 |
 |
| Korean J Ophthalmol > Volume 20(3); 2006 > Article |
Abstract
Purpose
We wanted to examine the effect of graded recession and anteriorization of the inferior oblique muscle on patients suffering from unilateral superior oblique palsy.
Methods
Inferior oblique muscle graded recession and anteriorization were performed on twenty-two patients (22 eyes) with unilateral superior oblique palsy. The recession and anteriorization were matched to the degree of inferior oblique overaction and hypertropia. The inferior oblique muscle was attached 4 mm posterior to the temporal border of the inferior rectus muscle in six eyes, 3 mm posterior in five eyes, 2 mm posterior in five eyes, 1 mm posterior in five eyes, and parallel to the temporal border in one eye.
Results
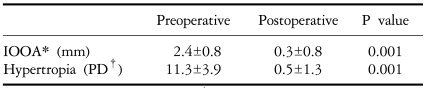
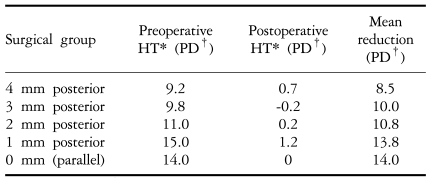
The average angle of vertical deviation prior to surgery was 11.3┬▒3.9 prism diopters (PD). The total average correction in the angle of vertical deviation after surgery was 10.8┬▒3.8 PD. In the parallel group, the average reduction was 14 PD. After surgery, normal inferior oblique muscle action was seen in eighteen of twenty-two eyes (81.8%).
The incidence of superior oblique palsy has been reported to be relatively high in patients with extraocular muscle palsy. von Noorden et al1 reported it to be the most common paralytic strabismus. The causalities of superior oblique palsy are mostly congenital and traumatic but may also be idiopathic, or develop in association with tumor, vascular ischemia, diabetes mellitus, hypertension, or other vascular diseases.2-5 Parks three-step test6 is used to diagnose superior oblique palsy, based on hypertropia in the paralyzed eye, increased vertical deviation upon adduction, and increased vertical deviation upon head tilt to the ipsilateral side. The symptoms of superior oblique palsy include vertical diplopia, cyclodiplopia, and head tilt.
Surgeries for concomitant inferior oblique muscle (the antagonist muscle to superior oblique palsy) overaction include myotomy, myectomy, recession,7 anterior transposition,8 and disinsertion9 of the inferior oblique muscle. Guemes and Wright10 recently reported on a surgical anterior transposition of the inferior oblique muscle to the inferior rectus muscle insertion site. The transposition varies according to the degree of inferior oblique overaction.
Therefore, we performed a graded recession and anteriorization of the inferior oblique muscle in patients with unilateral superior oblique palsy and concomitant inferior oblique overaction. We also examined the amount of correction related to hypertropia and inferior oblique overaction.
Between August 1996 and April 2005, we retrospectively analyzed twenty-two patients with twenty-two unilaterally affected eyes that were diagnosed with unilateral superior oblique palsy and concomitant hypertropia and inferior oblique overaction. These patients were seen in the Department of Ophthalmology at our hospital. Seventeen patients were male, and five were female, with a mean age of seven years (range: 2-22 years). The follow-up period varied between three and forty-six months, although the average was twelve months. In concomitant horizontal strabismus cases, ten patients had exotropia and five had esotropia. Cases that underwent simultaneous vertical muscle surgery were excluded from the study population.
Superior oblique palsy was diagnosed by the Parks three-step test6 and the fundus examination. In order to measure the vertical deviation, the prism cover test was performed at the primary position, 1/3 m and 5 m. The up, down, right, and left gazes of deviation were measured at 5 m.
The severity of the inferior oblique overaction before and after surgery was graded. This was done by recording the difference between the corneal limbus height in each eye, according to the degree of over-elevation of the eye in adduction. The over-elevation scale ranged from 0 to +4. Two eyes had 1-5 prism diopters (PD) preoperative hypertropia, eight had 6-10 PD, nine had 11-15 PD, and three had 16-20 PD (average: 11.3 PD). Three eyes had inferior oblique overaction of +1, six eyes were +2, four were +2.5, eight were +3 and one eye was +4. Seven eyes had a head tilt to the right, and twelve eyes had a head tilt to the left. In three cases, the head tilt was less than 5┬░.
