A Case of Epithelial Inclusion Cyst of Iris
Article information
Abstract
To report on an epithelial inclusion cyst of the iris that was successfully treated with needle aspiration and Ab externo laser photocoagulation. A 6-year-old boy was treated for a 6.0 mm fluid-filled cyst in the anterior chamber of the right eye. Thirteen months previously, he had undergone primary closure of a 6 mm full-thickness corneal laceration. The subsequent cyst was diagnosed as an epithelial inclusion cyst of the iris. His vision decreased to finger-count at 30 cm as the cyst grew over the pupil. We performed needle aspiration of the cyst and Ab externo laser photocoagulation of the cyst wall. The treated lesion was completely removed. The patient's visual acuity recovered to 20/40 without complications. There was no recurrence as determined by slit lamp examination up to 6 months after treatment. Needle aspiration and Ab externo laser photocoagulation can be used to effectively treat epithelial inclusion cysts of the iris.
Epithelial inclusion cysts occur secondary to penetrating ocular injuries1 and incisional ocular surgery.2,3 Various surgical procedures including cataract surgery, penetrating keratoplasty, radial keratotomy, and glaucoma surgery may predispose a patient to the formation of epithelial inclusion cysts.4
When epithelial cells are implanted into the anterior chamber of the eye, most will form sheet-like ingrowths that spread across the ocular structures. However, a cyst-like pattern may also occur if an intraocular nest of implanted or congenital cells grows centripetally.5 Small cysts that are stable in size and otherwise asymptomatic may be present, often for years.5 If the cyst enlarges, however, it may require surgical treatment because it may obstruct the visual axis and incite further complications such as uveitis, corneal edema, or glaucoma.6,7
Numerous reports have reported treatments for epithelial cysts. Aspiration and injection of sclerosing agents, electrolysis, endodiathermy, and en bloc excision have been used; however, these procedures are largely unsuccessful with a high rate of recurrence.2,4,5 Recently, laser photocoagulation was used as an alternative, less invasive treatment for epithelial cysts with fewer compilcations.8 Nevertheless, this technique has several limitations including possible recurrences, anterior cyst wall visualization, risk of rupturing the cyst wall, and conversion of the cyst into a diffuse sheet with epithelial ingrowth.5
Here, we report a case of an epithelial inclusion cyst of the iris that was successfully treated with aspiration and Ab externo laser photocoagulation.
Case Report
A 6-year-old boy was referred to our clinic for 6 mm full-thickness corneal laceration after trauma from a boomerang to his right eye. Past ocular and medical histories were unremarkable, and the patient was otherwise in good health. On examination, the best-corrected visual acuities were 20/20 in his left eye and finger-count at 10 cm in his right eye. Intraocular pressure was not assessed in either eye. Upon anterior segment examination of the right eye, we observed a 6 mm full-thickness corneal laceration. This laceration involved 1 mm of the sclera with a prolapsed iris and incarceration extending horizontally from the center to the nasal side of the limbus area. The anterior chamber was shallow. A blood clot had precipitated in half of the inferior part of the anterior chamber, and red blood cells and a fibrotic membrane was also dispersed in the anterior chamber. An anterior segment examination was unremarkable in the patient's left eye. The lens and fundus were invisible in the right eye, and unremarkable in the left eye.
The patient underwent a primary closure of the cornea and was treated with oral Augmentin syrup at 40 ml/day (400 mg), Bendazac lysine (Bendaline®) at 750 mg/day, and 0.3% tobramycine and 0.1% fluorometholone (Ocumetholone®) eyedrops every 6 hours. He was followed-up every week, and 1 month postoperatively the wound was well approximated and the best-corrected visual acuity was 20/20 in his left eye and 20/40 in his right eye. There were no anterior chamber reactions in the right eye.
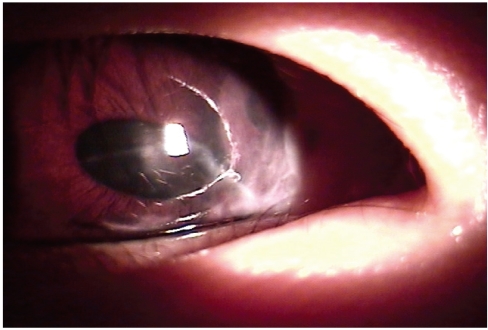
Thirteen months later, slit lamp examination revealed a fluid-filled cyst adjacent to the previously approximated corneal wound (Fig. 1). The cyst was diagnosed as an epithelial inclusion cyst of the iris. There was no dehiscence of the corneal wound. The best-corrected visual acuity was 20/20 in the left eye and finger count at 30 cm in the right eye because the inclusion cyst grew over the pupil and covered the visual axis.

