Arteriovenous Sheathotomy for Persistent Macular Edema in Branch Retinal Vein Occlusion
Article information
Abstract
Purpose
To evaluate the efficacy of arteriovenous (AV) sheathotomy with internal limiting membrane peeling for persistent or recurrent macular edema after intravitreal triamcinolone injection and/or laser photocoagulation in branch retinal vein occlusion.
Methods
Twenty-two eyes with branch retinal vein occlusion (BRVO) with recurrent macular edema underwent vitrectomy with AV sheathotomy and internal limiting membrane peeling. All eyes had previous intravitreal triamcinolone injection and/or laser photocoagulation for macular edema. The best corrected visual acuity (BCVA), fluorescein angiography and optical coherence tomography (OCT) before and after surgery were compared.
Results
The mean preoperative BCVA (log MAR) were 0.79±0.29 and postoperative BCVA (log MAR) at 3 months was 0.57±0.33. And improvement of visual acuity ≥2 lines was observed in 10 eyes (45%). The mean preoperative fovea thickness measured by OCT was 595.22±76.83 µm (510-737 µm) and postoperative fovea thickness was 217.60±47.33 µm (164-285 µm).
Conclusions
Vitrectomy with AV sheathotomy can be one treatment option for the patients with recurrent macular edema in BRVO.
Branch retinal vein occlusion is the second most common cause of retinal vascular disease after diabetic retinopathy.1,2 Many patients with BRVO experience a decrease in visual acuity because of macular edema, retinal ischemia or hemorrhage.2 The Branch Retinal Vein Occlusion Study demonstrated that eyes treated with argon laser photocoagulation for macular edema gained a mean improvement of visual acuity of 1.3 lines whereas the control group gained 0.2 lines.2 Recently, improvement in macular edema and visual acuity after intravitreal triamcinolone injections on macular edema in BRVO have been reported.3 However, these therapeutic results were not satisfactory in many cases because recurrent or persistent macular edema is common even after laser photocoagulation or intravitreal triamcinolone injections.4
After the first report by Osterloh and Chales in 1988, several investigators reported significant improvement of macular edema and visual acuity after arteriovenous sheathotomy for decompression of macular edema in BRVO.5-9 This surgical approach is based on the fact that BRVO takes place at the site of arteriovenous crossing where the artery and the vein shared a common vascular adventitia. Although the exact mechanism responsible for the improvement of visual acuity after vitrectomy and arteriovenous sheathotomy is still not clear, Mason et al reported that surgery halved the visual angle in 75% of patients compared with 40% of the control group.10 Charbonnel et al also reported visual acuity improvement of two ETDRS lines or more in 69% of patients with a mean gain of 1.9 ETDRS lines.11 However, most of these results are in eyes with relatively short BRVO duration and excluded the eyes with recurrent or persistent macular edema in BRVO after laser or intravitreal triamcinolone injections.
The purpose of this study is to investigate the anatomic and functional results after arteriovenous sheathotomy with ILM peeling for persistent or recurrent macular edema in BRVO.
Materials and Methods
A retrospective, nonrandomized study was conducted in 22 eyes (22 patients) with BRVO and recurrent or persistent macular edema after laser or intravitreal triamcinolone injections. Inclusion criteria were BCVA of 0.3 or worse in log MAR unit as result of recurrent or persistent macular edema or hemorrhages secondary to BRVO in spite of laser photocoagulation or intravitreal triamcinolone injections. Exclusion criteria were the presence of other retinal vascular diseases, marked macular ischemia, vitreous hemorrhage or retinal neovascularization secondary to BRVO. The duration of symptoms was not used for the exclusion criteria. All patients provided written informed consent. The BCVA in logMAR units using the Snellen chart, indirect ophthalmoscopic and slit-lamp examination, fundus photography, fluorescein angiography, and central fovea thickness by OCT (Humphrey model 3000; Humphrey Instruments, San Leandro, CA) was checked preoperatively and postoperative mean 3 months. The improvement of visual acuity was defined as 2 lines or more of improvement of BCVA (Snellen visual acuity).
