral ICES before, there may have been other misdiagnosed and unreported cases.
Because iridoschisis is associated with aging, cataract is often a concomitant issue.2 The disorganized anterior layer of the iris and fibrillar material in the pupillary axis has a tendency to become drawn in by the suction of the I/A cannula and phaco tip during phacoemulsification. Pupil dilation in these patients is also poor because this condition may be associated with pseudoexfoliation syndrome or atrophy of the pupillary margin.11
If the loose iris fibrils become drawn and entrapped in the aspiration port, there is a strong chance of complications like bleeding, iris tears, loss of mydriasis, and disruption of the blood-aqueous barrier.9 Many methods have been tried to stabilize the iris fibers during cataract operation in the presence of iridoschisis. Most of them are based on mechanical restraint of the disorganized iris using flexible iris hooks, iris retractors or pupil expanders, such as multiple iris hooks or Graether pupil expander.2,9,11,12
These mechanical supports provide additional pupillary dilation, stabilize the capsule, and trap some of the fibers at pupillary margin during phacoemulsification. But these supportive devices can also induce strain and trauma to iris tissue resulting in increased inflammation after postoperative period. Sometimes they lead to defects in the pupillary margin or to an atonic pupil.11 Moreover, long, free-floating, torn fibers may not be trapped and may still extend over the rim into the surgical field.9 In withdrawing these instruments, iris fibers can be trapped in the stab incisions, and such fibers may act as an entrance for epithelial cells and micro-organisms.9
In this case, without mechanical restraint of iris, we minimized the iris trauma through the right choice of the viscoelastic material, careful manipulation of phaco tip or I&A cannula, and reducing the turbulence by using the minimum required fluidic parameters achieved with lowering the total phaco power and the height of the irrigation bottle. The Allergan Sovereign® Phaco System has a peristaltic fluidic pump system with vacuum range of 0~500 mmHg and flow range of 0~40 cc/min. The maximal fluidic parameters showed in the presented case were relatively lower than the values that had been usually set for conventional cataract surgery. The detail values are shown in Table 1.
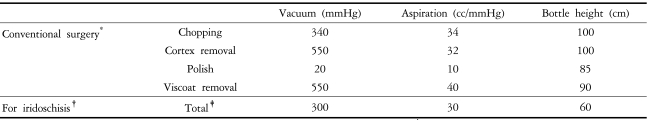
The maximum limits of fluidic parameters set in cataract surgery with Allergan Sovereign® Phaco System
As an OVD, sodium hyaluronate 3%-sodium chondroitin sulfate 4% (Viscoat®) was chosen. Viscoat® has been known to have a very high dynamic viscosity at high shear rate. This property and a poor cohesion provide a better corneal endothelial protection during in vitro phacoemulsification. 19,20 Although the removal time of OVD is longer with dispersive Viscoat® than other cohesive OVDs (sodium hyaluronate 1.4%, Healon GV®, or sodium hyaluronate 1.0%, Provisc®),21 Viscoat® is less influenced by turbulent flow while cohesive OVDs tend to be washed out suddenly which could result in sudden collapse of anterior chamber.21,22 Furthermore, the cohesive OVD fragment behind the IOL is exposed to too little turbulent flow to move towards the aspiration port unless the I&A tip is placed behind the IOL or a special technique is used.23
A small capsulorhexis that did not extend vertically beyond the middle of the pupil was performed deliberately to allow he anterior capsule to act as an additional barrier between the iris and instruments.
To protect the friable and disorganized iris from further damage, the instruments were manipulated only in the pupillary center. If a loss of the protective effect or the movement of iris fibril were observed, the OVD was injected additionally.
The machine settings, including flow rate and vacuum limit, as well as port diameter are different between phacoemulsification needle and I/A tip. The former is related to the retention ability of OVDs and the latter to removal property.23 Although we were not able to manage the diameter of phaco or I&A tips, the minimum possible amount of US energy, BSS flow rate and vacuum limit enabled the surgical procedures to be performed under safer environment.
There was no iris trauma, intraoperative iris bleeding, or posterior capsular rupture during surgery. The corneal edema had disappeared by two weeks after surgery, and the AC inflammation had subsided after one month postoperatively. The final BCVA OD had improved from the preoperative one, from 20/400 to 20/20.
This is a case which emphasizes the importance of exact preoperative diagnosis and differential diagnosis in iridoschisis. In the absence of proper clinical impression and proper preoperative preparation, surgeons may not have been able to manage the various intraoperative complications. Our patient had been diagnosed as ICES, and underwent ICCE, anterior vitrectomy and scleral fixation of IOL on the contralateral eye (OS).
In conclusion, for iridoschisis is a very rare condition and easy to be confused with other diseases, one must consider this condition into differential diagnosis if the iris abnormalities are suspicious.
Notes
This paper has been presented in the 97th Korean Ophthalmological Society Conference (in poster)