 |
 |
| Korean J Ophthalmol > Volume 21(2); 2007 > Article |
Abstract
Purpose
To determine the proper time frame in which to assess retinal attachment status and to evaluate the superior retinal attachment status by performing B-scan ultrasonography in different positions on patients who have undergone pars plana vitrectomy and gas tamoponade.
Methods
In this prospective study, 23 patients (23 eyes) who had undergone pars plana vitrectomy and gas tamponade were investigated between June 2005 and February 2006. SF6 (18%) was injected into the vitreous cavity of 15 eyes, and C3F8 (14%) was injected into the vitreous cavity of 8 eyes. At postoperative day 1, day 3, week 1, week 2, and week 4, B-scan ultrasonography was performed in the supine, sitting, prone, right decubitus, and left decubitus positions.
Results
The proper time to evaluate the retinal attachment status was three days post-operatively in 10 eyes (66.7%) with SF6 (18%) injections and two weeks post-operatively in six eyes (75%) that had C3F8 (14%) injections. The superior retinal attachment status can be evaluated from the summation of B-scan ultrasonography results performed in the right decubitus and left ducubitus positions.
Conclusions
The proper time to evaluate the retinal attachment status was related to the degree of the gas absorption when performing B-scan ultrasonography after pars plana vitrectomy and gas tamponade. To evaluate the entire retina, it is useful to perform B-scan ultrasonograhy in the prone, right decubitus and left decubitus positions.
Pars plana vitrectomy and gas tamponade are useful surgical techniques that have been performed to induce the attachment of the retina in various diseases that commonly accompany retinal detachment. However, after such a surgery the pupil becomes smaller due to the posterior synechia of the iris, and some cases develop complications such as hemorrhage from the vitreous body and re-detachment of the retina, so retinal attachment is difficult to evaluate.1-4 Such complications have been reported to occur from 5-10% of cases, and when these complications develop in the eye containing gas, B-scan ultrasonography is a good test method to evaluate the retinal attachment status.5 However, B-scan ultrasonography should be performed when gas is absorbed at a certain degree, and it is not possible in the supine position. Even when the patients are examined in the sitting position the gas floats to the superior area, and therefore the evaluation of the superior peripheral retinal area has been shown to be impossible.6 In our study, B-scan ultrasonography was performed following pars plana vitrectomy and gas tamponade to examine the proper time period for the evaluation of retinal attachment status depending on the gas types used and also to determine the optimal method to examine the attachment condition of the superior peripheral retina. The subjects and methods
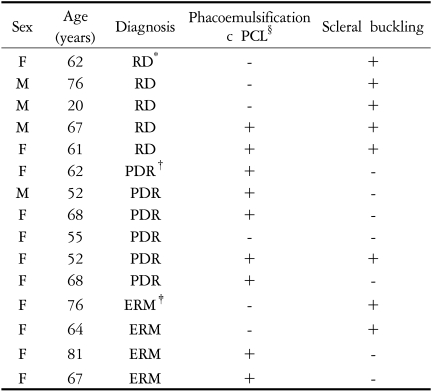
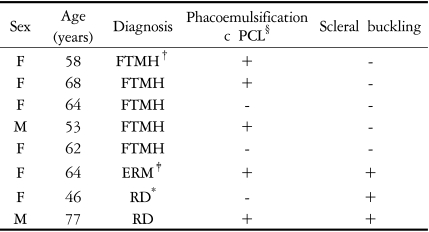
We conducted a prospective study through the examination on 23 patients. Twenty-three eyes received pars plana vitrctomy and gas tamponade from June 2005 through February 2006.
Pars plana vitrectomy and gas tamponade were performed only on cases with proliferative diabetic retinopathy, retinal detachment, macular holes, or severe epiretinal membrane. During surgery under general anesthesia or Subtenon anesthesia, pars plana vitrectomy using three ports was performed, the fluid-air exchange was carried out and gas was injected. Nitrogen gas used for general anesthesia was blocked 15 minutes prior to gas injection. If needed, removal of the epiretinal membrane, intraocular lens implantation and buckling were performed in parallel (Tables 1 and 2).
