Efficacy of Intravitreal Triamcinolone Acetonide for Eyes with Postvitrectomy Diabetic Vitreous Hemorrhage
Article information
Abstract
Purpose
To evaluate the efficacy of intravitreal triamcinolone acetonide (IVT) for the management of postvitrectomy diabetic vitreous hemorrhage.
Methods
The authors conducted a retrospective study of patients with postvitrectomy diabetic vitreous hemorrhage who were administered 4 mg (0.1 cc) of triamcinolone acetonide ophthalmic suspension. Ocular history, adverse events, BCVA, intraocular pressure, external eye examination, slit-lamp biomicroscopy, fundus examination, B-scan ultrasonography, and fundus photography were assessed on day 1, weeks 1, 2, and 4 and months 2 and 3.
Results
There were 19 eyes of 18 consecutive patients with mean follow-up after IVT injection of 28 weeks. Of the 19 eyes, 17 eyes (89%) experienced clearing of vitreous hemorrhage within 1 to 5 weeks (mean, 1.7 weeks) with visible triamcinolone precipitates along with blood clot in the inferior aspect of fundus. Of these 17 eyes, 12 eyes (63%) maintained vitreous hemorrhage-free condition at last follow-up with a mean visual acuity of 20/63 (range, 20/320 20/25), whereas 5 (29%) developed recurrent vitreous hemorrhage after clearing of vitreous hemorrhage. Vitreous hemorrhage was not cleared in 2 eyes, which required surgical procedures.
Conclusions
IVT injection may be beneficial for clearing recurrent postvitrectomy Diabetic Vitreous Hemorrhage.
The incidence of recurrent vitreous hemorrhage of proliferative diabetic retinopathy following posterior vitrectomy ranges from 12 % to 63 %.1-3 Recurrent vitreous hemorrhage may be caused by the dissolution of blood clots trapped in the remaining anteroperipheral vitreous gel, remnants of fibrovascular tissue, reactivation of retinal sites that bled intraoperatively, anterior hyaloidal fibrovascular proliferation, or neovascularization originating from the sclerotomy sites.4-5 This condition is usually managed by fluid-gas exchange or vitreous cavity washout.6-7
Intravitreal triamcinolone acetonide (IVT) has been shown to be a useful adjunct therapy for intraocular edematous and neovascular disease.8-12 Corticosteroids are used in the treatment of various retinal diseases primarily for their anti-inflammatory and anti-angiogenic effects. Corticosteroids inhibit rostaglandins and inflammatory adhesion molecules, thus contribute to the stabilization of the blood-retinal barrier.13-15 Corticosteroids also inhibit expression of the vascular endothelial growth factor (VEGF), as well as the induction of VEGF by platelet-derived growth factor (PEGF) and platelet activating factor (PAF).16
We have found that IVT, when used along with vitrectomy for the treatment of proliferative diabetic retinopathy, facilitates the absorption of macular edema. Follow up examinations have shown the triamcinolone precipitates downward of vitreous cavity along with retained blood. We have therefore assessed the efficacy of IVT for the management of postvitrectomy diabetic vitreous hemorrhage.
Materials and Methods
Among the patients at Asan Medical Center from April 1 through November 30, 2005, we conducted a retrospective study of 19 eyes of 18 patients who received IVT injection for postvitrectomy diabetic vitreous hemorrhage. The 19 eyes in this study included those who previously had three-port pars plana vitrectomy, with or without cataract operation for nonclearing vitreous hemorrhage (11 eyes), and vitreous hemorrhage with traction retinal detachment (8 eyes). The risks and benefits of the procedure were discussed with each patient before injection, and all patients provided written informed consent. This study had Institutional Research Board approval.
The degree of intravitreal hemorrhage was scaled according to the diabetic retinopathy vitrectomy study grading system (Table 1).17 Baseline parameters were documented, including visual acuity, intraocular pressure (IOP), lenticular status and retinal attachment through the B-scan. The eye was cleansed with 10% Betadine (Becetin®, Hyundai Pharm, Seoul, Korea) solution. A sterile lid speculum was placed in the eye, and sterile topical lidocaine was used to anesthetize the inferotemporal quadrant. Triamcinolone acetonide (4 mg/0.1 ml; TRIAM®; Shinpoong, Seoul, Korea) was injected inferotemporally through the pars plana using a 30 gauge needle on a tuberculin syringe.