A single surgeon performed the surgeries for all twenty-two patients, using an identical method. The inferior oblique muscle was attached to the sclera 4 mm posterior to the temporal border of inferior rectus muscle in six cases (inferior oblique overaction is +1 or hypertropia is less than 6 PD), 3 mm posterior in five eyes (inferior oblique overaction between +2 and +2.5 or hypertropia beween 6 and 10 PD), 2 mm posterior in five eyes (inferior oblique overaction is +3 or hypertropia between 11 and 15 PD), 1 mm posterior in five eyes (inferior oblique overaction is +3 or hypertropia is more than 15 PD), and parallel to the temporal border of inferior rectus muscle in one eye (inferior oblique overaction is +4 or hypertropia is more than 15 PD) (Table 1). If inferior oblique overaction was +3, we reattached 1 mm when hypertropia was more than 15 PD and 2 mm posterior when hypertropia was less than 15 PD. If hypertropia was more than 15 PD and inferior oblique overaction was +3, we reattached 1 mm posterior. When inferior oblique overaction was +4, we reattached parallel to the temporal border of the inferior rectus muscle. In most cases, we followed the above standards.
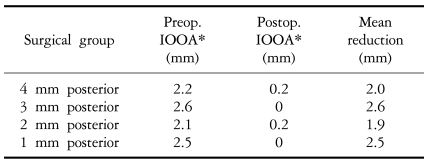
In twenty-two patients, the average preoperative angle of vertical deviation was 11.3┬▒3.9 PD, and the average severity of inferior oblique muscle overaction was 2.4┬▒0.8 mm. The average postoperative follow-up period was twelve months. At the last follow-up examination, the average angle of vertical deviation at the primary position was 0.5┬▒1.3 PD (Table 2). The mean reduction in the angle of vertical deviation at the primary position was 8.5 PD in the 4 mm group, 10.0 PD in the 3 mm group, 10.8 PD in the 2 mm group, 13.8 PD in the 1 mm group, and 14 PD in the parallel group (Table 3). Eighteen of twenty-two eyes (81.8%) showed normal inferior oblique muscle action; the 4 mm group decreased in activity from an average of 2.2 to 0.2, the 3 mm group decreased from an average of 2.6 to 0, the 2 mm group decreased from an average of 2.1 to 0.2, and the 1 mm group decreased from an average of 2.5 to 0 (Table 4).
After surgery, no cases of hypertropia at the primary position or upgaze limitation were seen. One eye from the parallel group and one from the 1 mm group developed inferior oblique overaction in the opposite eye. One eye in the 2 mm group and one in the 3 mm group developed hypertropia of less than 4 PD in the opposite eye. After surgery, mild residual hypertropia was detected in six eyes, all of less than 4 PD. Prior to surgery, head tilt away from the paralyzed eye was detected in nineteen patients. This condition improved or disappeared in eighteen of these patients (94.7%). Mild anti-elevation syndrome developed in one case each in the 1 mm and the 0 mm groups.
Superior oblique palsy is the most common vertical paralytic strabismus and limits both adduction and depression. The inferior oblique muscle is overactive and hypertropia appears in the paralyzed eye. The amount of aggravation of hypertropia can be measured by the amount of head tilt toward the paralyzed eye.1,11,12 Surgical indications of superior oblique palsy include complaints of diplopia, severe vertical strabismus, and facial asymmetry.
Various surgical methods have been reported to treat inferior oblique overaction since Duane13 first reported on inferior oblique muscle tenotomy in 1906. Elliott and Nankin8 have since reported that anterior transposition of the inferior oblique muscle for cases with an angle of vertical deviation less than 13 PD gives good results. Engman et al14 reported that an anterior transposition of the inferior oblique muscle by suturing 1, 2, and 3 mm anterior to the temporal border of the inferior rectus muscle can correct eyes with an angle of vertical deviation less than 15 PD. In Korea, Kim and Kim15 reported an average of 7 PD correction following anterior transposition of the inferior oblique muscle. Min et al16 reported that inferior oblique overaction more than +3 can be treated by anterior transposition of the inferior oblique muscle performed by suturing the inferior oblique muscle to the temporal border of the inferior rectus muscle or 1 mm posterior. The inferior oblique overaction was normalized in 81.8% of patients. Jung and Han17 reported that an anterior transposition of the inferior oblique muscle gave an average correction of 10 PD of vertical angle deviation. In this study, the inferior oblique muscle was sutured to the sclera immediately next to the temporal border of the inferior rectus muscle and the hypothetical continuous line.
Guemes and Wright10 reported on a treatment for dissociative vertical deviation with concomitant primary inferior oblique overaction, unilateral superior oblique palsy, and inferior oblique overaction. The graded recession varied according to the severity of the inferior oblique overaction. Recessions of the inferior oblique muscle 4 mm posterior and 2 mm temporal, 4 mm posterior, 3 mm posterior, 2 mm posterior, 1 mm posterior, or in parallel to the temporal border of the inferior rectus muscle were performed. An average of 20 PD correction in the 1 mm recession cases, 18 PD in the 2 mm recession cases, and 15 PD in the 3 mm recession cases were obtained. The amount of correction was smaller in our cases; nevertheless, it was comparable to that reported by Jung and Han.17 In our study, surgical correction of inferior oblique muscle overaction had an 81.8% success rate, and the surgical correction of hypertropia had a 91% success rate in cases with normalized inferior oblique overaction and hypertropia within 4 PD after surgery.