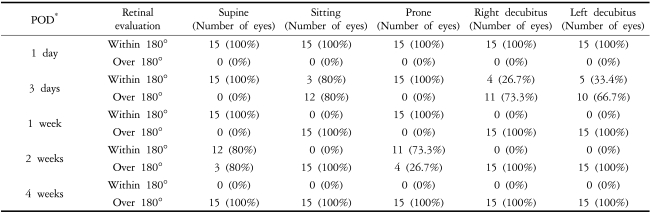
B-scan ultrasonography (A/B scan workstation®, P37, Paradigm, USA) was measured at 80 dB. Follow-ups were performed on day 1, day 3, week 1, week 2 and week 4 after surgery in the supine, prone, right decubitus, and left decubitus positions (Fig. 1). The positions were changed by the patients, and the centerline of the patient was maintained vertically or horizontally based on the horizontal surface. The areas that could be estimated using ultrasound were divided into the two categories of "greater than 180 degrees" and "less than 180 degrees" and then evaluated (Tables 3 and 4). In cases in which the echogenic and low echoic borderlines were more than half of the line connecting the equator of both eyes, the evaluable retina was defined as "greater than 180 degrees", while the cases with less than half of the line connecting the equator of both eyes were defined as "less than 180 degrees."
Among the total 23 cases there were 23 eyes, and males made up 6 of these cases and 6 eyes while females comprised 17 cases and 17 eyes. The mean age was 61.9 years. In 15 eyes, an 18% SF6 intraocular gas tamponade was used, and a 14% C3F8 intraocular gas tamponade was used in the remaining 8 eyes.
On the first day after surgery when gas filled the entire intraocular area, the retinal attachment state could not be evaluated by B-scan ultrasonography regardless of the type of gas or test position used (Fig. 2). In the eyes injected with 18% SF6 and in patients in the supine or prone positions during the B-scan ultrasonographic examination, the retinal attachment state could be evaluated from the third day after surgery onward. Nevertheless, retinal attachment "greater than 180 degrees" could be assessed in 80% (12/15 eyes) of patients in the sitting position, in 73.3% (11/15 eyes) of patients in the right decubitus position, and in 66.7% of patients (10/15 eyes) in the left decubitus position.
In other words, in the eyes injected with 18% SF6 the retinal attachment state could be evaluated in 66.7% of patients (10/15 eyes) when the left decubitus and right decubitus positions were used (Fig. 3). In the eyes injected with 18% SF6, it was still impossible to assess the retina one week after surgery even in patients who were in the supine or prone positions during B-scan ultrasonography. Among the cases in which the "greater than 180 degrees" retinal attachment condition could be assessed, it was evaluated in 100% (15/15 eyes) in the sitting position, 100% (15/15 eyes) in the right decubitus position and 100% (15/15 eyes) in the left decubitus position. One week after surgery in eyes that underwent pars plana vitrectomy and were injected with 18% SF6, the retinal attachment condition could be evaluated in 100% of patients (15/15 eyes) in the sitting position, the right decubitus position or the left decubitus position (Fig. 4).
In the eyes injected with 14% C3F8, the retinal attachment condition could not be evaluated by B-scan ultrasound performed on day 1, day 3 or week 1 after surgery, regardless of the test position used (Fig. 5). In the eyes injected with 14% C3F8, the evaluation of the retina was still impossible even two weeks following surgery in patients who were in the supine or prone position during B-scan ultrasonography. However, the retina in the "greater than 180 degrees" range could be assessed in 87.5% (7/8 eyes) of patients in the sitting position, 75.0% (6/8 eyes) in the right decubitus position and 75.0% (6/8 eyes) in the left decubitus position. In eyes injected with 14% C3F8, the retinal attachment condition could be evaluated in 75% (6/8 eyes) (Fig. 6) of patients at two weeks after surgery when the ultrasound was performed in the sitting position, the right decubitus position or the left decubitus position.
Therefore, in cases where 18% SF6 was used, it was possible to evaluate retinal attachment in 66.7% (10/15 eyes) of patients on the third day postoperatively, and in the cases using 14% C3F8 it was possible in 75% (6/8 eyes) of patients after two weeks had passed since the surgery. The evaluation of the retinal attachment condition by B-scan ultrasonographic testing was not possible in the supine position or the prone position. However, the evaluation of the superior peripheral area was possible in the right decubitus and the left decubitus positions. Therefore, evaluation of the entire retina is possible when B-scan sonography is performed in the sitting position and the right and left decubitus positions.