Response to treatment was monitored on day 1, weeks 1, 2, and 4, and months 2 and 3 by Snellen visual acuity and biomicroscopic examination. IOP was recorded at every visit, along with potential corticosteroid-induced and injection-related complications. Other assessments included ocular history, adverse events, external eye examination, fundus examination, B-scan ultrasonography, and fundus photography.
Results
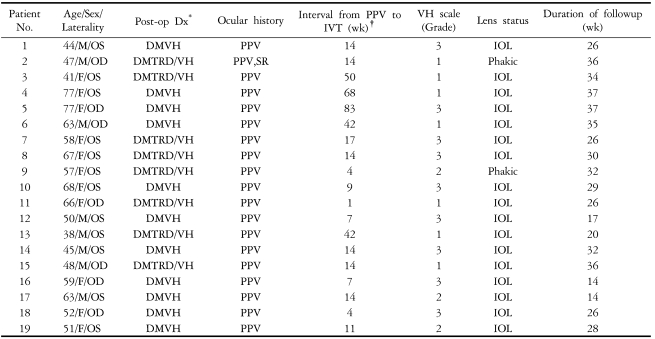
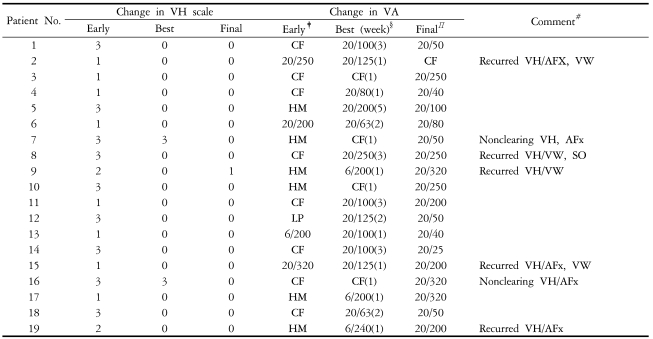
A total of 19 eyes from 18 patients were reviewed. Patient's age, gender, ocular laterality, diagnosis of prior vitrectomy, and interval between vitrectomy and IVT injection are described in Table 2.
The visual acuity of 15 eyes at the time of IVT injection ranged from LP to CF, and in 4 eyes the visual acuity was slightly better than CF. Nine eyes had grade 3 VH (severe vitreous hemorrhage with no retinal details and no orange fundus reflex), 2 eyes had grade 2 VH (moderate vitreous hemorrhage with no visible fundus details but with orange fundus reflex) and 8 eyes had grade 1 VH (mild vitreous hemorrhage with visible fundus details). Mean follow-up after IVT injection was 28 weeks (range, 14-37 weeks). The vitreous hemorrhage was cleared in 17 of the 19 eyes (89%) within 1 to 5 weeks (mean, 1.7 weeks); in 11 of these 17 eyes, it was cleared within 1 week (Table 3). The fundus was clearly visible in all 17 of VH clearing eyes, and triamcinolone precipitates were observed along with retained blood clots (Fig. 1). All but one of these 17 eyes had visual improvement, with a mean visual acuity of 20/160 (range, CF to 20/63) within 1 to 5 weeks. At last follow-up, 12 of the 17 eyes maintained VH-free condition with the mean visual acuity of 20/63. (range, 20/320 to 20/25) Of the 17 eyes that cleared, 5 subsequently developed recurrent vitreous hemorrhage, and these underwent air-fluid exchange or vitreous cavity washout. VH was not cleared in 2 eyes, and vitreous cavity washouts were performed.
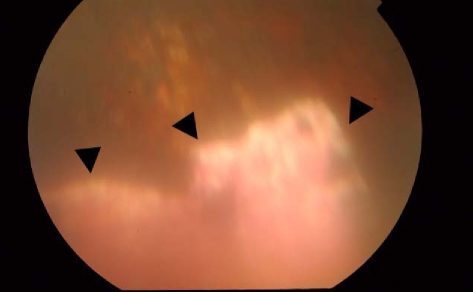
Fundus photograph of patient No. 17 showing the inferior peripheral aspect of retina at 1 week after intravitreal triamcinolone injection for recurrent postvitrectomy diabetic hemorrhage. Previous laser photocoagulation scars (upward) and whitish precipitation of triamcinolone with reddish blood clots on the precipitation (downward, arrow) can be seen.
IOP increased in 7 eyes during the follow-up period; in one, increased IOP was due to recurrent VH. Of the 7 eyes, 6 were treated with topical antiglaucomatous medication and 1 was managed for recurrent VH. There was no significant cataract progression in the 2 phakic eyes, and no procedure-related complications during follow-up.
