Overt and Massive Spontaneous Subconjunctival Hemorrhage on a Patient with Prolonged International Normalized Ratio on Therapeutic Warfarin: A Case Report
Article information
Dear Editor,
Subconjunctival hemorrhage is a common benign condition of the eye that can happen to anyone regardless of the use of anticoagulant. Usually, it appears as a sudden, painless redness in the eye. Trauma is known to be the most common major risk factor [1].
Warfarin is the most commonly used anticoagulant around the world for the prevention and treatment of venous thromboembolism and systemic embolism. It acts by inhibiting the action of vitamin K dependent coagulation factors, which are II, VII, IX, and X. The effect of warfarin is measured via prothrombin time (PT) and international normalized ratio (INR). Bleeding is the most common primary adverse effect associated with warfarin use. Approximately 15% of the patient on warfarin will experience some form of minor bleeding episode [2]. According to Superstein et al. [3], six out of 126 patients (4.76%), who were receiving warfarin therapy, had ocular bleeding.
Written informed consent for publication of the research details and clinical images was obtained from the patient. A 61-year-old Asian male patient came to our emergency department on July 26, 2022, complaining bloody tears on his left eye. The patient found sudden bleeding in the left eye upon waking up. The patient stated that he had no history of ocular trauma or rubbing. He was treated for central retinal vein occlusion on his right eye at our ophthalmology outpatient clinic, and the left eye had no known ophthalmic problems. No treatment was given other than the frequent intravitreal bevacizumab injections in the right eye.
In addition to hemodialysis treatment due to end-stage renal disease, the patient was diagnosed with hypertension, coronary artery disease, and paroxysmal atrial fibrillation. The patient was taking clopidogrel 75 mg and warfarin 2 mg daily since July 2019 at our internal medicine cardiology clinic.
Visual acuity and intraocular pressure could not be measured due to the massive subconjunctival bleeding. Active bleeding and hematoma at conjunctiva and extensive periorbital ecchymosis were found (Fig. 1A). Due to the continuous bleeding overflow, it was difficult to examine the patient’s eye through the slit-lamp, but no visible conjunctival laceration was found. Ocular ultrasound revealed that there was no hemorrhage in vitreous.
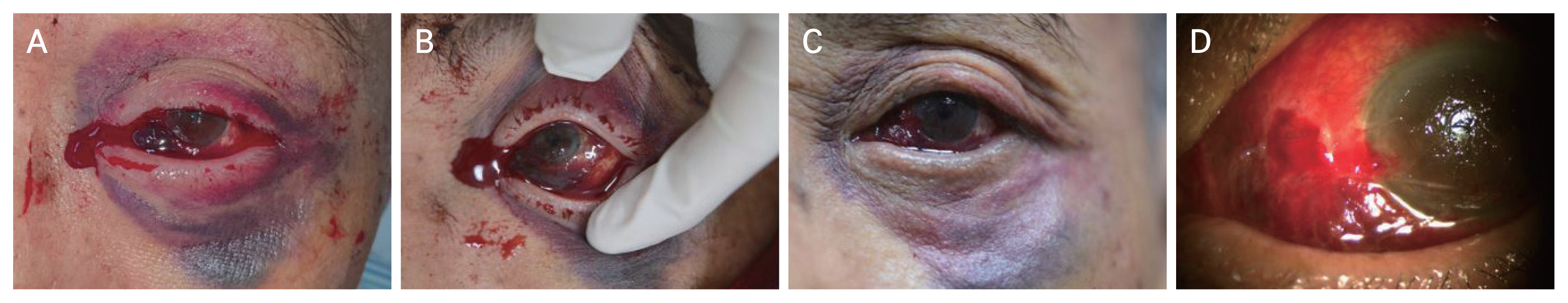
Active bleeding and hematoma in conjunctiva and extensive periorbital ecchymosis are found in the left eye. (A) Blood kept overflowing onto the patient’s face. (B) Upper and lower lid manually retracted superiorly and inferiorly. After 5 hours of manual compression, active bleeding persists. (C) On the next day of surgical procedure, active subconjunctival bleeding stopped. (D) Conjunctival wound is sutured and chemosis is found. The patient provided written informed consent for publication of the clinical images.
Even after manual compression and ice bag application on the left eye for 5 hours, the blood kept overflowing onto the patient’s face once we took our hands off (Fig. 1B). The laboratory work-up reported INR of 3.69 (normal range, 0.8–1.12; 2.0–3.0 with therapeutic anticoagulation), with a PT of 42.2 seconds (normal range, 9.8–12.7 seconds), and activated partial thromboplastin time of 62.8 seconds (normal range, 21–36 seconds), which were all significantly prolonged. After consulting with the patient’s cardiologist, the decision was made to cut all the anticoagulant drug use and reverse the warfarin effect with 5 mg of vitamin K.
As bleeding continued despite all of these treatments, we concluded that surgical intervention was needed. Under the microscope, we electrocauterized the focal nasal artery of the conjunctiva and sutured the site. As a result, although the amount of bleeding decreased significantly, there was still mild conjunctival bleeding and manual compression was continued.
The patient was admitted to the general ward at the internal medicine cardiology department to correct the prolonged INR. On the next day, laboratory work-up showed an INR of 1.87 with a PT of 21.6 seconds, which significantly improved since the previous day. On slit-lamp examination, the subconjunctival bleeding that started 18 hours ago had finally stopped (Fig. 1C, 1D). The best visual acuity in the left eye improved to 50 / 50 at his final follow-up appointment.
Subconjunctival hemorrhage usually does not require any interventions because it resolves on its own within 5 to 10 days. Ophthalmologists can manage the symptom with further treatments, such as manual compression and ice bag application. If bleeding persists, surgical intervention should be considered. However, in this case, the patient’s bleeding stopped after the ocular surgical management and INR correction by cutting the anticoagulant and intaking vitamin K.
In order to treat patients with uncontrolled subconjunctival hemorrhage, it is crucial to examine the patient’s medical history for any underlying disease or anticoagulant use along with ocular treatments. Consulting the internal medicine physician for cutting the anticoagulant must be considered. Also, it is recommended that patients, undergoing anticoagulant therapy, should have regular checkup of PT and INR, and adjust the anticoagulant dose accordingly.
Acknowledgements
None.
Notes
Conflicts of Interest: None.
Funding: None.