OCT-guided Hyaloid Release for Vitreomacular Traction Syndrome
Article information
Abstract
Purpose
To evaluate the usefulness of OCT retinal mapping in determining the configuration of a vitreomacular adhesion and selecting a meridian for entry into the subhyaloid space in patients with vitreomacular traction syndrome.
Methods
Six consecutive patients (6 eyes) with vitreomacular traction syndrome underwent vitrectomy with peeling of posterior hyaloid. Ocular coherence tomography (OCT) retinal mapping was performed preoperatively. Access to the subhyaloid space was made by creating an opening with a 25 gauge needle at a location where the detached posterior hyaloid membrane was farthest from the retinal surface. The location was selected based on six preoperative meridional OCT scans. The posterior hyaloid was then gently peeled off in a circular fashion around the fovea with a micropick. Visual acuity and foveal thicknesses were measured before the operation and 3 months afterwards.
Results
After the operation, visual acuity improved and central macular thicknesses were reduced significantly in all six patients. The best corrected visual acuity improved from 0.4 to 0.75 with a mean increase by 3.5 lines on a Snellen chart 3 months after the operation. The mean foveal thickness was reduced from 406 µm to 241 µm. The restoration of foveal pit was observed in five patients. Neither intraoperative nor postoperative complications were observed during the follow up period.
Conclusions
An OCT retinal mapping program is a valuable diagnostic tool in understanding the configuration of vitreomacular adhesion and planning the surgical approach for operating on vitreomacular traction syndrome.
Vitreomacular traction syndrome is a complication of a partial posterior vitreous detachment that causes vitreous traction on the posterior retina. In the classic form of the disorder, the vitreous cortex is separated peripheral to the zone where the cortical vitreous remains attached to the retina at the macula and the optic nerve head.1-5 This exerts persistent anteroposterior traction on macula, leading to cystoid macular edema, tranctional macular detachment, and impaire dvisual acuity.1-6 Although spontaneous resolution of the traction has been observed in about 11% of patients, surgical intervention to relieve the traction is necessary in many cases.7-9 Pars plana vitrectomy has been shown to relieve the vitreomacular traction and results in visual improvement in most patients with vitreomacular traction syndrome.7-13
Optical coherence tomography (OCT) has become a valuable diagnostic tool to evaluate the morphological features of macular changes, incomplete posterior vitreous detachment, and postoperative resolution of macular changes in vitreomacular traction syndrome.14-16 Diagnosis of the disorder is straightforward with OCT, even cases considered questionable by biomicroscopic examination. An OCT retinal mapping program, with additional radial scan images, has advantages compared to using a single line scan. A single line scan to measure retinal thickness provides incomplete information because it is only possible to obtain the thickness in one single A-scan, where as in retinal mapping with OCT, several A-scans are put together to calculate the mean thickness of the macula.17,18 From this program, six cross-sectional images can also be obtained for detailed examination of the vitreoretinal interface.19 In the current study, we performed preoperative OCT retinal mapping in six patients (6 eyes) with vitreomacular traction syndrome to evaluate the usefulness of OCT retinal mapping program in understanding the configuration of vitreoretinal adhesion and planning the surgical approach for the operation.
Materials and Methods
The study was a retrospective, interventional case series of consecutive patients diagnosed with vitreomacular traction syndrome at the vitreoretinal service clinic of the Yonsei University Eye, and Ear, Nose, and Throat Hospital, Seoul, Korea. Six eyes of six patients were included. All six patients underwent a complete ophthalmic examination, including dilated fundus examination using an indirect ophthalmoscope and 90+ diopter noncontact lens slit lamp biomicroscopy. In addition to routine ophthalmic examination, OCT retinal mapping using third generation OCT (OCT3; instrument manufactured by Stratus Zeiss Humphrey, San Leandro, CA) was performed preoperatively on all patients, as previously described.17 The diagnosis of vitreomacular traction syndrome was made when apparent traction from the vitreous causing increased thickness of the macula was observed. Internal fixation was used and the scanning and video images were displayed simultaneously to verify fixation. Six consecutive radial scans 30 degrees apart were obtained with a 6-mm length, centering on the patient's fixation point. The mean central macular thickness was calculated using the Early Treatment for Diabetic Retinopathy Study (ETDRS) central 1mm zone area of the macula. With the six radially scanned images, three-dimensional configuration of vitreomacular adhesion was analogized and the farthest point of the detached posterior hyaloid membrane from the retinal surface was located. After the location of the posterior hyaloid opening site, pars plana vitrectomy was performed on all six patients.