Discussion
VH is the most common complication of vitrectomy for diabetic retinopathy. Despite measures to prevent and control this bleeding, it can lead to air-fluid exchange in the office or to additional surgery in the operating room. Air-fluid exchange does not result in clear vision immediately after the procedure, and the patient has to maintain a face-down position. Vitreous lavage combined with/without air tamponade, a more invasive procedure performed in the operating room, may give rise to complications such as iatrogenic retinal breaks, incarcerations of vitreous in the sclerotomy sites, retinal detachment, rubeosis iridis, neovascular glaucoma and infective endophthalmitis.18 With lack of large number of patients, longer follow-up and control group, it is hard to say that IVT injection is superior to common standard treatment such as air-fluid exchange and vitreous lavage or as much efficient as those treatments. However, in our study, most eyes with clearing VH improved their visual acuity within 1 to 5 weeks (mean; 1.7 weeks) and in 11 of these 17 eyes, VH was cleared within 1 week. Thus possibly more rapid clearing of VH by IVT injection than natural course may enable faster visual rehabilitation and additional laser photocoagulation which may prevent recurrence of VH. When spontaneous clearing occurred, it usually did so in 7-11 weeks.6 Additionally, in terms of less invasiveness and avoiding face-down position, IVT injection may be more convenient.
It is still unclear how IVT injection can cause clearing the vitreous hemorrhage. We suppose that the mechanical downward sedimentation of triamcinolone in the vitreous cavity with the adherent remaining blood may play a role since this phenomenon is always observed once the fundus becomes visible.. One thing remarkable is that IVT injection is only useful for VH in the vitrectomized eye rather than non-vitrectomized eye to our best knowledge. Considering the difference in vitrectomized and non-vitrectomized eye, we are presuming a 'sedimentation' theory. In addition, induction of direct vascular stabilizing effect may play a role in maintaining VH-free condition. At the time of last follow-up (mean, 28 weeks), 12 of 19 eyes maintained their VH-free condition.
With respect to the VH scale, the 2 eyes that did not clear were grade 3. Of the 17 eyes that cleared, 8 eyes were grade 1, 2 eyes were grade 2, and 7 eyes were grade 3. The 5 eyes that showed recurrent hemorrhage varied in VH scale from grades 1 to 3. With this small sample size, we can not find any statistical significant relationship between VH scale and efficacy of IVT injection.
Significant adverse effects of the IVT injection procedure were infrequent. The remarkable complications were non-clearing of the vitreous hemorrhage, requiring vitreous cavity washout in 2 eyes (10%), recurrent vitreous hemorrhage in 5 eyes (26%), and procedure related IOP increase in 6 eyes (31%) which were controlled well with topical antiglaucomatous agent. There was no evidence of cataract progression in the 2 phakic eyes.
IVT injection can delay surgical intervention. With early treatment of preproliferative diabetic retinopathy and advancement of vitrectomy, the risk of anterior hyaloidal fibrovascular proliferation can be decreased. Additionally, triamcinolone has anti-proliferative and anti-inflammatory properties. IVT injection combined with pars plana vitrectomy as an adjunct treatment of proliferative vitreoretinopathy was shown to lower intraocular inflammation, postoperative pain and incidence of re-operations caused by preretinal fibrous membrane formation.10,19 Triamcinolone may induce regression of neovascular iris vessels.20-21 Thus, delaying surgical intervention through IVT injection does not appear to negatively affect final visual outcome. In this study, fibrovascular ingrowths at sclerotomy sites were not found in nonclearing VH or recurrent VH that required vitrectomy.
We recognize that the limitations of our work include a small sample size; no comparison with natural course of recurrent VH; limited success in clearing VH, and relatively short follow-up time. Despite these limitations, IVT injection as an optional treatment of post vitrectomy diabetic VH is a less invasive procedure that possibly provides quicker visual recovery while avoiding the patient keeping a face-down position.
In conclusion, IVT injection may be beneficial for prompt clearing of recurrent postvitrectomy diabetic VH and maintaining VH-free condition, possibly by mechanical sedimentation with retained blood clots and the vascular stabilizing effects of triamcinolone. We have started on a randomized controlled clinical trial with air-fluid exchange and IVT injection to assess the safety and efficacy with long term follow up.
Notes
Presented at the 2006 annual meeting of the Association for Research in Vision and Ophthalmology.