Preoperative anterior segment photograph in an operative microscopic field of an inclusion cyst at POD 13 months after primary corneal closure. This photograph shows a linear corneal scar and a 6.0 mm fluid-filled epithelial inclusion cyst which occluded the pupil.
White arrow=margin of epithelial inclusion cyst;
Yellow arrow=previous corneal laceration scar.
The patient was treated with a 27-Gauge needle aspiration of the cyst at the nasal side of corneal limbus (Fig. 2A) after making a side puncture at the temporal side of the cornea limbus. Viscodissection of the cyst separated the cyst from the corneal endothelium. Then, laser photocoagulation was performed with an endolaser (Ultima 2000SE, Coherent. Inc., USA) at 200 mW and a total of 40 pulses in the epithelial wall with an endolaser probe (curved maximum focused endo ocular laser probe 55.29L, Synergetics Inc., USA) from the external cornea (Fig. 2B). We aspirated 0.04 ml, and cell cytology showed amorphous fluid with no cells. After needle aspiration and laser photocoagulation, an anterior segment photograph showed shrinkage of the cyst (Fig. 3). Upon examination 10 days after treatment, the cornea was relatively clear and the anterior chamber was deep and clear. The best-corrected visual acuity was 20/20 in the left eye and 20/100 in the right eye. The patient's right eye was medicated with 0.3% tobramycine and 0.1% fluorometholone (Ocumetholone®) eye drops every 6 hours.
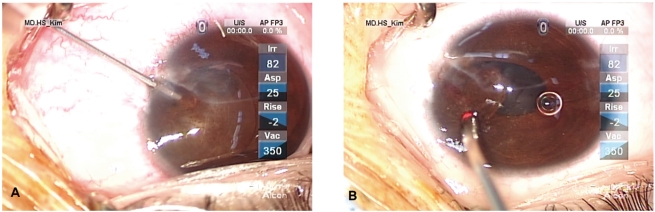
Operative microscopic fields showing needle aspiration of a fluid-filled cyst (A) and Ab externo photocoagulation with an endolaser probe (B).
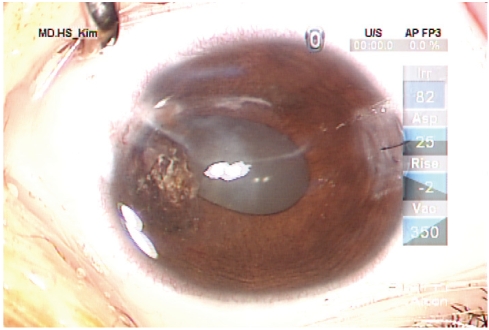
Postoperative anterior segment photograph after needle aspiration and Ab externo laser photocoagulation treatment showing shrinkage of the large cyst.
On examination 1 month after needle aspiration and laser photocoagulation, the best-corrected visual acuities were 20/40, -4.00 sph -5.00 cyl 130 Ax in the right eye and 20/20, plano in the left eye. The cornea showed oblique corneal opacity in the center to the nasal side of limbus, and iridocorneal adhesion was seen in the nasal side of the iris which was the site of laser ablation. Otherwise, the lens and fundus examinations were normal.
At the 6-month follow-up visit, the best-corrected visual acuity of the right eye was 20/40 with an intraocular pressure of 12 mm Hg. There was no evidence of recurrence of the epithelial cyst (Fig. 4).
Discussion
Iris cysts are divided into primary and secondary iris cysts. A primary iris cyst is an epithelial-lined space which involves a portion of the iris and has no recognizable etiology.9 A primary iris cyst can be further classified according to its histological origin, that is, one that is derived from the epithelium of the iris and the ciliary body and another that is derived from the iris stroma.9-12 A secondary iris cyst is an epithelial-lined space that involves a portion of the iris and has a recognizable etiology, such as surgical or nonsurgical trauma, drugs, secondary to an intraocular tumor, or parasites.9
The two types of cysts have different clinical courses. Primary iris cysts maintain their original state without an increase in size or complications, while secondary iris cysts may increase in size and may be accompanied by severe complications such as inflammation or glaucoma.
