Serous retinal detachment secondary to choroidal ischemia have been reported in very few cases in the literature but is a well-documented cause of visual loss in preeclampsia or disseminated intravascular coagulation (DIC).1,2 We report the case of a 71-year-old woman who developed unilateral choroidal ischemia with serous retinal detachment associated with severe pain following total knee replacement arthroplasty (TKRA). There were spontaneous resolutions of the serous detachment and the choroidal changes with residual pigment epithelial changes. To our knowledge, this is the first report describing serous macular detachment following severe postoperative pain.
Case Report
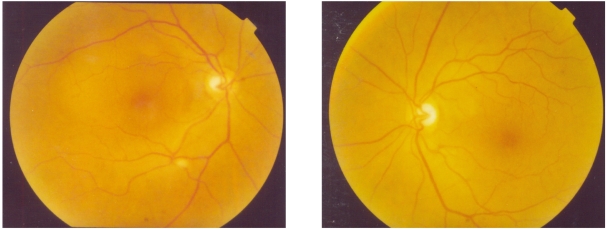
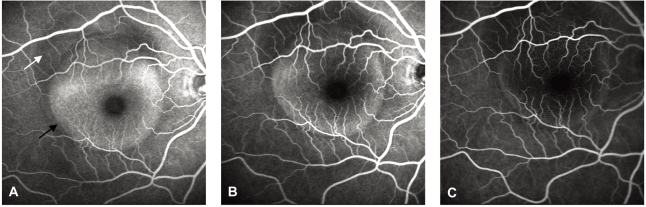
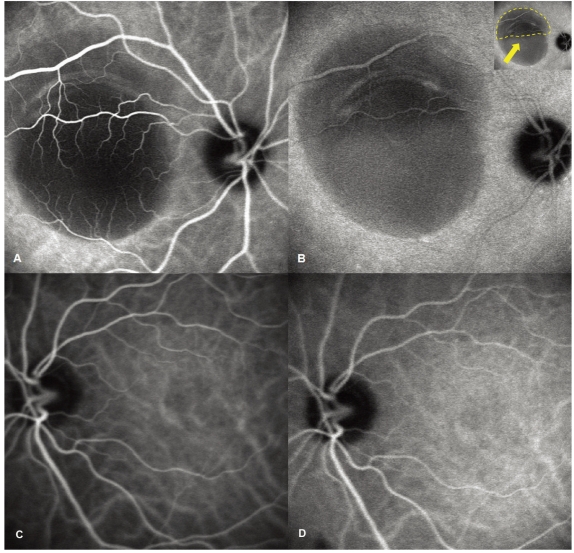
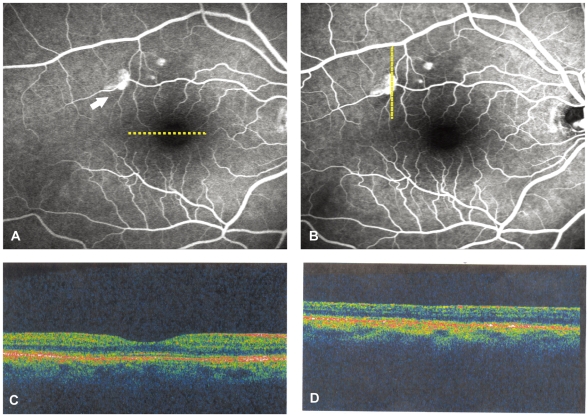
A 71-year-old woman presented with a complaint of sudden decrease in vision in the right eye, 7 days after TKRA. The patient's history was unremarkable except a severe pain of more than the visual analog scale of 8 points for about 2 days, because the analgesic dose given was not adequate for the pain after the surgical operation. On examination the best corrected visual acuity (BCVA) was 20/100 in the right eye and 20/20 in the left eye. Retinal examination showed a well differentiated serous detachment that was about 3.5 disc diameter in size and located on the macular area in the right eye. No disc edema, retinal cotton wool spots, hemorrhages, or vascular abnormalities were noted in both eyes (Fig. 1). A fluorescein angiography (FA) of right eye performed at the first visit revealed choroidal hypoperfusion and a serous detachment without any leakage points in the early phase of the angiogram (Fig. 2A). In the mid and late phases, the area of non-perfusion showed pooling of the dye in the subretinal space without a leakage point (Fig. 2B, C). Indocyanine green (ICG) angiography was also performed on the same day and showed delayed perfusion of the choriocapillaris without a leakage point in the early phase followed by slow filling of neurosensory detachment without a focal source of leakage in the late phase (Fig. 3A, B). The areas of choroidal hypoperfusion corresponded to the serous detachment seen clinically. There was no disturbance of the retinal pigment epithelium (RPE). After 2 months, the symptoms and clinical findings began to improve gradually and at the follow-up examination 6 months after the first clinic visit, there was a complete resolution of the serous detachment of macula. The BCVA had improved to 20/20 in the right eye and the fluorescein angiogram showed minor disturbances in the RPE only (Fig. 4).