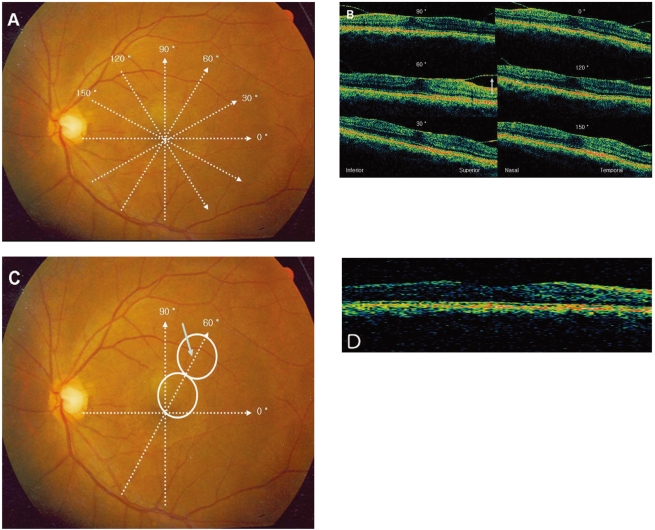
Pars plana vitrectomy using 25-G Transconjunctival Sutureless Vitrectomy (TSV) system was performed. After the core vitrectomy, access to the subhyaloid space was made by creating an opening with a 25-G needle at the previously located site based on the OCT retinal mapping. The posterior hyaloid membrane was then peeled off with a micropick in a circular fashion around the fovea.
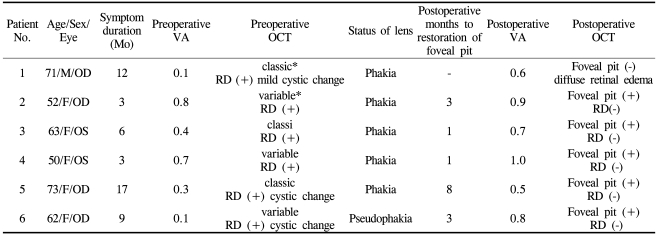
In patient 4, the located site was in the superotemporal area at the meridian of a 60 degree plane. Since the total scan length was 6 mm, the site might be between 2.5 and 3.0 mm apart from the foveal center. During the operation, we drew two imaginary circles, each the size of the optic nerve head (~1.5 mm in diameter), along the 60-degree plane and made an opening through the posterior hyaloid membrane within the second circle.The opening site was assumed to be about 2.5 mm away from the foveal center and corresponded to the preoperatively located site based on the OCT retinal mapping (Fig. 1). Then, the tractional posterior hyaloid membrane was peeled off as previously described (Fig. 2). The same surgical method was applied to all other patients.
Localization of the retinal opening site with OCT retinal mapping. (A) Preoperative OCT retinal mapping of patient 4 (50-year-old female, left eye) contains radial spoke pattern of six scans 6 mm long, centered on the patient's fixation point. (B) Cross-sectional optical coherence tomograms obtained from the corresponding six radial scans. A blue arrow points to the site with posterior hyaloid detachment farthest from the retina. (C) During the operation, two imaginary circles the size of the optic nerve head are drawn to approximate a length of 3 mm. The blue arrow within the second circle points to the opening site for an access to subhyaloid space. (D) Three months after the surgery, the foveal detachment has resolved and the foveal pit is restored. The OCT is taken at 60 degree plane.
Peeling of the posterior hyaloid membrane. (A) Creating an opening at the preoperatively located site with a 25 g needle. Since the posterior hyaloid membrane's detachment is farthest from the retina as shown on preoperative OCT retinal mapping,the procedure can be performed safely and effectively. (B) Peeling of the posterior hyaloid membrane with a micropick in a circular fashion around the macula.
Best corrected visual acuity and central macular thickness by OCT were measured before the operation and 3 months afterwards.
Statistical analyses utilized SPSS®12.0.1 (SPSS Inc., Chicago, IL) for Windows. Wilcoxon signed-rank tests were run to compare differences between follow-up and baseline data. The level of statistical significance was set at P<0.05.