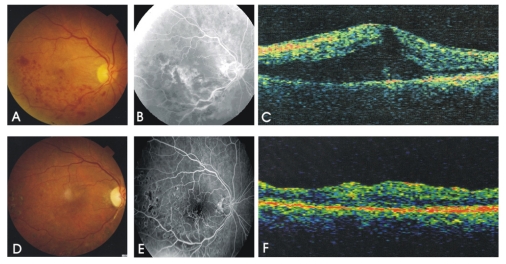
All surgeries were performed by one author (S.J.). Standard pars plana vitrectomy was performed and followed by removal of posterior hyaloid membrane. The involved AV crossing site was identified and the common AV crossing sheath was incised by a BRVO knife (Synergetics, USA). The completion of AV dissection was confirmed by the elevation of the overlying vessels. But, in cases having very slender and sclerotic thread like overlying vessels, complete A-V separation was not performed obsessively not to cut the vessel. The internal limiting membrane (ILM) in the macular area was removed using ILM forceps (Eckardt end-gripping foceps, D.O.R.C) without triamcinolone or indocyanine green dye staining. Laser photocoagulation was done on the ischemic retina in cases of large ischemic area. Simultaneous phacoemulsification and aspiration of cataracts with intraocular lens implantation was performed in 10 eyes (45%).
The preoperative BCVA, preoperative central foveal thickness, duration of symptoms, patient's age and sex, associated systemic illness such as hypertension were evaluated.
Results
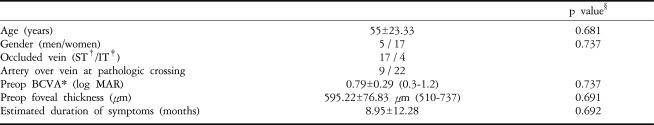
Baseline demographics of the recruited patients are given in Table 1. There was no significant intraoperative or postoperative retinal bleeding, retinal tear, or detachments.
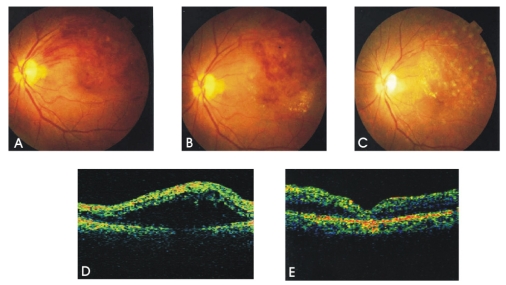
The mean preoperative BCVA (log MAR) was 0.79±0.29 (0.3-1.2) and postoperative BCVA (log MAR) was 0.57±0.33 (0.05-1.2). Postoperative BCVA was significantly better than preoperative BCVA (p<0.01, Fig. 1). The mean duration of symptoms before treatment (laser or IVTA) was 8.95±12.28 months. The interval between the recurrence of macular edema after IVTA or laser treatment and surgery was 3.05±2.08 months. All eyes did not have PVD before the surgery.
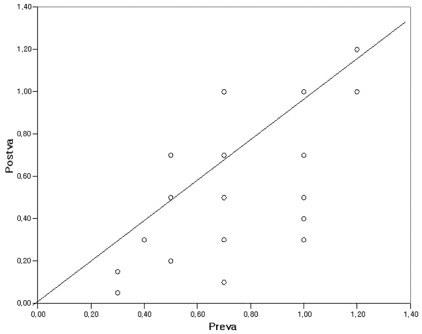
The relationship between the preoperative visual acuity and postoperative visual acuity. The improvement of visual acuity is statistically significant (p<0.01, Chi squared test).
Preva: preoperative visual acuity (log MAR), Postva: postoperative visual acuity (log MAR)
Ten eyes (45%) had more than 2 lines of improvement of visual acuity and 4 eyes (18%) had more than 4 lines of visual improvement. Visual acuity remained stable during 13.53±4.18 months (9-22 months) of follow up period thereafter. Two eyes (9%) had decreased visual acuity because of persistent macular edema. The mean preoperative central fovea thickness measured by OCT was 595.22±76.83 µm (510-737 µm) and postoperative fovea thickness was 217.60±47.33 µm (164-285 µm). At obstruction site, the vein crossed over the artery in 12 eyes (54%). In twenty (91%) eyes, the tertiary branch retinal vein was responsible for the pathologic crossing. Restoration of blood flow, intraoperative reestablishment of a red column of erythrocytes through the previously closed vessel, was identified in all cases having overlying arteries at obstruction site, but not in cases having sclerotic thread-like overlying veins. Three eyes (14%) had phacoemulsification and aspiration of cataracts with intraocular lens implantation during follow up period. Cataract surgery did not influence the postoperative improvement of visual acuity (partial correlation, p=0.627). None of the expected factors such as preoperative BCVA, preoperative foveal thickness, duration of symptoms, patient's age and sex had a significant effect on postoperative visual improvement (Table 1).
