Visual Function after Primary Posterior Chamber Intraocular Lens Implantation in Pediatric Unilateral Cataract: Stereopsis and Visual Acuity
Article information
Abstract
Purpose
To investigate the association between binocular function and vision after cataract removal and primary posterior chamber intraocular lens (PC-IOL) implantation in children with unilateral cataract and to identify visual function differences according cataract type.
Methods
Clinical records of 2- to 6-year-old patients with unilateral cataract removal and primary PC-IOL implantation were reviewed retrospectively. Visual acuity and ocular alignment were measured. Sensory fusion was assessed with the Worth 4-dot test, and stereoacuity with the Titmus stereo test. Cataracts were classified according to cause, lens opacity location, age at onset, and presence of strabismus. Clinical characteristics of patients who obtained good visual function were identified.
Results
Forty-seven patients were included. Among 22 (46.8%) with good vision (20/40 or better), only 6 (27.3%) achieved good binocular function (the presence of fusion and 100 seconds of arc or better of stereoacuity). Visual acuity was better in eyes with good binocular function (p=0.002). No other variables were significant for achieving good binocular function.
Conclusions
The removal of unilateral cataract in a visually immature child can result in a combination of good visual acuity and binocular function. Good binocular function is closely related to good visual acuity.
Cataracts are a major cause of childhood blindness, with a prevalence of 1.2 to 6.0 cases per 10,000 births.1 Visual rehabilitation, especially in children with unilateral cataracts, remains challenging, and results are frequently disappointing.
Over the past several decades, visual outcomes after cataract extraction have dramatically improved due to earlier surgery, greater attention to aphakia optical correction with contact or intraocular lenses (IOL), and occlusion therapy.2-6The development of useful binocularity has also been considered hard to achieve, but recent case reports and small case series describe patients with good central vision as well as stereopsis or other evidence of binocularity.7-10 However, previous reports combined unilateral and bilateral cataract results,10 and studies on unilateral cataract only had small sample sizes.7-8 Furthermore, most studies included patients who underwent various treatment methods for aphakic eyes,such as contact lenses, epikeratophakia, and primary or secondary IOL implantation.7-10
The purpose of this study is to investigate the frequency of attaining good binocular function and vision after unilateral cataract removal and primary posterior chamber IOL implantation and to identify which children have the best opportunity for good visual function. The difference of visual function according to cataract type is also investigated.
Materials and Methods
A series of consecutive clinical records of 2- to 6-year-old patients diagnosed with unilateral cataract who underwent cataract removal and posterior chamber intraocular lens (PC-IOL) implantation at Seoul National University Children's Hospital between February 1995 and June 2004 were reviewed retrospectively. Patients with visual outcomes possibly predetermined by co-existing organic ocular defects were excluded; these defects included cataracts secondary to retinopathy of prematurity and those associated with dense corneal opacity and posterior-type persistent hyperplastic primary vitreous (PHPV).
Cataracts were classified by etiology as congenital, developmental, or traumatic. A congenital cataract was defined when the condition was detected before 3 months of age, with a consideration of opacity location, associated micro-ophthalmia or microcornea or the isolated presence of nuclear cataract. Cataracts were categorized by opacity location as nuclear, lamellar, posterior subcapsular, and mixed type. Age at onset was determined by pediatrician or ophthalmologist examination, parental observation, or date of ocular trauma. Ocular deviations were measured in prism diopters (PD). Children with visual axis deviation equal to or greater than 10PD and those with previous strabismus surgery were considered to have strabismus.
Sensory fusion was assessed by the Worth 4-dot test with red-green glasses. Near (1/3 meter) and distance (6 meters) fusion was measured. Stereoacuity was assessed by the Titmus stereo test. Near fusion and Titmus stereo test was performed with their near glasses or by adding +3.0 diopters trial lenses on the pseudophakic eyes. Binocular function was graded as "good" if there was distance and near fusion of the Worth 4-dot test, and if measured stereo acuity was 100 seconds of arc or better.
Visual acuity was measured with the fixation pattern or Snellen letters in preliterate and literate children, respectively. The best-corrected visual acuity measured during binocular function test was noted. Visual acuity levels between 20/20 and 20/40 were considered "good." During binocular function assessment, refractive error was also measured in manifest or cycloplegic manners. Patients with a refractive error difference of 2 diopters or larger were considered to have anisometropia.
Surgery was performed by a single surgeon (YS Yu). All procedures were performed under general anesthesia, including mechanical anterior capsulorrhexis and lens material aspiration by a mechanical irrigation-aspiration instrument. Posterior capsulectomy with anterior vitrectomy was performed in children with posterior capsular opacities at the time of surgery. Children had simultaneous PMMA IOL implantation in the posterior chamber. IOL power was calculated using the SRK-II formula, with the goal of attaining emmetropia after the age of six. Between 2 and 5 years, the refractive goal was adjusted to allow 4.0D to 1.0D more of hyperopia.