In recession or anterior transposition, recurrence of the overaction, development of hypotropia, and anti-elevation syndrome are all possible complications. Elliott and Nankin8 reported that inferior oblique muscle overaction recurred in 67% of cases, following a 10 mm recession of the inferior oblique muscle. Raab and Costenbader18 reported that inferior oblique overaction developed in 46.6% of cases when the inferior oblique muscle in the opposite eye was not weakened. Lee19 reported graded recession and anteriorization of the inferior oblique muscle in forty-four eyes and limited up-gaze in both adduction and abduction in the primary position in five eyes. In our study, inferior oblique overaction in the opposite eye developed in 2 cases (9.1%), and hypertropia in the opposite eye developed in 2 cases (9.1%).
The transposition of the inferior oblique muscle is a surgical technique that shortens the distance between the origin and the insertion of the inferior oblique muscle. Thus, it weakens the elevation and abduction, endowing an anti-elevation function. Stager et al20 argued that the anteriorized inferior oblique muscle is a depressor by transposition of the posterior fibers of the inferior oblique muscle to the depressor. Kushner,21 on the other hand, argued that upon upgaze, the inferior oblique muscle is not transpositioned to the depressor, but rather limits elevation. Thus the inferior oblique muscle was transpositioned from elevator to anti-elevator. In addition, it has been reported that the anti-elevation syndrome appeared in all anterior transpositions of the inferior oblique muscle. Due to insignificance, however it was not detected. Furthermore, in the 1 mm group, the limitation upon upgaze may be enhanced upon abduction. Anti-elevation Syndrome is a complication of limitation on up-gaze in the primary position. It can also be depression upon abduction without any evidence of adherent syndrome when an anterior transposition of the inferior oblique muscle is performed on the affected eye. In our study, we performed a graded attachment of the inferior oblique muscle to the inferior rectus muscle posteriorly, according to Wright's method.10 The other option would be to insert the inferior oblique muscle into the inferior rectus muscle anteriorly, resulting in a less severe anti-elevation defect. Mild anti-elevation syndrome developed in one eye in the 0 mm group and one eye in the 1 mm group.
The head tilt test is very useful for diagnosis of unilateral superior oblique palsy and to the assessment of treatment results. This test is based on the theory that, during the head tilt, the ocular meridian line is maintained by oblique and vertical rectus muscle cycloduction. von Noorden reported that the prognosis of superior oblique palsy is very good, with an approximate 85% cure rate. In our cases, nineteen patients exhibited head tilt away from the paralyzed eye. This condition improved or disappeared in eighteen patients (94.7%) following surgery.
In our study, graded recession and anteriorization of the inferior oblique muscle was performed on patients with unilateral superior oblique palsy of less than 15 PD. Good correction of vertical deviation and inferior oblique muscle overaction was obtained. In two eyes, inferior oblique muscle overaction and hypertropia in the opposite eye developed. In the 0 and 1 mm groups, anti-elevation syndrome developed, although this was insignificant. The limitation of our study is the relatively short minimum three-month follow-up period. A longer observation period may be required. Creating the inferior rectus muscle insertion and moving the inferior oblique muscle closer were anticipated to increase the corrected angle for vertical deviation. this result was not statistically significant, although this finding could be due to the small number of patients in each group.
In summary, graded recession and anteriorization of the inferior oblique muscle is suitable for treatment of unilateral superior oblique palsy with concomitant inferior oblique muscle overaction of less than 15 PD. Because postoperative anti-elevation syndrome or hypotropia may develop, a larger study is required.
Notes
This study was presented at the Korean Ophthalmological Society 94th Autumn Meeting, October 2005, Seoul, Korea.
REFERENCES
1. von Noorden GK, Murray E, Wong SY. Superior oblique paralysis. A review of 270 cases. Arch Ophthalmol 1986;104:1771-1776.