Discussion
Branch retinal vein occlusion is a common retinal vascular disorder. The interruption of venous flow in these eyes almost always occurs at a retinal arteriovenous intersection, where a retinal artery crosses a retinal vein.12 The thickened artery compresses the vein, which starts the cascade of turbulence of blood flow, endothelial damage, and thrombosis in the vein.12 The natural history of BRVO is known to be favorable, and 53% of patients achieve final visual acuity of 20/40 or better.13 Intraretinal hemorrhage, macular edema, and capillary nonperfusion may be the cause in cases with poor visual acuity.13 The BRVO Study showed significant improvement of visual acuity 3 years after grid laser treatment, with an average visual acuity of 20/40 to 20/50 in the treated group and 20/70 in the control group.13 But the BRVO study did not include cases of foveal hemorrhage or ischemia, or cases of persistent macular edema after grid laser photocoagulation, which are the majority of BRVO-associated morbidities. Various medical and surgical treatments have been tried to treat complications of BRVO. Ozkiris and Evereklioglu reported that intravitreal injection of corticosteroid for macular edema in BRVO resulted in significant improvement in visual acuity, from baseline of 0.98±0.19 to a maximum of 0.24±0.24 logMAR during a mean follow-up period of 6.3 months.14,15 However, the monotherapy of corticosteroid intravitreal injection cannot prevent recurrent macular edema.4 Pars plana vitrectomy with removal of posterior cortical vitreous can improve oxygen supply to the ischemic inner retina by enhancing fluid currents in the vitreous cavity. The resolution of retinal hypoxia might suppress retinal neovascularization and thus reduce macular edema.16
Since the first report by Osterloh and Chales, many authors have reported the improvement of macular edema and visual acuity by vitrectomy with AV sheathotomy in BRVO.17 Charbonnel et al11 reported that improvement of visual acuity was more frequent in eyes with removal of ILM and without PVD. The exact role of AV sheathtotomy and timing of surgery in BRVO are still controversial. Yamamoto et al18 reported AV sheathotomy and PVD significantly reduced macular edema, but there was no significant difference in macular function following either procedure. However, Lakhanpal et al19 reported that AV sheathotomy without vitrectomy can improve macular edema and hemorrhage and also improve visual acuity. Many authors advocate that early surgery may be associated with better anatomical and functional outcomes.10,20 Although we expected a lower rate of improvement of macular edema and visual acuity in this study, because of the chronic nature of the study candidates and possibility of long standing subretinal fluid causing RPE damages, there was improvement of visual acuity in 16 eyes in 22 eyes (75%), which was similar results with previous results.10,11 This result may be in part coincidence with the vitrectomy and surgical PVD may playing a more important role than AV sheathotomy, and postoperative visual acuity improvement may be due to the reduction of macular edema and not to a better blood flow in occluded territory itself. But the effect of AV sheathotomy cannot be ruled out because we did not compare eyes with and without AV sheathtotomy and did not consider an additional effect of ILM removal on macular edema resolution.21 Another interesting finding in our study was at pathologic AV crossing site, vein crossed anterior to the artery in 12 eyes (54.5%). This finding is opposite to previous reports that most of pathologic AV crossing in BRVO occurs where the artery is anterior to the vein.14,21 Considering that our study patients had persistent or recurrent macular edema and hemorrhage despite the treatment, vein-overcrossing BRVO may be more associated with poor response to laser or corticosteroid intravitreal injection more than artery over-crossing BRVO. In these cases, dual compression outside from the underlying artery and inside from intraocular pressure might cause more severe and refractory venous obstructions. But this finding needs more evaluation in a larger clinical observation. No complications have been observed in our study except for cataract progression in 3 eyes (14%). This study has several limitations. Patients were not randomly assigned to the treatments group, there was no control group, and the possible additional effect of the ILM removal on macular edema resolution was not investigated.
In conclusion, this study showed a favorable effect of vitrectomy and AV sheathotomy in eyes with persistent or recurrent macular edema after laser photocoagulation and/or corticosteroid intravitreal injection and vitrectomy with AV sheathotomy can be one treatment option for the patients with recurrent macular edema in BRVO.
Notes
All authors have no financial interest in this subject.
The study and data accumulation were in conformity with all country laws