Results
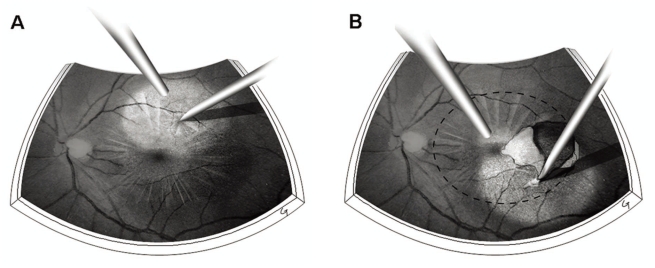
The baseline characteristics are listed in Table 1. All six patients had symptoms of reduced visual acuity and four of them had metamorphopsia. One eye was pseudophakic at symptom onset but did not have a temporal relationship with cataract surgery, which suggested possible postoperative complications were causing the macular changes.
Based on the classification by McDonald and associates5, three of the patients were classified as the classic type, characterized by midperipheral posterior vitreous detachment with persistent attachment to the macula and optic disc. The other three eyes were variable types with one or more quadrants attached to the vitreous, in addition to vitreomacular traction. Three of them had cystoid macular changes, presumed to be due to tractional etiology, and all of the eyes revealed tractional macular detachment.
Pars plana vitrectomy with TSV 25-G system was performed on all six patients. Posterior hyaloid membrane attached to the posterior retina was released by previously described method. No intraoperative complications were observed.
Best corrected visual acuity significantlyimproved from 0.4 to 0.75 with mean increase by 3.5 lines on a Snellen chart (Wilcoxon signed-rank test, P=0.027). The mean preoperative foveal thickness was 406 µm and significantly decreased to 241 µm 3 months after the operation (P=0.027). The foveal pit was restored in five patients and one patient had a remaining diffuse thickening of the macula, although the foveal thickness was significantly decreased. No patients had any signs of persistent vitreomacular traction or postoperative complications during thefollow-up period.
Discussion
Pars plana vitrectomy to release the tractional posterior hyaloid membrane has been the mainstay of the treatment for the vitreomacular traction syndrome.7-13 Several previous studies regarding the disorder reported excellent visual improvement after the operation.7-13
After the advent of OCT as an important diagnostic tool for the vitreomacular traction syndrome, a more precise understanding of the vitreoretinal attachment's configuration has become possible with additional images obtained by performing six consecutive radial scans 30 degrees apart with a 6 mm length centering on the patient's fixation point.14-19 In the current study, we used OCT retinal mapping to analogize the three-dimensional architecture of the vitreomacular adhesion and to select a safe access point into the subhyaloid space. With the OCT retinal mapping tomograms, making an access into the subhyaloid space could be conducted more safely and effectively at the site where the posterior vitreous detachment was farthest from the retinal surface. This technique is even more useful in variable types of the disorder with absence of vitreous separation in the midperiphery and localized perifoveal hyaloid detachment, which is shallow and invisible. All of these factors could make access to the subhyaloid space a technically challenging procedure using a conventional technique. After making an opening to the subhyaloid space, we peeled off the posterior hyaloid membrane by circumscribing it around the fovea through the opening site. By circumscribing the posterior hyaloid membrane, the traction on the macula during the procedure could be minimized. Regarding the surgical outcomes of the variant types, Yamada and associates20 previously reported that patients with V-shaped incomplete posterior vitreous detachment (classic type) responded more favorably after the operation than those with partial posterior vitreous detachment temporal to the fovea but attached nasally and developed into cystoid macular edema (variant type), which could lead to a macular hole or macular atrophy. However, Johnson21 reported excellent outcomes in variant vitreomacular traction syndrome by using the surgical technique of making an opening in the perifoveal hyaloid membrane and circumscribing the vitreous around the fovea to avoid traumatic separation. In the current study, we observed significant functional and anatomical improvement of vitreomacular traction syndrome regardless of disorder type. The visual outcomes were even better in variable types, with a postoperative visual acuity of 0.8 or better in all three patients.
In conclusion, OCT retinal mapping program is a valuable diagnostic tool in determining the configuration of the vitreomacular adhesion and planning the surgical approach during procedures for vitreomacular traction syndrome.