The half life of gas charged within the eye is a factor that allows retinal attachment after pars planar vitrectomy. Raymond et al7 reported that the half-life of 20% SF6 injected into the eyes of rabbits during vitrectomy and lensectomy was 66 hours. Thompson et al8 found that among cases having 20% SF6 injected after vitrectomy, the half-life of SF6 in the pseudophakic eye was 2.8 days and was 2.4 days in the aphakic eye, while for injected 10% C3F8, the half-life of C3F8 in the phakic eye was 5.7 days, the aphakic eye was 4.5 days, and the pseudophakic eye was 4.3 days. Lincoff et al9 reported that in the pseudophakic eye in which pars planar vitrectomy was not performed, the half-life of 10% C3F8 was 148 hours. In these cases, the half-life in the eyes charged with gas became a marker of the time when pars planar ultrasonography could be performed after surgery. In the eyes that underwent pars planar vitrectomy and gas tamponade, the evaluation of the part of the retina into which the gas was absorbed during pars planar vitrectomy is possible using ultrasonography.
In our study, on the postoperative third day, the "greater than 180 degrees" retinal attachment condition could be evaluated in 66.7% of the eyes which had a pars plana vitrectomy and which were injected with 18% SF6 (10/15 eyes), which was similar to the half-life of 2.8 days reported in previous studies. However, in the eyes injected with 14% C3F8, none of the cases with the "greater than 180 degrees" retinal attachment condition could be evaluated one week after surgery, which was not in agreement with the half-life of five days that had been previously reported.6 It is possible that the cause of such a difference may be because the observation interval was long, ranging from one week to two weeks, and also due to the fact that the concentration of C3F8 used in previous studies was 10% while a concentration of 14% was used in our study. Nevertheless, such points could not explain all the differences of nine days, and comprehensive studies on the half-life of gas may be required.
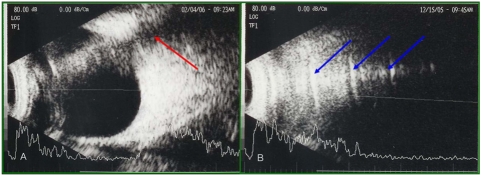
The reflection coefficient is due to the difference of acoustic impedence in the interface of two materials.10 The general reflection coefficient in the intraocular interface is 0.1-7.0%. However, the reflection coefficient of the gas-liquid interface and the gas-tissue interface is 99.9%, regardless of the type of gas.10 Because of this, the image of the posterior area of gas within the eye could not be assessed by B-scan ultrasonography, and the images produced in that area may be considered to be pseudoimages. In our study, when B-scan ultrasonography was performed in the prone position, images were shown to be similar to the retina. However, by differentiating using the points generated from consecutive tests taken one day apart, it was possible to confirm that they were in fact pseudoimages reflecting from the gas-liquid interface, or mirror images. The images also became larger with time and varied depending on the position of the patient (Fig. 7).10 In addition, posterior shadowing11 or reverberation10 could be observed as pseudoimages when gas was present in the eye (Fig. 8).
Since such various pseudoimages appear in the cases using intraocular gas, an experienced eye is best for interpreting B-scan ultrasonography. In addition, depending on the angle of the test equipment or the position of the patients, differing images of the gas-liquid interface were obtained, and therefore methods that can minimize this effect should be selected by recognizing the pseudoimages well.
In the eyes injected with 14% C3F8, a method that can shorten the follow-up interval may be a way to assess the earliest time when the retina can be evaluated using B-scan ultrasonography. In addition, it is necessary to examine the difference between phakic eyes, aphakia, and pseudophakia.
In conclusion, after pars plana vitrectomy and gas tamponade, in cases where a small, fixed pupil is developed by the posterior attachment of the iris or in cases with hemorrhage in the vitreous body, the time when the retinal attachment could be assessed by B-scan ultrasonography in the cases using 14% C3F8 was two weeks after surgery in 75% (6/8 eyes). If intraocular gas were present or if the patient was in the supine or prone positions, the retinal condition could not be assessed. Evaluation of the entire retina was possible using the sitting, right decubitus or the left decubitus positions alone. By reducing pseudoimages developed in the gas-liquid interface at the time the retinal condition is evaluated and keeping in mind the possibility of pseudoimages, B-scan ultrasonography following vitrectomy and gas tamponade by changing the positions of the patient may be useful for the early diagnosis of a retinal attachment condition.
