Evaluation of the Efficacy of Vitrectomy for Persistent Diabetic Macular Edema and Associated Factors Predicting Outcome
Article information
Abstract
Purpose
To evaluate the efficacy of vitrectomy for persistent diabetic macular edema after laser photocoagulation or intravitreal triamcinolone injections and to determine the demographic and ocular factors that influence functional and anatomical outcomes.
Methods
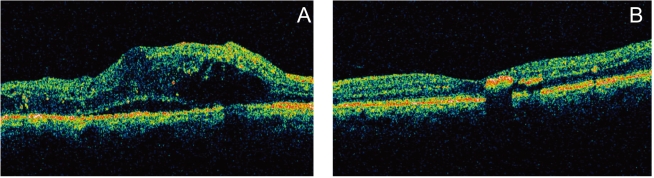
We retrospectively evaluated 55 eyes (51 patients) that had persistent diffuse macular edema after laser photocoagulation or intravitreal triamcinolone injections. We compared preoperative and postoperative best corrected visual acuity and macular thickness by Optical Coherence Tomography and investigated factors including patient's age, presence of vitreomacular traction, grade of diabetic retinopathy, and intraoperative internal limiting membrane removal that may influence the surgical results.
Results
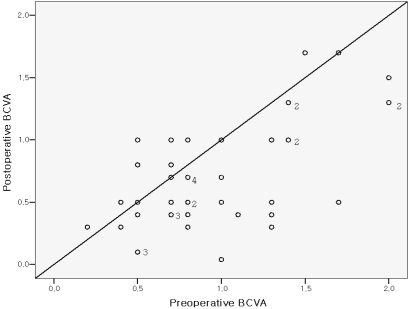
The mean preoperative BCVA (log MAR) was 0.91±0.40 (0.8-1.2). The BCVA improved to 0.72±0.39 (0.3-1.2). The mean preoperative macular thickness was 440±130 (202-805) μm and the mean macular thickness decreased to 306±97 (136-580) μm postoperatively. The eyes showed statistically significant improvement in BCVA and central macular thickness (p<0.001). Preoperative better BCVA was associated with an improved postoperative visual acuity. (p=0.04). No other covariates were found to be statistically significant factors for prognosis of postoperative BCVA.
Conclusions
In eyes with persistent diabetic macular edema after laser or IVTA injections, vitrectomy was effective for decreasing macular thickness and improvement of vision. The visual improvement after vitrectomy was associated with the preoperative better BCVA.
For eyes with long-standing diabetic macular edema (DME) that persists or recurs after laser photocoagulation or intravitreal triamcinolone injection (IVTA), limited treatment benefits are expected. This is because of the structural damage caused by chronic macula edema and the underlying diabetic retinopathy. Several retrospective studies showed that vitrectomy leads to reduction of central macular thickness (CMT) in most cases and improvement of visual acuity in 43-69% of study eyes.1-4 Stolba et al performed a prospective study and reported, that vitrectomy with internal limiting membrane (ILM) peeling was found to be superior to observation alone; in addition, an interaction with therapy time was significant and had a negative impact on vision, confirming a decrease of vision with time in the control group.5 However, there are many opinions regarding the effect of vitrectomies on eyes without vitreomacular traction. Tachi and Ogino reported a positive effect of vitrectomy on macular edema in eyes without any evidence of vitreomacular traction.6 On the other hand, Shah et al reported that the visual benefit of vitrectomy is limited to eyes with signs of macular traction.7 It is important for the surgeon to determine the factors that might influence surgical outcome so that patients are chosen for the procedure that they can get benefit from. Therefore, we made the hypothesis that vitrectomy was effective for decreasing macular thickness and improvement of vision for eyes with persistent DME after laser photocoagulation or IVTA, and evaluated the possible preoperative and intraoperative factors that might influence surgical outcomes.