Discussion
Serous detachment of the neurosensory retina can occur due to any process that disrupts the outer blood-ocular barrier controlled by the RPE.3 Diagnosis of a serous detachment is made clinically, although optical coherence tomography has recently been used for the detection of clinically occult serous elevations of the retina. The underlying mechanisms of subretinal exudation are thought to include choroidal vascular perfusion and permeability changes, which result in increased choroidal interstitial fluid with further extension into the subretinal space.3 In our case, this 71-year-old woman presented with a unilateral choroidal ischemia with serous macular detachment detected by FA and ICG angiography. The most common cause of this finding is the neovascular form of age related macular degeneration.3,4 However, the patient did not have subretinal hemorrhages, exudates or fibrosis at any time.5 Other signs of choroidal neovascualr membrane including a gray-green membrane and pigment epithelial detachment were also absent. Subretinal leakage, due to altered choroidal vascular perfusion and permeability, occurs in systemic inflammatory and infectious diseases with fluid extension into the subretinal space.3 Systemic malignant hypertension, toxemia of pregnancy, and hypercoagulable states may result in choriocapillaris occlusion and choroidal ischemia with subsequent breakdown of the outer blood ocular barrier and serous detachment.3,6 However, the patient had no significant ophthalmic history and her medical history and review of systems were unremarkable. In addition, there was no history of systemic steroid use. Other causes of serous macular detachment include acute and chronic central serous chorioretinopathy (CSC). However, FA failed to show focal RPE leaks, RPE stippling, or gravitational fluid tracts consistent with CSC.7,8 The ICG angiography showed a slow pooling of ICG in the subneurosensory space but failed to demonstrate focal leaks or frank choroidal leakage as seen in CSC. Idiopathic CSC in a resolving phase with early resolution of fluorescein leakage and persistence of subretinal fluid, might present with serous macular detachment. However, the acute onset of visual loss in a close temporal relationship to severe postoperative pain that interfered with sleep for 2 days after surgery (visual analog scale: 8 points) and the constant pain (visual analog scale: 2~4 points) despite narcotic analgesics suggest a different etiology. A search of the medline database (search words used: choroidal ischemia, pain, serous retinal detachment) showed no studies on choroidal hypoperfusion and serous detachment related to severe pain. Generally, pain reacts to nociceptive stimulation, and primarily secretes histamine or substance P, and serotonin; secondary stimulation of the sympathetic nervous system follows.9 It is possible that the sympathetic innervation produced vasoconstriction and alteration of blood flow in the choroidal vascular beds leading to choroidal hypoperfusion. Compromised function of the retinal pigment epithelium and/or choroid would lead to accumulation of subretinal fluid as is observed in our patient with a serous detachment. A recent survey investigation of the severity of pain, following ambulatory surgery in 5,703 patients, indicated that 30%(1,712) of the patients experienced moderate-to-severe pain postoperatively. However, because individual tolerance to pain varies, patients who have pain do not always present with ocular symptoms.10 Therefore, we propose that severe postoperative pain influences sympathetic activity that can result in ischemic injury with focal choroidal vascular compromise and secondary dysfunction of the overlying REP cells; this may occur in some patients and lead to leakage across the RPE and accumulation of subretinal fluid. Further investigation of the potential impact of pain on the delicate balance of fluid homeostasis, at the outer blood-ocular barrier, may be warranted.



 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print