3. Reynolds JD, Biglan AW, Hiles DA. Congenital superior oblique palsy in infants. Arch Ophthalmol 1984;102:1503-1505.


4. Sydnor CF, Seaber JH, Buckley EG. Traumatic superior oblique palsies. Ophthalmology 1982;89:134-138.


5. Kushner BJ. The diagnosis and treatment of bilateral masked superior oblique palsy. Am J Ophthalmol 1988;105:186-194.


7. White JW. Surgery of the inferior oblique at or near the insertion. Am J Ophthalmol 1943;26:586-591.

8. Elliott RL, Nankin SJ. Anterior transposition of the inferior oblique. J Pediatr Ophthalmol Strabismus 1981;18:35-38.

10. Guemes A, Wright KW. Effect of graded anterior transposition of the inferior oblique muscle on versions and vertical deviation in primary position. J AAPOS 1998;2:201-206.


12. Oh HI, Roh YB. Head tilting in the patients with superior oblique palsy. J Korean Ophthalmol Soc 1994;35:454-459.
13. Duane A. Tenotomy of inferior oblique and consideration of the conditions that may call for the operation. Br Med J 1906;2:1867-1871.
14. Engman JH, Egbert JE, Summers CG, et al. Efficacy of inferior oblique anterior transposition placement grading for dissociated vertical deviation. Ophthalmology 2001;108:2045-2050.


15. Kim JW, Kim MM. The effect of inferior oblique weakening procedures in the congenital superior oblique palsies. J Korean Ophthalmol Soc 2004;45:1893-1898.
16. Min BM, Park YG, Gho KH. The effect of anteriorization of the inferior oblique muscle in 3 or 4 inferior oblique overaction. J Korean Ophthalmol Soc 1995;36:1014-1019.
17. Jung JI, Han SH. Anterior transposition of the inferior oblique muscle for treatment of hypertropia in superior oblique muscle palsy. J Korean Ophthalmol Soc 1999;40:242-247.
18. Raab EL, Costenbader FD. Unilateral surgery for inferior oblique overaction. Arch Ophthalmol 1973;90:180-184.


19. Lee SY. Effect of graded recession and anteriorization for the overacting inferior oblique muscle. J Korean Ophthalmol Soc 1998;39:2432-2437.
Table┬Ā1
Recession and anterior transposition of the inferior oblique muscle operative method
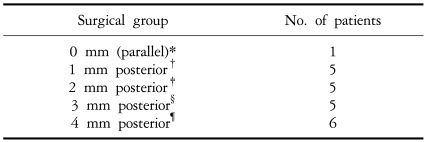
*: The inferior oblique muscle (IOM) insertion was attached to the temporal border of the inferior rectus muscle (IRM), ŌĆĀ: The IOM insertion was attached 1 mm posterior to the temporal border of the IRM, ŌĆĪ: The IOM insertion was attached 2 mm posterior to the temporal border of the IRM, ┬¦: The IOM insertion was attached 3 mm posterior to the temporal border of the IRM, ┬Č: The IOM insertion was attached 4 mm posterior to the temporal border of the IRM.



 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print