Notes
* This study was presented in part at the 95nd annual metting of the Korean Ophthalmological Society, April 2006.
REFERENCES
1. Susanne S, Katharina K, Andreas W. Incidence of rhegmatogenous retinal detachment after vitrectomy in eyes of diabetic patients. Retina 2006;26:149-152.


2. Han NS, Lee SB, Jo YJ. The results of primary vitrectomy for rhegmatogenous retinal detachment. J Korean Ophthalmol Soc 2006;47:55-61.
3. Ahn JB, Huh K. Clinical analysis of vitrectomy for complication of proliferative diabetic retinopathy. J Korean Ophthalmol Soc 1996;37:1161-1167.
4. Mochizuki Y, Yubota T, Hata Y, et al. Surgical results of combined pars plana vitrectomy, phacoemulsification, and intraocular lens implantation. Eur J Ophthalmol 2006;16:279-286.


5. Treumer F, Bunse A, Rudolf M, Roider J. Pars plana vitrectomy, phacoemulsification and intraocular lens implantation. Comparison of clinical complications in a combined versus two-step surgical approach. Graefes Arch Clin Exp Ophthalmol 2006;244:808-815.


6. Stephen JR, Ronald L, Green , Sandra FB. Diagnostic ophthalmic ultrasound. Retina. 2006. v. 1:4th ed. Baltimore: Elsevier Mosby; chap. 19.
7. Wong Raymond F, Thomson John T. Prediction of the kinetics of disapperance of sulfur hexafluoride and perfluoropropane intraocular gas bubbles. Ophthalmology 1988;95:609-613.


9. Lincoff H, Maise JM, Lincoff A. Intravitreal disappearance rates of four perfluorocarbon gases. Arch Ophthalmol 1984;102:928-929.


10. Whitacre Macr M. B-scan ultrasonograghy of eyes containing intravitreal gas. Am J Ophthalmol 1991;112:272-277.


11. Laing FC. Commonly encountered artifacts in clinical ultrasound. Seminars In Ultrasound 1983;4:27.
Fig. 1
Photographs of B-scan ultrasonography with patients in different positions. (A) Supine position. (B) Sitting position. (C) Prone position. (D) Right decubitus position. (E) Left decubitus position.

Fig. 2
On postoperative day 1, the results of B-scan ultrasonography while patients assumed different positions on eyes undergoing vitrectomy and an 18% SF6 gas tamponade. (A) Supine position: can not evaluate the retinal attachment status. (B) Sitting position: can not evaluate the retinal attachment status. (C) Prone position: can not evaluate the retinal attachment status. (D) Right decubitus position: can not evaluate the retinal attachment status. (E) Left decubitus position: can not evaluate the retinal attachment status.
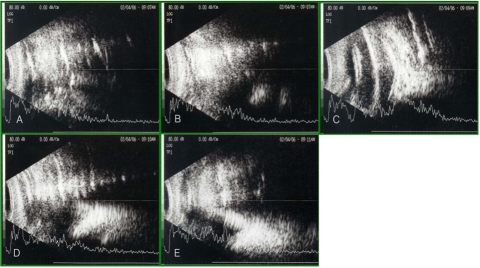
Fig. 3
On postoperative day 3, the results of B-scan ultrasonography taken with patients in different positions on the eyes undergoing vitrectomy and an 18% SF6 gas tamponade. (A) Supine position: can not evaluate the retinal attachment status. (B) Sitting position: can evaluate the retinal attachment status greater than 180°. (C) Prone position: can not evaluate the retinal attachment status. (D) Right decubitus position: can evaluate the retinal attachment status greater than 180°. (E) Left decubitus position: can evaluate the retinal attachment status less than 180°.
