Dear Editor,
Lipogranuloma is a type of soft tissue granulomatous inflammatory reaction that can be caused by lipid deposition or external injection, trauma, or a secondary reaction to systemic diseases [1]. There are several reports of lipogranuloma after diagnostic tests of the orbital or lacrimal system with a lipid-based contrast and application of topical ointment [2]. Periorbital surgery is another potential cause, with cases reported after external dacryocystorhinostomy and even endoscopic sinus surgery (ESS) [3]. Several cases of lipogranuloma occurring after ESS are diagnosed as orbital paraffinoma [3]. We report a case of a patient who presented with severe and recurrent bilateral eyelid swelling after ESS. The patient was treated by systemic steroid and surgical removal of visible lipid-based ointment. Written informed consent for publication of the clinical images was obtained from the patient.
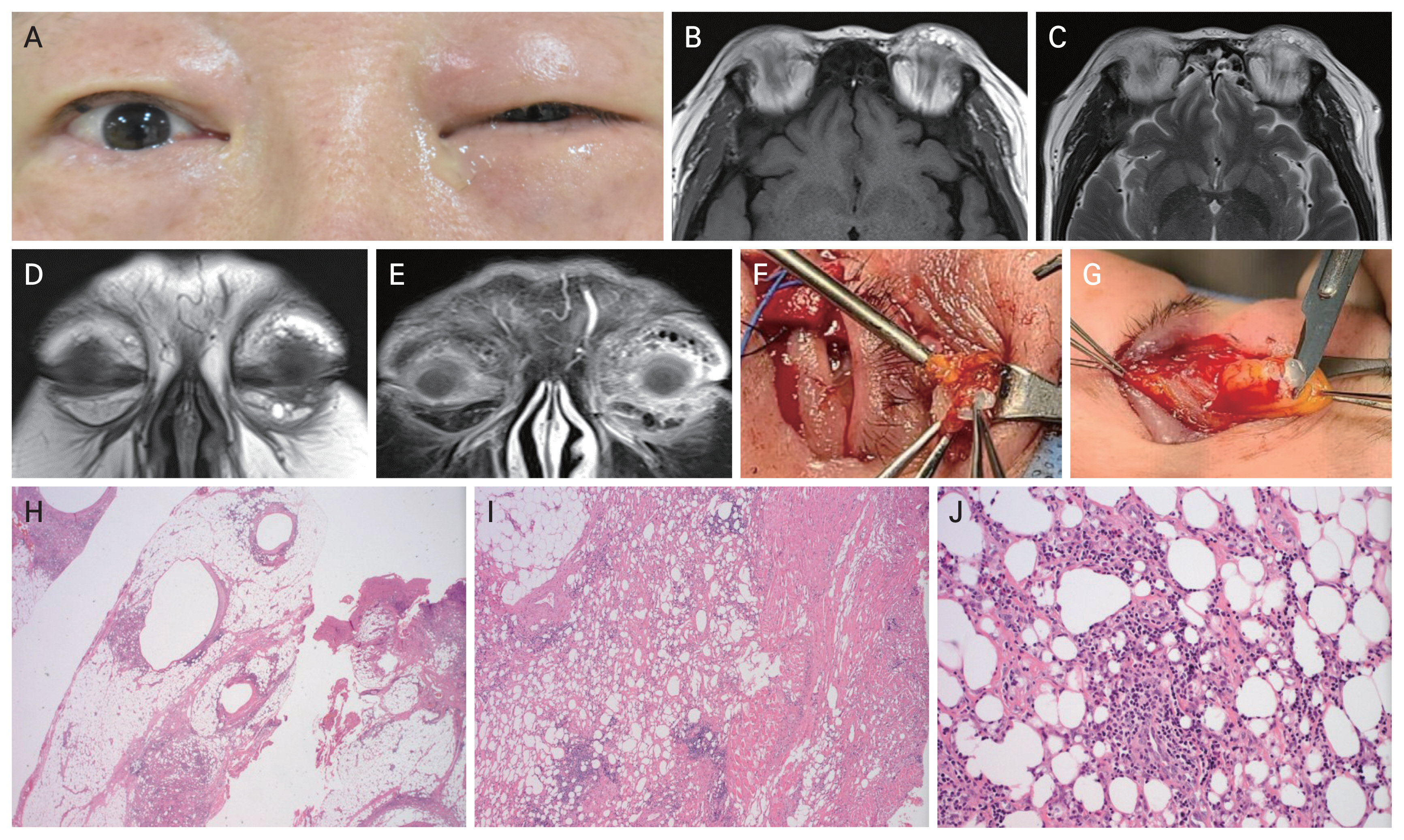
A 57-year-old woman with a history of ESS 2 years prior presented with waxing and waning bilateral swelling of both upper and lower eyelid and multiple palpable masses in various sizes (Fig. 1A). She denied any history of cosmetic surgery. The symptoms occurred 2 weeks after sinus surgery, and resolved with oral prednisone. However, they soon recurred multiple times upon withdrawal of prednisone. According to the patientŌĆÖs medical record, a surgical excisional biopsy was performed 3 months ago at other medical institution, and the diagnosis was chronic inflammation with fat necrosis. Visual acuity was 20/20 in the right eye and 20/50 in the left eye, and the patient denied any visual changes. Extraocular motility was full and pupils were isocoric and reactive without an afferent pupillary defect. On clinical examination, there were the diffuse swelling with palpable, firm and nontender masses over both upper and lower eyelid especially in the medial side. The anterior segment was normal, but fundus examination revealed superior branch retinal vein occlusion with laser marking in the left eye. Magnetic resonance imaging showed well-defined nodular lesions distributed in both upper and lower eyelids that exhibited high signal on T1-weighted images and low signal on the fat-suppressed magnetic resonance image (Fig. 1B-1E). We reviewed her medical record of the outside institution, and no information of nasal packing material was found. The patientŌĆÖs symptoms improved