Comparison between Anterior Corneal Aberration and Ocular Aberration in Laser Refractive Surgery
Article information
Abstract
Purpose
To compare changes of anterior corneal aberration (Pentacam®) and ocular aberration (aberrometer, LADARWave®) after laser refractive surgery.
Methods
Sixty-six eyes underwent laser refractive surgery and were retrospectively reviewed. Anterior corneal aberration and ocular aberration were measured by Pentacam® and an aberrometer (LADARWave®) respectively. Changes of root mean square (RMS) values of coma, spherical aberration, and total high order aberration (HOA) were evaluated before, 1 month, and 3 months after surgery
Results
Ocular aberrations displayed low preoperative values, but after laser refractive surgery, anterior corneal aberration and ocular aberration increased equally. There were no statistically significant differences of internal optics aberration values (ocular aberration minus anterior corneal aberration) in coma, spherical aberration, and total HOA. Anterior corneal aberration and ocular aberration showed statistically significant correlations at 1 and 3 months after surgery.
Conclusions
Internal optics aberration compensated the anterior corneal aberration effectively before surgery, but the increase of anterior corneal aberration after laser refractive surgery exceeded the compensation of internal optics. As a result, anterior corneal aberration and ocular aberration increased equally. The correlation between anterior corneal aberration and ocular aberration after surgery was statistically significant due to the increased proportion of anterior corneal aberration in ocular aberration.
Since Trokel et al. used an excimer laser to correct the refractive state of eyes in 1985, laser refractive surgery has advanced and become a generalized method for myopia correction.1-3 Patients' expectations for surgery increased and not only the quantitative improvement of vision but also the 'quality of vision' became an important issue.
Aberration is defined as the difference between a real image and an ideal image and if it occurs, the quality of vision becomes poorer; its importance is now being emphasized as a measurement of visual quality. Aberration is divided into low order aberrations and high order aberrations (HOAs). Low order aberrations represent simple refractive errors including defocus and astigmatism. HOAs include coma and spherical aberration. Conventional refractive surgery has focused on the correction of only low order aberrations, but HOAs can now be corrected by customized refractive surgery.4-8
Ocular aberration consists of anterior corneal aberration and internal optics aberration (Fig. 1). Internal optics includes the posterior corneal surface as well as the lens and vitreous body. In normal eyes, high values of anterior corneal aberration are compensated by negative values of internal optics aberration and as a result, ocular aberration values decrease.9,10 When laser refractive surgery is performed, aberrations are increased by deforming the anterior corneal surface.

Schematic diagram of composition of aberration. Complete ocular (eye) aberration is composed of the anterior corneal aberration (red color) and internal optics aberration (blue color).
In this study, changes of anterior corneal aberration and ocular aberration were evaluated by Pentacam® (Oculus, Germany) and LADARWave® (Alcon, USA), respectively, before and after laser refractive surgery. In addition, the correlation between the aberrations was examined.
Materials and Methods
Thirty-three patients (66 eyes; mean age 25.5±15.6 years) who underwent laser refractive surgery for myopia correction between November 2006 and May 2007 followed up for more than 3 months were retrospectively reviewed. Twenty-eight patients underwent laser in situ keratomileusis (LASIK) surgery, and 5 patients underwent photorefractive keratectomy (PRK) surgery. All surgeries were performed using LADARVision 4000® (Alcon, USA) by a single surgeon (Park WC). Anterior corneal aberration and ocular aberration were measured by Pentacam® and an aberrometer (LADARWave®), respectively, before, 1 month, and 3 months after surgery, with the diameter of the measured zone set to 6.5 mm. Among HOAs, coma, spherical aberration, and total HOA values were investigated. Total HOA was calculated as a root mean square (RMS) value between the 3rd and 6th order aberrations.
Pentacam® is a rotating Schiempflug camera, which generates images from the anterior surface of the cornea to the posterior surface of the lens, and can create a corneal elevation map. Pentacam® can also perform Zernike analysis for the anterior and posterior surface based on the measured height data up to the 8th order aberration. LADARWave® is an aberrometer using the Hartmann-Shack sensor and measured up to the 6th order aberration in the present study. Total HOA was calculated up to the 6th order aberration for comparison between Pentacam® and LADARWave®.