Materials and Methods
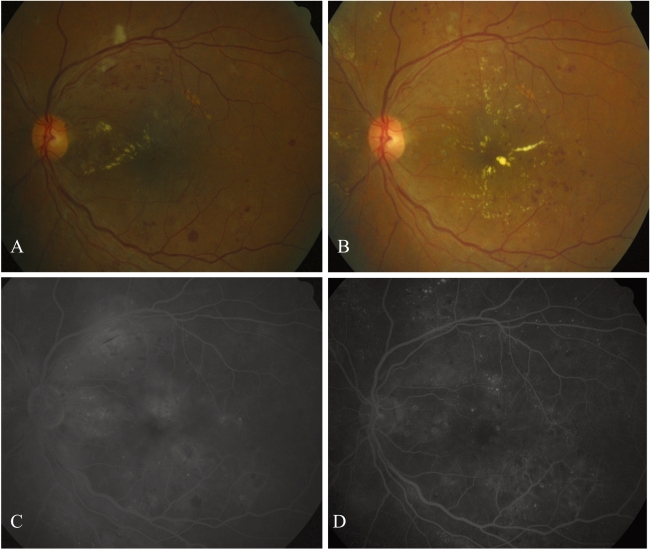
A retrospective nonrandomized study was conducted at 3 hospitals by 3 surgeons between February 2004 and February 2006. Fifty-five eyes (51 patients) with DME that had recurrent or persistent macular edema after laser or intravitreal triamcinolone injections were included in this study. Inclusion criterion was a BCVA of 0.3 or worse in Log MAR units because of recurrent or persistent macular edema secondary to DMR in spite of laser photocoagulation or intravitreal triamcinolone injections. The period of DME since the last laser photocoagulation or intravitreal triamcinolone injections was at least 3 months. Exclusion criteria were significant macular ischemia defined as enlarged perifoveal capillary loss (>1000 μm) by fluorescein angiography, the focal macular edema due to focal leakage from microaneurysm, and other macular pathology such as age related macula degeneration, retinal vascular occlusive diseases, combined optic neuropathy, glaucoma including neovascular glaucoma, vitreous hemorrhage or tractional retinal detachments secondary to diabetic retinopathy. All patients provided written informed consent. All of the patients were followed for at least 6 months with a mean follow-up period of 8.3±7.0 (6-26) months. The BCVA for Snellen chart, lens status, retinopathy stage, and the history of laser photocoagulation and/or IVTA, fundus photography, fluorescein angiography, and OCT (Humphrey model 3000; Humphrey Instruments, San Leandro, CA) were assessed preoperatively and at a mean of 3 month intervals during the follow-up period. OCT was performed six 6 mm radial scans centered at the patient's fixation point at 30 degree intervals. Retinal thickness was computed using the OCT mapping software. The preoperative and postoperative BCVA were converted to log MAR for statistical analysis. An improvement in visual acuity was defined as two or more improved lines of BCVA. All eyes had standard 20 gauze vitrectomy. The paired t-test was used for comparison of preoperative and postoperative visual acuities and central fovea thickness. Multivariate linear regression was performed to evaluate the possible association of age, HbA1C level, preoperative BCVA, preoperative central macular thickness (CMT), phakic status, presence of vitreoretinal traction (presence of epiretinal membrane or taut posterior hyaloid), diabetic retinopathy stage, history of grid laser photocoagulation and IVTA or both, preoperative BCVA, and intraoperative internal limiting membrane removal with a change in postoperative BCVA. To rule out the possible effect of postoperative cataract progression on postoperative BCVA, we compared the results of eyes that were already pseudophakic with eyes that had concomitant cataract surgery.
Results
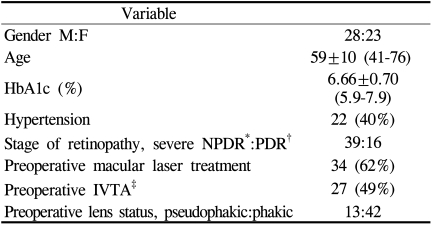
The demographic characteristics of the patients including age, gender, HbA1C level, diabetic retinopathy stage, previous laser or IVTA, presence of systemic hypertension are shown in Table 1.
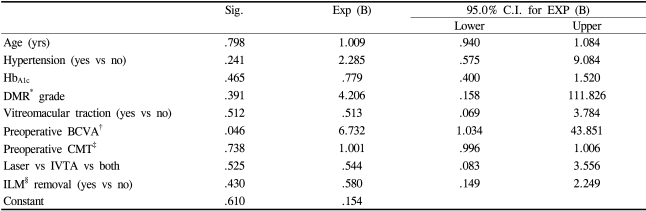
The mean preoperative BCVA (log MAR) was 0.91±0.40 (0.8-1.2). The BCVA improved to 0.72±0.39 (0.3-1.2) postoperatively. The mean postoperative visual acuity was significantly better than the preoperative visual acuity (p<0.001). The improvement of visual acuity was more than two lines in 27 (49%) eyes. The preoperative macular thickness was 440±130 μm (range; 202-805 μm) and the macular thickness significantly decreased to 306±97 μm (range; 136-580 μm) postoperatively (p<0.001). Thirty-four (62%) eyes had concomitant cataract surgery during the vitrectomy procedure. Thirteen eyes (24%) had already undergone cataract surgery before the vitrectomy. Cataract surgery was performed in 3 (5%) eyes during the follow-up period. The numbers of eyes that had laser photocoagulation or IVTA are shown in Table 1. Seventeen (31%) eyes had both laser photocoagulation and IVTA. Two eyes had IVTA twice. Seventeen eyes (31%) had previous pan retinal photocoagulation (PRP). Thirty-two (58%) eyes had vitreomacular traction (presence of epiretinal membrane or taut posterior hyaloid, p=0.512). The internal limiting membrane was peeled in 22 (40%) eyes and indocyanine green (ICG, 0.25%) dye was used in 19 eyes. Intraoperative ILM peeling did not affect the postoperative BCVA (p=0.430). The concomitant cataract surgery with vitrectomy had better postoperative BCVA with marginal statistical significance (p=0.06, paired t test). Better preoperative BCVA was associated with a better postoperative BCVA (p=0.04). No other covariates were found to be statistically significant factors associated with postoperative BCVA improvement (Table 2).