dramatically after treatment with systemic prednisone. As the lesions were localized enough, extensive surgical debulking with biopsy was performed in both eyes. Intraoperatively, multiple masses were found to be attached to the tarsal plate and were excised along with surrounding normal fat tissue. All excised masses contained whitish gelatinous material similar to topical ointment (Fig. 1F, 1G), and the histopathological diagnosis was sclerosing lipogranuloma that showed variable-sized cyst without lining epithelium and necrosis of adipocytes with mixed inflammatory cell infiltration (Fig. 1H-1J). During the observation period through outpatient visits for 1 year after surgery, the patient showed complete improvement of symptoms without recurrence.
During endonasal surgical interventions, the extremely thin bony boundaries between sinuses and orbit, especially the lamina papyracea of the ethmoid sinus, are occasionally undermined. The paraffin used to coat nasal dressings during packing may permeate and involve surrounding tissues, distributed in peripheral orbital tissues and the eyelid. Paraffin acts as foreign bodies that cannot be absorbed, only accumulating and transported since they cannot be easily digested by cellular enzymes, causing chronic inflammation [4]. Lipograuloma is observed more frequently in cases with massive hemorrhage after ESS, where hemorrhage may diffuse paraffin. Due to the extensive spread of paraffin, complete removal is difficult, resulting in frequent recurrence and repeated surgery.
Recently, noncomparative clinical reports have evaluated therapies for periorbital lipogranuloma. Conservative treatment like intralesional and systemic corticosteroids have resulted in a variable good response, but surgical resection is generally known as a treatment of choice [5]. However, complete removal of the lipogranuloma is difficult and may require secondary surgery. Delayed surgical removal is preferred until the granuloma formation by foreign body reaction is probably completed. In this case, we were able to confirm that the ointment material caused continuous inflammation even after a long period of time had passed. Therefore, preoperative systemic steroid treatment allowed the lesion to be localized as much as possible, and extensive surgical excision of it with surrounding fat tissue led to good surgical results.



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print






