Dacryocystitis is an acute or chronic inflammatory condition that is caused by an obstruction of the nasolacrimal duct that induces the stagnation of tears in the lacrimal sac. Acute dacryocystitis is heralded by sudden onset of redness, swelling, and pain in the medial canthal region, and it can produce pus in the lacrimal sac or fistula on the skin. On the other hand, chronic dacryocystitis has an insidious onset of epiphora, recurrent conjunctivitis, and a mucoid pus-like discharge when digital pressure is placed on the lacrimal sac or when the irrigation of the lacrimal sac is carried into the lacrimal punctum.1,2 The pathophysiology of these inflammatory conditions is as follows: congenital narrowing or obstruction of the lacrimal excretory system, inflammation or trauma around the lacrimal sac, a mass lesion in the nose or nasal cavity, etc. The treatment includes systemic antibiotic therapy in the acute stage and subsequent surgical drainage and dacryocystorhinostomy.3-5
A silastic sheet is made from a Dacron mesh that is added to silicone, and has been used in the surgical sections for various purposes including reconstructions after trauma.6-10
The authors report the case of a silastic sheet that was found during an endoscopic transnasal dacryocystorhinostomy to treat acute dacryocystitis with necrosis of the lacrimal sac.
Case Report
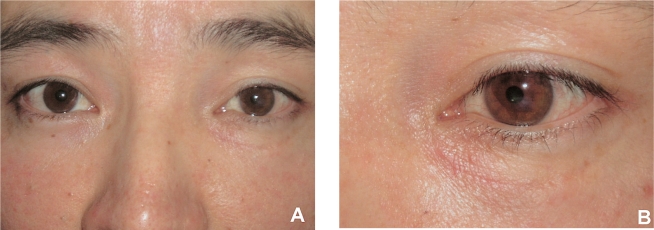
A thirty-two year old male presented with painful swelling on the nasal side of his left lower lid and complained medial canthal swelling, tenderness, chemosis, and epiphora. Oral antibiotics administered in another hospital did not relieve these symptoms. He was involved in a traffic accident fourteen years ago and at that time suffered from a left side facial bone fracture and left sided visual disturbance as a result of a choroidal rupture in his left eye. The patient underwent surgery to reconstruct the ethmoidal sinus. At the time of the initial visit, his uncorrected visual acuity was 20/20 in the right eye and counting fingers 10 cm from his left eye. The left lower lid showed severe erythematous swelling, particularly around the medial canthus, and there was a moderate degree of conjunctival injection and chemosis (Fig. 1). A complete blood count, urinalysis, and simple chest X-ray were within the normal limits. However, regurgitation of the purulent discharge from the lower lacrimal punctum upon lacrimal sac massage was observed. Accordingly, the patient was diagnosed with acute dacryocystitis and a bacterial culture examination was carried out. An endoscopic transnasal dacryocystorhinostomy was performed the next day.
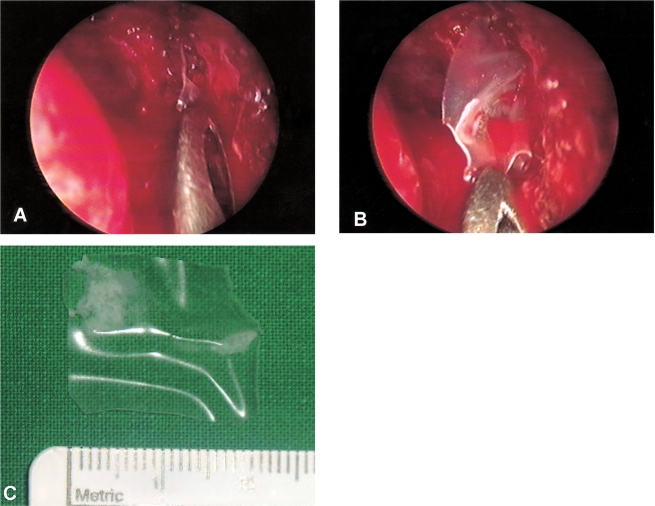
Surgery was performed under the general anesthesia and endotracheal intubation was held at the 45° position. Packing gauze soaked with a mixture of epinephrine and 2% lidocaine at a ratio of 1:100,000 was inserted one hour before the surgery, which was removed at the time of the surgery. A 20-gauge illuminator for the vitreoretinal surgery was placed into the lacrimal sac via the lacrimal punctum so an overview of the lacrimal sac and surrounding structure could be obtained. An electrocautery device tipped with a Colorado needle was used to cauterize and ablate the nasal mucosa, while a Freer elevator was used to expose the maxillonasal suture and adjacent bony structure. An osteotomy was made principally using a Kerrison punch and a microdrill. The surgical finding showed severe necrosis around the lacrimal sac and a 20×15-mm sized silastic sheet crumpled within the purulent discharge (Fig. 2). The sheet was removed, the lacrimal sac irrigated with an antibiotic solution (Gentamicin 80 mg/2 ml), and the medial half of the lacrimal sac was excised using a sickle knife and upward Blakesley forceps. Subsequently, gauze soaked with mitomycin C 0.4 mg/ml was placed into the osteotomy site for approximately two minutes and removed. The area was then irrigated with normal saline. A silastic tube (FCI bicanalicular intubation set®, France Chirurge instrumentation, France) with a 0.8-mm outer gauze was applied into the lacrimal pathway from the upper and lower punctum to the nasal cavity, which was then sutured with 4-0 nylon and positioned in the nasal cavity. A polyvinyl resin (Merocel®) pasted with antibiotic ointment was packed into the nasal cavity in order to prevent nasal bleeding, and to maintain the patency of the lacrimal sac opening.