During the follow-up period, deterioration of BCVA was noted in 6 eyes (11%). The causes for deterioration of BCVA were vitreous hemorrhage due to progression of diabetic retinopathy in 2 eyes and persistent macular edema in 4 eyes. Two eyes had increased intraocular pressure which was controlled with topical medications. No eye had complications such as iris neovascularization, retinal detachments during the follow-up period.
Discussion
Diabetic macular edema (DMR) is a major cause of visual loss in diabetic patients.8 The natural history of DME is progressive visual loss with >50% of patients losing more than 2 lines of visual acuity within 2 years.9 The Early Treatment Diabetic Retinopathy Study (ETDRS) showed that laser photocoagulation stabilized vision and reduced the risk of visual loss by 50%.10 But only 3% of patients had improved by three or more lines of vision by the end of study. Recently, improvement of macular edema and visual acuity after intravitreal triamcinolone injections (IVTA) on DME has been reported.11-13
However, laser photocoagulation and IVTA results were not satisfactory in many cases because of common recurrent or persistent macular edema. The efficacy of pars plana vitrectomy (PPV) has been reported for the treatment of diffuse DME with taut posterior hyaloid. Since Lewis et al reported that PPV was effective for treating DME with thickened and taut posterior hyaloid that did not respond to laser treatment, many reports showed that vitrectomy resulted in a decrease of macular edema and improvement of visual acuity.14,15 Although less encouraging results were anticipated due to photoreceptor damage caused by chronic macula edema and the underlying diabetic retinopathy, our study results showed that the mean postoperative BCVA was significantly better than the preoperative BCVA (p<0.001). In addition, more than two lines of BCVA improvement were achieved in 27 (49%) eyes. These findings are consistent with the aforementioned studies and show that vitrectomy can help restore macular structure as well as improve visual acuity for eyes with persistent DME after laser photocoagulation or IVTA. For eyes without taut posterior hyaloid and in eyes with posterior vitreous detachments, the efficacy of vitrectomy is controversial.6,7 Our study showed that the presence of vitreomacular traction (presence of epiretinal membrane or taut posterior hyaloid) did not affect the surgical results (p>0.05). This finding suggests that we can expect a decrease in macular edema and improvement of visual acuity even in the eyes without vitreomacular traction. The correlation of preoperative BCVA and postoperative visual acuity improvement was statistically significant (p=0.04). This fact is implying that preoperative degree of photoreceptor cell dysfunction by chronic macular edema and underlying diabetic retinopathy is important for postoperative visual improvement. And early surgical intervention may be helpful for eyes with chronic DME that persists after laser photocoagulation and IVTA. Another controversial subject is removal of ILM during vitrectomy. Removal of the ILM may have the additional benefit of preventing later epiretinal membrane formation by removing the scaffold for proliferating cells.
Several reports showed that vitrectomy with ILM removal has a better anatomical as well as functional results.15,16 However, for eyes with chronic diffuse DME, there are concerns for further photoreceptor damage in an already damaged macula by removing ILM as well as the possible ICG dye toxicity during the ILM removal.17-19 Yamamoto et al reported that the ILM does not have to be removed to treat eyes with DME.20 Our study showed that ILM removal did not affect either the anatomical or the functional surgical outcomes. Cataract progression after vitrectomy may influence the postoperative BCVA. And our study result showed that eyes with concomitant cataract surgery with vitrectomy had better postoperative BCVA but with marginal statistical significance (p=0.06). This result may have been influenced by the small number of patients studied. Limitations of the present study include relatively small study numbers that may influence the statistical results and lack of a control group. In conclusion, our study provides evidence that vitrectomy can be an effective method to restore macular structure and may improve visual acuity for eyes with persistent DME after laser photocoagulation or IVTA even in eyes without vitreomacular traction. Preoperative BCVA was significantly associated with postoperative visual acuity. An additional positive effect of ILM removal on postoperative BCVA was not significant. A larger prospective case series is needed with longer observation time to further evaluate the effect of vitrectomy on persistent diffuse DME after laser or IVTA.