Dear Editor,
Cataract surgery is now performed using a smaller incision, which can better withstand extraocular pressure than large incisions. However, small incisions are not sutured, and thus can reopen under sudden pressure. Traumatic aniridia appears as eye damage, including vitreous hemorrhage and hyphema, generally after blunt trauma. Additionally, blunt trauma may cause corneal laceration, cataract, or vitreous prolapse into the anterior chamber. To date, but few cases of complete aniridia have been reported in pseudophakic eyes.
Here we describe a case of isolated traumatic aniridia after uneventful clear corneal incision cataract surgery without iris pigment traces and damage to other intraocular structures. Written informed consent was obtained from the patient after explanation of the nature and possible consequences of the study.
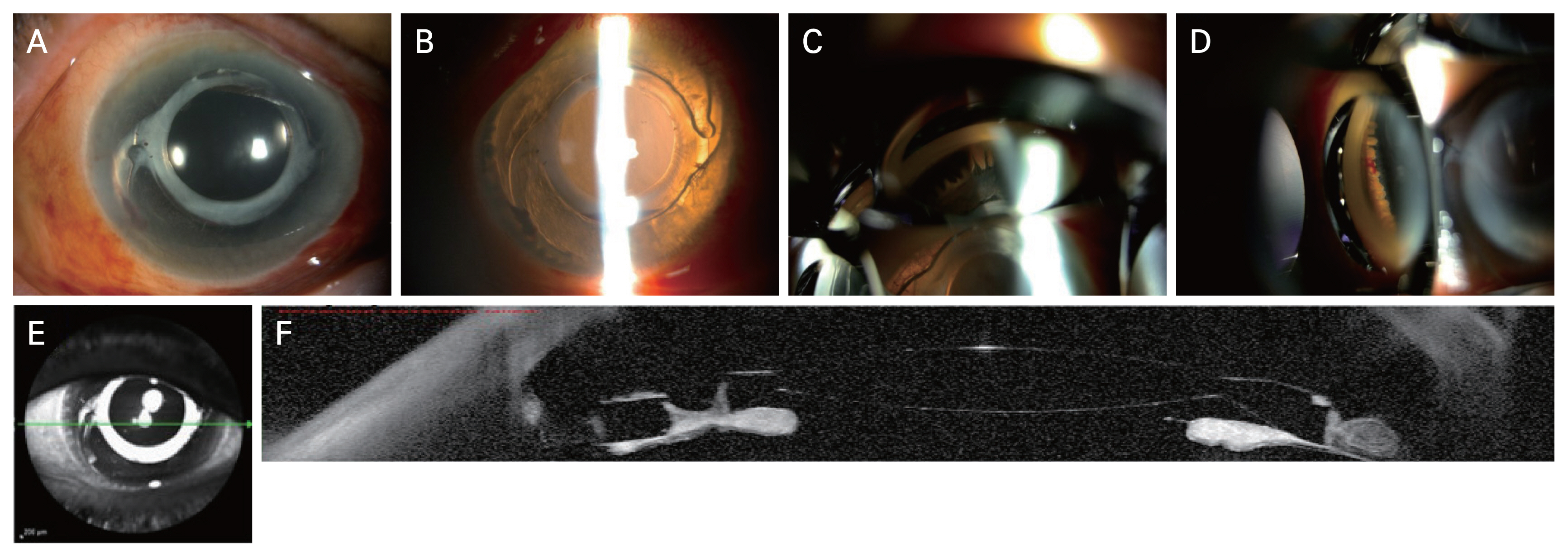
A 79-year-old woman was referred to our ophthalmology outpatient department after her visual acuity decreased following the collision of her right eyeball on the edge of a dresser. The patient had undergone uneventful bilateral phacoemulsification and posterior chamber intraocular lens (IOL) insertion 3 years prior and had no history of neodymium-doped:yttrium-aluminium-garnet (Nd:YAG) laser capsulotomy. At presentation, the visual acuity in her right eye was counting fingers at 50 cm, and intraocular pressure (IOP) was 13.1 mmHg. Slit-lamp examination revealed corneal edema and a blood clot in the endothelium. No iris was visible, but hyphema was present in the anterior chamber. The capsular bag and single-piece IOL appeared intact. The latter was in situ and adhered to the capsule without donesis (Fig. 1A, 1B). The fundus appeared blurry, but there was no residual iris in the vitreous cavity. Also, B-scan ultrasonography showed no evidence of vitreous hemorrhage or retinal detachment. Scleral ruptures were absent. The patient was treated with topical prednisolone and antibiotics.
One week later, visual acuity in the right eye was 20/200. The iris root was not visible; however, the ciliary process was visible at 360° by gonioscopy (Fig. 1C, 1D). Orbital computed tomography showed no abnormalities; however, anterior segment optical coherence tomography revealed aniridia (Fig. 1E, 1F). Seven weeks later, the visual acuity was 20/50 and the IOP was 12 mmHg. The cornea appeared clear, and no cells were visible in the anterior chamber. The IOL remained stable and adhered to the capsule without donesis. Likewise, the posterior capsule and segment were intact and stable.
Given the absence of the iris and of rupture sites, we presumed that the iris had been completely extruded through the small corneal incision. Navon [1] and Ball et al. [2], likewise, reported expulsive iridodialysis through an incision, while the IOL and lens capsule appeared intact. The authors [1,2] presumed that the scleral tunnel prevented eye rupture by acting as a valve to release traumatic pressure. As our patient had undergone cataract surgery at another clinic, we had limited information about the incision size or type (single-, two-, or three-planes); however, a clear corneal incision (<2.5 mm) was observed, without leakage. Also, as our patient had no history of Nd:YAG laser capsulotomy, the capsule and IOL likely decreased the impact of the traumatic pressure and minimized intraocular damage [3].
Clear corneal incisions heal more slowly than do scleral or limbal wounds. Although the possibility of wound leakage decreases over time, traumatic aniridia, which occurred 7 years after cataract surgery, has also been reported by Georgalas et al. [4]. A well-made incision is required to reduce the wound dehiscence incidence, particularly for a clear corneal incision. Smaller sized, stepped incisions, rather than a single incision and square surface architecture, have been recommended to improve wound stability [5]. The surgeon should ensure the integrity of the wound, particularly while closing with stromal hydration, and should reduce the pressure gradient during phacoemulsification to avoid iris prolapse.
In our case, it is thought that the capsule and IOL moved like a trampoline, absorbing the impact of the traumatic pressure and minimizing intraocular damage [4]. This case emphasizes that even small, clear corneal incisions can be vulnerable to trauma and cause wound dehiscence, even years after cataract surgery. An intact capsule and an IOL could reduce the trauma impact by a rebound effect, absorbing the impact of traumatic pressure and preventing damage to other ocular structures. The prognosis is expected to be good in cases where only aniridia occur after trauma.
Fig. 1
Images of the patient. (A) Slit-lamp photography of the right eye at initial examination. (B) Retroillumination of the right eye shows the intraocular lens adhered to the capsule and the intact posterior capsule. Gonioscopy shows the ciliary process without an iris root from (C) the inferior angle and (D) the nasal angle of the right eye. (E,F) Anterior segment optical coherence tomography of the right eye shows complete aniridia with a well-positioned intraocular lens.



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print