One day after surgery, the silicone tube was positioned at the medial canthus. The painful swelling around the medial canthal area of the left lower lid was slightly decreased, and no pus-like discharge was found upon lacrimal sac massage. The patient was discharged with a prescription of topical antibiotics, steroid, oral antibiotics, and non-steroidal anti-inflammatory agent, and was followed up at the outpatient department. The painful swelling on the nasal side of his left lower lid resolved gradually, and there were no symptomatic complications after removing the silicone tube three months later (Fig. 3).
Discussion
The lacrimal excretory system is prone to infection and inflammation for many reasons. This mucus membrane-lined tract is contiguous with two surfaces (conjunctival and nasal mucosal) that are normally colonized with bacteria. The functional purpose of the lacrimal excretory system is to drain tears from the eye into the nasal cavity. The stagnation of tears in a pathologically closed lacrimal drainage system can result in dacryocystitis. Acquired dacryocystitis can be either acute or chronic. Acute dacryocystitis is heralded by a sudden onset of pain and redness in the medial canthal region. An insidious onset of epiphora is characteristic of chronic inflammation or an infection of the lacrimal sac.2
The prevalence of acute dacryocystitis is highest after middle age, particularly the fifth decade of life. Manifestation is usually an acute attack of a chronic inflammatory condition of the lacrimal sac. The main causative microbial organism is Staphylococcus and Streptococcus, and rarely gram-negative bacteria and fungus, respectively. Generally, the causative organism is mainly pathogenic bacteria in the upper respiratory tract and among these, Staphylococcus aureus is the most common in acute dacryocystitis followed by β-hemolytic streptococcus. It is known that chronic dacryocystitis is mainly the result of Streptococcus pneumoniae, but Candida ablicans is the cause in rare cases.3-5,11-15 Uncommonly in adult patients, there is a cystic lesion such as a nasal polyp or tumor in the nasal cavity around the end of the nasolacrimal duct or a secondary obstruction of the nasolacrimal duct, after an ocular trauma precipitates chronic dacryocystitis.
Dacryocystitis due to an exogenous foreign body has been previously reported. Felt and Frueh reported a case where a small BB bullet found on a dacryocystogram played the role of a check valve in lacrimal sac and interrupted the lacrimal drainage causing chronic dacryocystitis.16
Thus far, people have tried various modalities in the treatment of acute dacryocystitis. Cahill and Burns17,18 reported pain relief within 48 hrs and infection control after an incision and drainage through the skin followed by an injection of antibiotics and irrigation in acute dacryocystitis patients. Moreover, a transcutaneous external dacryocystorhinostomy was performed within a month of this treatment, and no serious complications were encountered. However, an external dacryocystorhinostomy in the acute stage can cause preseptal or orbital cellulitis and sepsis, and a delay until the infection is controlled can cause patients some discomfort. For this reason, some people were recommended to undergo an early dacryocystorhinostomy. However, it is universally accepted that a dacryocystorhinostomy cannot be performed when pus forms after antibiotic therapy, until warm massage and pus drainage are performed, and inflammation thereby subsides.
A silastic (silicone elastomer: Polydimethyl Siloxane, Dow Corning Ltd, Midland, MI) sheet is silicone that is strengthened with a Dacron mesh, and has tensile strength and elasticity over a relatively large area. Surgeons have used it widely to reconstruct a defects in bone, cartilage, and connective tissue after trauma, inflammation, and tumor. The following are examples of its applications: reconstruction of the temporomandibular joint,19 pharynx and larynx,20 the dissociation of fingers in the syndactyly,21 emergent hemostasis in the surgery for a cerebral aneurysm,22 the closing of a defect in a diaphragmatic herniation,23 and a reconstruction of the orbital wall in a blowout fracture.6,8,10
However, several complications of the silastic sheet have been reported. These include the formation of excessive collagen connective tissue or cysts7,8,24 and an increase in infection as a result of increased bacterial adhesion.9 In addition, displacement and migration, as in our case, has also been reported. Groombridge and McGuinness reported a case where a silastic sheet used to reconstruct the orbital wall was displaced into the nasal cavity.25
The lateral wall of the ethmoid sinus, i.e. the Lamina papyracea, is a thin paper-like bone plate which constitutes the medial aspects of the orbit and the medial wall of the ethmoid sinus. The lamina papyracea is also a lateral wall of the nasal cavity and a sticking area of the middle nasal concha. The cribriform plate connects one group of ethmoid air cells to another.26 In a severe nasoethmoidal fracture, a silastic sheet is sometimes used endonasally with wiring to support a fracture site and nasal packing is achieved with Merocel®, which is maintained for several weeks.27 When the nasal packing is removed or when anatomical stability is not sufficiently achieved, the silastic sheet can be displaced into the adjacent nasal cavity or toward the medial wall of the orbit.
In this case, the silastic sheet was found adjacent to the lacrimal sac during endoscopic transnasal dacryocystorhinostomy to treat acute dacryocystitis. The authors do not know if the silastic sheet was the direct cause of the acute dacryocystitis, but it is possible that the silastic sheet used in the previous ethmoidal sinus reconstruction had migrated to the perimeter of the lacrimal sac and induced the chronic inflammation around the lacrimal sac. These conditions precipitated the acute purulent inflammation of the lacrimal sac. However, further investigation will be needed to determine the mechanism in this case.
It was reported that a narrowing or occlusion of the nasolacrimal duct is the most common cause of acute dacryocystitis. We report the first case where a silastic sheet applied during a facial reconstruction had migrated adjacent to the lacrimal sac resulting in severe inflammation.




 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print