Statistical analysis was performed using the Statistical Product and Service Solutions Software 15.0 for MS Windows (SPSS Inc, USA). A paired t-test was used to analyze changes of aberrations before and after surgery. Correlations between the aberrations were analyzed by bivariate correlation analysis calculating the Pearson correlation coefficient. A p-value less than 0.05 was considered statistically significant.
Results
1. Anterior corneal aberration and ocular aberration before and after surgery
Anterior corneal aberrations and ocular aberrations were measured by Pentacam® and an aberrometer (LADARWave®), respectively, before, 1 month, and 3 months after surgery. Internal optics aberration values, ocular aberration minus anterior corneal aberration, were also calculated. Before surgery, the positive values of anterior corneal aberrations were compensated by negative values of internal optics aberrations, and complete ocular aberrations were measured low. There were no significant changes of internal optics aberrations after surgery, and aberrations of internal optics remained relatively constant (Table 1).
The mean preoperative value of total HOAs was 0.416±0.113 µm, anterior corneal surface value was 0.782±0.136 µm, and internal optics value was -0.366±0.172 µm. At 1 month after surgery, anterior corneal aberration and ocular aberration increased to 1.152 µm and 0.737 µm, respectively, but aberration of the internal optics remained at -0.415 µm, similar to the preoperative value. At 3 months after surgery, anterior corneal aberration and ocular aberration continued to increase, but the internal optics aberration remained constant.
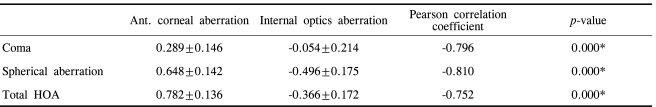
2. Correlation between anterior corneal aberration and internal optics aberration before surgery
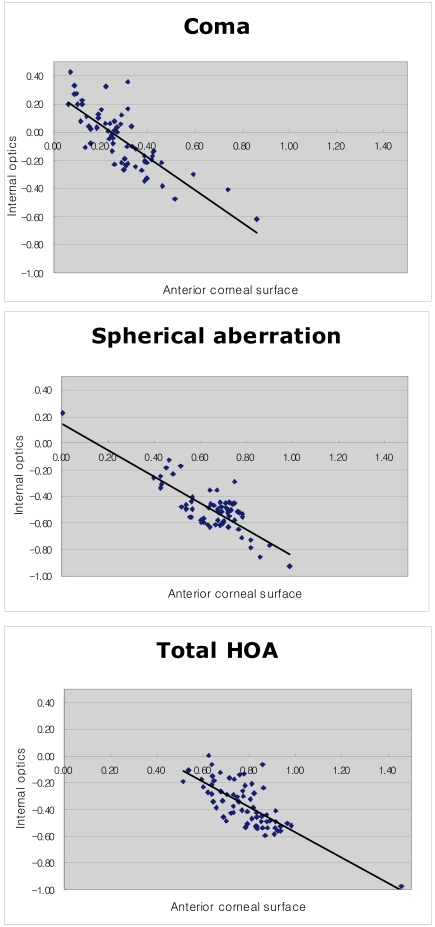
When the bivariate correlation analysis was performed to evaluate the correlation between anterior corneal aberration and internal optics aberration before surgery, the Pearson correlation coefficients were -0.796, -0.810, and -0.752 in coma, spherical aberration, and total HOA, respectively (p=0.000) (Table 2). These results displayed a negative correlation between the anterior corneal aberration and internal optics aberration (Fig. 2).
3. Changes of HOAs before and after surgery
Drawing graphs pertaining to the changes of HOAs before and after surgery, the anterior corneal aberration and ocular aberration were observed to increase equally, while the internal optics aberration maintained at a low level (Fig. 3). In the case of spherical aberration, a high value of anterior corneal aberration (0.648 µm) was compensated by the negative value of the internal optics aberration (-0.496 µm), allowing the ocular aberration (0.152 µm) to remain at a low level (Fig. 3). Similar patterns were found for coma and total HOA. Calculating increasing rates of aberrations before and 3 months after surgery, coma, spherical aberration and total HOA increased 1.7-, 2.6-, and 1.8-fold from previous values in anterior corneal aberrations, respectively. In ocular aberrations, coma, spherical aberration, and total HOA increased by 1.5, 1.4, and 1.5 times that of previous values, respectively (Table 1). Regarding internal optics aberrations, there were no statistically significant differences before and after surgery in coma, spherical aberration, and total HOA (all p>0.05).