Among secondary cysts, epithelial inclusion cysts result from penetrating ocular injury or surgical inclusion of corneal or conjunctival epithelium on the cornea or iris stroma.8 The iris vasculature provides a favorable environment for cellular proliferation in the eye.7
Although an epithelial inclusion cyst may remain unchanged for years or may even regress spontaneously, the usual course is a steady increase in size with devastating consequences such as uveitis, glaucoma, corneal damage, cataract formation, and obstruction of vision.6 The management of epithelial inclusion cysts is usually simple observation if the lesion is small and asymptomatic, but complete removal of the cyst is occasionally required to prevent or to treat serious problems such as pupillary obstruction, secondary glaucoma, iridocyclitis, corneal decompensation, loss of vision, and intractable pain.5
Here, a clinical diagnosis of epithelial inclusion cyst of the iris was made due to its orgin in the iris, the presence of a clear space between the cyst and the corneal endothelium, and the presence of iris pigment and vessels overlying the cyst's surface upon slit lamp evaluation.4
The epithelial inclusion cyst was detected 13 months after closure of the primary injury. The site of the cyst was in the vicinity of and just below the previous wound, substantiating the above definition. There was no pupillary obstruction, secondary glaucoma, iridocyclitis, corneal decompensation, nor pain. However, we documented an increase in size and proximity of the corneal endothelium as well as encroachment of the cyst toward the pupillary margin. Covering the pupil and obstructing the visual axis were the indications for therapy in this patient. Given the age of our patient, we took the conservative surgical approach of needle aspiration combined with endolaser photocoagulation therapy to optimize vision despite the threat of amblyopia. During the operation, a 27-Gauge needle was inserted into the cyst and its contents were aspirated. Needle aspiration of the cystic fluid, in contrast to laser-induced cyst dissolution, is believed to reduce recurrence rates by preventing the dispersion of cystic fluid in the eye. After making a side puncture, the cyst wall was viscodissected from the cornea and other structures. An endolaser probe was then directed at the residual cyst wall, and the collapsed capsule was removed from the external cornea with photocoagulation. Initially, we used the photocoagulation techniques described by Haller et al.5 but ablation of the cyst was difficult due to possible danger to the surrounding tissue and corneal endothelium. Therefore, we applied photocoagulation from the external cornea. This resulted in better coagulation, most likely because Ab externo photocoagulation with an endolaser probe is on the perpendicular axis of the tissue receiving the laser and a greater amount of laser energy can be absorbed if the proper distance is maintained. This procedure may decrease the risk of corneal endothelial damage. Photocoagulation of the cyst ensures complete destruction of the epithelial cells in the cyst, thus the treated area appears atrophic with contraction of the iris.
The only sequela was the formation of posterior synechiae in the treated area. The preoperative visual acuity of this patient was maintained without any signs of cyst recurrence for 6 months. Based on our experience, we believe that needle aspiration and Ab externo laser photocoagulation can result in a satisfactory outcome without resorting to more extensive and invasive surgery.
There are many treatment modalities for an inclusion cyst of the iris and anterior chamber.2,5,13,14 Surgical excision may be unsuccessful and may have a high rate of recurrence and complications including conversion of the cyst into a diffuse, sheet-like epithelial ingrowth.15 Incomplete excision can lead to the recurrence of the cyst which could necessitate block excision with tectonic corneoscleral grafting.16 However, laser photocoagulation has also been used to ablate these cysts.5,17-19 In a previous study, argon laser photocoagulation treatment of an iris cyst was successful,5,20,21 but laser photocoagulation may not be a satisfactory therapeutic modality for very large iris cysts close to corneal endothelium.20
Needle aspiration combined with Ab externo endolaser photocoagulation therapy should prove helpful in several instances, such as difficulties visualizing the anterior cyst wall, a large cyst contacting the corneal endothelium, and a risk of cyst rupture during photocoagulation. In this procedure, needle aspiration and viscodissection reduce the size of the cyst which enables clear visualization of the anterior cyst wall and decreases the risk of corneal injury during photocoagulation. Reduced cystic fluid volume decreases the probability of laser-induced cystic fluid dissolution. In this way, we successfully eradicated a large epithelial inclusion cyst.
This procedure has advantages in cases of recurrences as repeated procedures can be done without worsening the progression. Conservative surgical approaches are especially helpful in children's eyes, for they tend to have better visual outcomes. The postoperative complications of these procedures were mild uveitis and immediate post surgical pain, which responded well to pharmacological treatment. The only sequela was posterior synechiae, though this did not result in any other secondary complication. Long-term follow-up is recommended due to possible recurrence resulting from the dissolution of a small amount of cystic fluid remaining after needle aspiration. There is also a remote possibility of developing a cataract in the treated eye.
In summary, a cystic lesion was completely removed using the combined techniques of needle aspiration and Ab externo laser photocoagulation. The patient's best-corrected visual acuity recovered without complication. Therefore, the combination of these two techniques may be used to effectively treat epithelial inclusion cysts of the iris.
Notes
This study was presented in part at the Korean Ophthalmological Society, Meeting, Seoul, Korea, October, 2007.