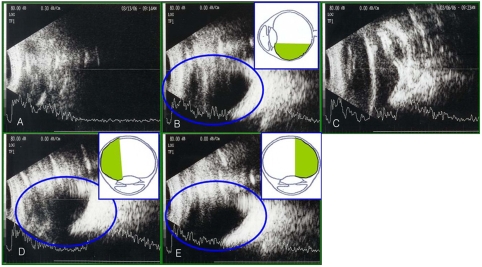
Fig. 4
On postoperative day 7, results of B-scan ultrasonography with the patients in different positions of the eyes undergoing vitrectomy and an 18% SF6 gas tamponade. (A) Supine position: can not evaluate the retinal attachment status. (B) Sitting position: can evaluate the retinal attachment status greater than 180°. (C) Prone position: can not evaluate the retinal attachment status. (D) Right decubitus position: can evaluate the retinal attachment status greater than 180°. (E) Left decubitus position: can evaluate the retinal attachment status greater than 180°.
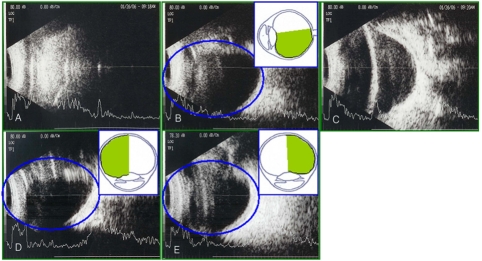
Fig. 5
At postoperative week 1, results of B-scan ultrasonography with patients in different positions on the eyes undergoing vitrectomy and using a 14% C3F8 gas tamponade. (A) Supine position: can not evaluate the retinal attachment status. (B) Sitting position: can not evaluate the retinal attachment status. (C) Prone position: can not evaluate the retinal attachment status. (D) Right decubitus position: can not evaluate the retinal attachment status. (E) Left decubitus position: can not evaluate the retinal attachment status.
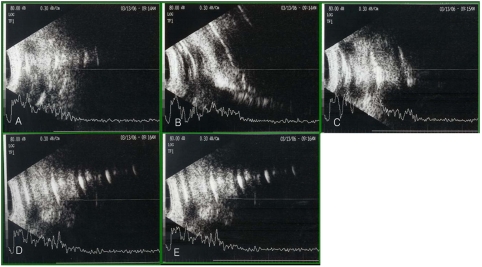
Fig. 6
At two weeks postoperatively, results of B-scan ultrasonography with patients assuming different positions on the eyes undergoing vitrectomy and using a 14% C3F8 gas tamponade. (A) Supine position: can not evaluate the retinal attachment status. (B) Sitting position: can evaluate the retinal attachment status greater than 180°. (C) Prone position: can not the retinal attachment status. (D) Right decubitus position: can evaluate the retinal attachment status greater than 180°. (E) Left decubitus position: can evaluate the retinal attachment status greater than 180°.
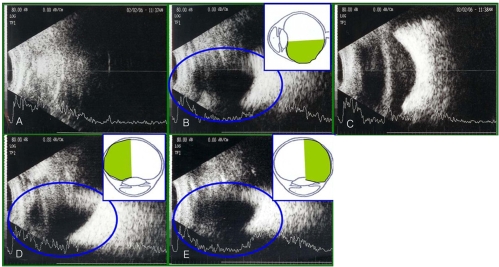
Fig. 7
Results of B-scan ultrasonography with the patient in the prone position on the eyes undergoing vitrectomy and using an 18% SF6 gas tamponade. (A) At postoperative day 1, (B) on postoperative day 2, (C) at postoperative day 3, (D) on postoperative day 4, (E) at postoperative day 5, (F) on postoperative day 6, (G) at postoperative day 10, (H) on postoperative day 11: the echogenic image that we thought was the retina proved to be the gas-fluid interface because this echogenic image has moved to the posterior pole from day to day.
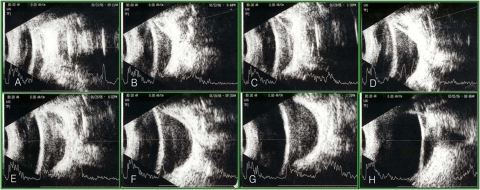
Fig. 8
The false images on B-scan ultrasonography on the eyes filled with gas. (A) Posterior shadowing (red arrow). (B) Multiple reverberations (blue arrows).
- TOOLS




 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print