4. Correlation between anterior corneal aberration and ocular aberration
Before surgery, correlations between anterior corneal aberration and ocular aberration were not statistically significant for coma, spherical aberration, and total HOA, but became statistically significant after surgery. One month after surgery, the Pearson correlation coefficient values were 0.535, 0.662 and 0.696 (all p=0.000) in coma, spherical aberration, and total HOA, respectively. Three months following surgery, the correlation coefficients were 0.413, 0.604, and 0.734 with p-value 0.001, 0.000, 0.000, respectively (Table 1).
Discussion
Aberration is the difference between a real image and an ideal image occurring when plane wavefront is refracted by Snell's law. Ideally, parallel light focuses on one point. However, the eye is not a perfect circle for focusing incoming light on one point, and eventually an aberration occurs.
Zernike analysis is commonly used in ophthalmology to express ocular wavefront error in the form of a polynomial equation. Specifically, the Zernike polynomial describes the shape contribution made by a series of sine and cosine basis functions to the total wavefront error surface. The RMS is a measure of the magnitude of the wave aberration.11,12
Increased HOA after laser refractive surgery causes complications such as a decrease in contrast sensitivity, halos, glare, starbursts, and ghost images, which degrade visual quality.4-8 McCormick et al. verified the mean HOA of patients complaining of complications increased 2.26-fold higher than that of patients without problems.8
Ocular aberration is composed of an anterior corneal aberration and internal optics aberration. In principle, internal optics aberration should be measured directly, but direct measurement is difficult in all patients. Artal et al. compared directly measured internal optics aberrations after neutralizing anterior corneal aberrations by water-filled goggles and indirectly calculated internal optics aberrations by subtracting anterior corneal aberrations from ocular aberrations. The result showed that directly and indirectly measured values of internal optics aberrations were the same.9 Based on this study, internal optics aberration was defined in the present study as ocular aberration minus anterior corneal aberration, which were measured by LADARWave® and Pentacam®, respectively.
The compensating effect of internal optics aberration for anterior corneal aberration contributes to acquisition of a fine image.9,10 In this study, a negative correlation between the anterior corneal aberration and internal optics aberration before surgery was identified (Table 2). Additionally, results confirmed that the positive values of anterior corneal aberrations were compensated by negative values of internal optics aberrations, and complete ocular aberrations were maintained at a low level before surgery.
An increase in aberration after conventional refractive surgery has been confirmed by numerous studies.7,13,14 However, studies regarding aberration changes after customized refractive surgery have produced varying results. An increase in aberrations but lower increasing rates than conventional refractive surgery15-18, no significant increase19, or even a decrease in aberrations20 than the preoperative state has been reported. In this study, anterior corneal aberrations were increased, but internal optics aberrations were not influenced by surgery and remained constant. As a result, ocular aberration increased to the same degree as the anterior corneal aberration increased. Graphs pertaining to changes of HOAs before and after surgery also showed that the anterior corneal aberration slope and the ocular aberration slope increased at same rate, while internal optics aberration maintained a low level (Fig. 3). Calculating increasing rates of aberrations before and 3 months after surgery, coma, spherical aberration and total HOA increased by 1.7-, 2.6-, and 1.8-fold from previous values in anterior corneal aberrations and 1.5-, 1.4-, and 1.5-fold from previous values in ocular aberrations, respectively (Table 1). Regarding internal optics aberrations, there were no statistically significant changes in coma, spherical aberration and total HOA before and after surgery (all p>0.05).
Correlations between anterior corneal aberration and ocular aberration were not significant in coma, spherical aberration, and total HOA before surgery, but became statistically significant in all aberrations after surgery (Table 1). This can be explained by the increase of anterior corneal aberration after surgery which exceeds the limit of the compensating effect of internal optics aberration. This alteration is believed to result in a larger proportion of anterior corneal aberration in ocular aberrations and to induce changes of correlation between anterior corneal aberration and ocular aberration.
Patients in the current study were followed up for 3 months after surgery, but more time was necessary to observe complete changes in HOA. Additionally, various methods of surgery were included in this study, but there were not enough cases to identify any differences among these methods. The authors are planning to study the differences of aberrations depending on laser refractive surgery methods by including more cases and a longer follow-up period.
An increase of HOA after refractive surgery could degrade the quality of vision, and thus accurate analysis of the aberrations and techniques to lower HOA is imperative to improve visual quality.
Notes
This study was presented at the 98th annual meeting of the Korean ophthalmological society in November, 2007.