Occlusion therapy was initiated when optics were sufficient to provide a clear retinal image. Recommended occlusion ranged from 1 to 6 hours a day and was prescribed according to patient age and the visual acuity level of the affected eye. Patching compliance was subjectively assessed as poor, moderate, or good by parental interviews on follow up.
Studied parameters were age at onset, sex, cataract type, opacity location, presence of strabismus pre- or postoperatively, anisometropia, and occlusion therapy compliance. The association of each independent variable with clinical outcome was estimated by chi-square test for discrete variables and student t test or Fisher's exact test for continuous variables.
Results
Forty-seven patients were included in the study with 14, 27, and 6 congenital, developmental, and traumatic cataracts, respectively. Of the 27 eyes with developmental cataracts, 10 were posterior lenticonus and 2 were PHPV. Twenty-nine (61.7%) patients were male and 18 (38.3%) were female. Mean age at onset was 47.7±18.9 months (3-71 months). Mean age at cataract surgery was 53.2±15.6 months (24-72 months), with mean follow-up of 47.3±29.9 months (8-126 months).
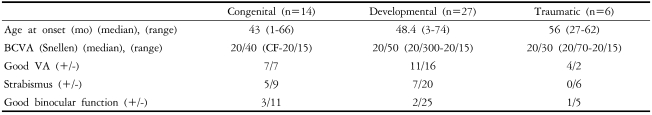
Clinical characteristics of the different cataract groups are listed in Table 1. There were no significant differences in best corrected visual acuities, presence of strabismus, or good binocular function.
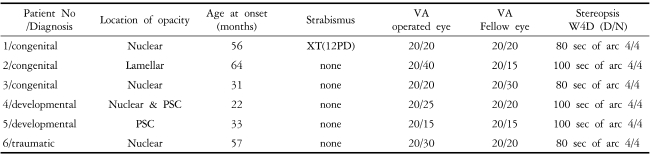
Overall, visual acuity was 20/40 or better in 22 (46.8%) eyes, with 6 (27.3%) who achieved stereopsis of 100 seconds of arc or less. Data from these 6 patients are listed in Table 2. One patient with good binocular function had exotropia, but deviation was intermittent and measured 12PD at distance.
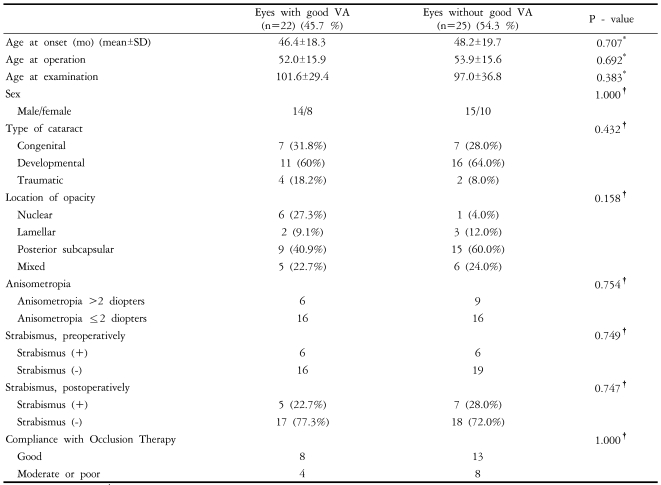
Table 3 compares the characteristics of patients who achieved or did not achieve good visual acuity, with univariate analysis results. Age at onset, cataract type, opacity location, presence of pre- or postoperative strabismus, and occlusion therapy compliance was not different between patients with or without good visual acuity.
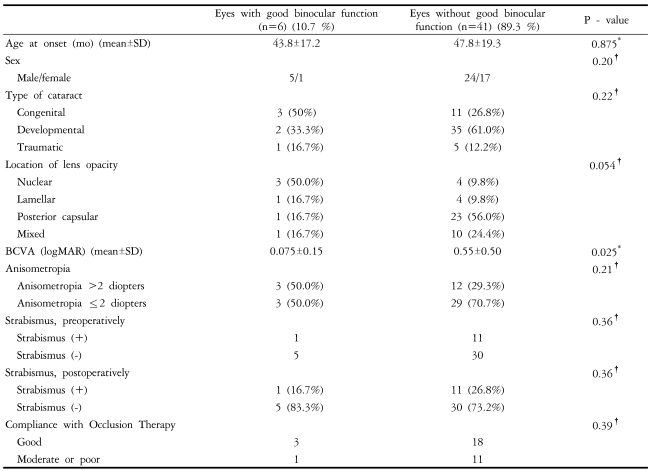
Table 4 compares characteristics of patients with or without good binocular function with univariate analysis results. In eyes with good binocular function, visual acuity was better (p=0.025) compared with eyes without good binocular function. No other variables were significant for achieving good binocular function.
Discussion
Pediatric cataract surgery and aphakia correction after cataract removal presents unique management problems rarely encountered in adult patients. Because of the risk of deprivation amblyopia, cataract surgery in children cannot be delayed once a cataract has developed. With the amblyogenic factor removed, visual development of the operated eye is threatened by anisometropia. Unilateral aphakia correction with glasses produces up to 35% image difference; the use of contact lenses reduces this to 10%. Intraocular lens implantation results in aniseikonia of 0 to 4%.11,12
With cataract surgery evolution and the ability to provide early, effective, and constant optical rehabilitation,13-15 several authors have reported good vision4-6,16,17 and binocular function8,10,18-20 in children with unilateral cataract after surgery.
Our results showed that 46.8% of children with unilateral cataract who underwent removal and PC-IOL implantation between 2 and 6 years of age achieved 20/40 or better visual acuities, which is a prerequisite for good binocular function. However, good binocular function outcome is limited.
There are numerous studies on the relationship between visual acuity and stereopsis. Lee et al.21 reported that as visual acuity improves with occlusion therapy for amblyopia, stereopsis also generally improves. Donzis and associates22 reported that when binocular Snellen visual acuity varies in normal subjects from 20/20 to 20/200, stereopsis changes proportionally. In our study, all children who achieved good binocular function had good visual acuity; other factors were found to be independent.
Autrata et al.23 reported that children treated during their first year of life for unilateral congenital cataracts had improved visual outcomes with primary IOL implantation compared with infants with contact lenses. He suggested that this is because IOLs provide full-time correction of an aphakic eye with optics that closely simulate those of a crystalline lens. Primary IOL implantation provides a stable retinal image with minimal aniseikonia and offers a permanent method of optical correction. Our study focuses on children with unilateral cataract treated between 2 and 6 years of age. A comparison of visual outcome after aphakic correction with primary PC-IOL or with contact lenses is to be investigated further.
The presence of strabismus was reported to be the only contributable factor to good visual acuity and binocular function in a previous study9 but was not significant in our study. Most of our patients with strabismus presented with intermittent small angle strabismus and deviation of 10 to 20 PD, and one had good binocular function.
Our results show that eyes with traumatic cataracts achieved good visual acuity. All 6 patients with traumatic cataract achieved visual acuity of 20/70 or better, and 4 achieved visual acuity of 20/40 or better. However, only 2 achieved good binocular function, which suggests that even a short period of visual deprivation may be sufficient to interrupt binocular vision development if it occurs before visual maturation.
Cataracts associated with posterior lenticonus usually progress slowly. Parks et al.24 demonstrated that cataracts with lamellar opacity and those associated with posterior lentiglobus had the best visual outcomes. Forty-five percent of their patients had 20/40 or better visual acuity. Cheng et al.25 reported similar results, showing that 43.6% of patients with unilateral cataracts associated with posterior lenticonus achieved 20/40 or better visual acuity. Hosal et al.24 reported that 42.1% of posterior lenticonus patients achieved 20/40 or better visual acuity, and 22.1% achieved 100 sec of arc or better stereopsis. Of the 10 patients with posterior lenticonus in our study, 3 patients achieved 20/40 or better visual acuity and 2 achieved good binocular function. Since 0 to 43% of patients with good visual acuity achieved good binocular function in the other cataract group, the probability for patients with good visual acuity to achieve good binocular function is relatively high in the posterior lenticonus group. It is thought that binocularity is more likely to develop in these patients because visual impairment occurs at a later age.
Our study includes only patients with IOL implantation between 2 and 6 years of age. The preferred minimum age for IOL implantation is 2 years for unilateral cataracts, although earlier implantation has recently been attempted. IOL implantation in children younger than 2 may not provide accurate long-term optical correction. Because of myopic shift in refractive error as subjects grow, it is difficult to predict the appropriate lens power required. We still recommend contact lens use in very young children and PC-IOL implantation at approximately 2 years. In addition, our study focuses on the visual function of patients corrected with PC-IOL; we excluded patients with PC-IOL after the age of 6 whose visual function developed mostly without PC-IOL.
This study has several limitations. It was retrospective study, and therefore treatment modality decisions were made by the physician and not randomized. Also, diagnosis was made when parents noticed abnormalities in behavior or appearance, meaning that the precise age of onset for patients in this study may be less accurate than that in a prospective study. Because most patients were diagnosed at preliterate periods, quantitative measurement of visual acuity was unavailable, and preoperative and postoperative visual function association could not analyzed.
In conclusion, our study shows that unilateral cataract removal in a visually immature child can result in a combination of good visual acuity and binocular function. Good binocular function is closely related to good visual acuity.
Notes
The concept of this paper was reported at the 94th annual meeting of the Korean Ophthalmological Society, October 2005.