Effect and Safety of Pressure Sensor-equipped Handpiece in Phacoemulsification System
Article information
Abstract
Purpose
To evaluate the effect of the Active Sentry handpiece of the Centurion Vision System compared to the Centurion Ozil handpiece for phacoemulsification in cataract surgery.
Methods
A retrospective study was conducted on 281 patients (449 eyes) who underwent cataract surgery between August 2020 and June 2021. Preoperative measurements, intraoperative parameters, complication rate, and postoperative outcomes were compared between the Active Sentry handpiece and the Centurion Ozil handpiece groups. Additionally, the parameters were compared in different cataract severity groups and multiple predictive factors for the number of active surge mitigation (ASM) actuations were assessed with the Active Sentry handpiece.
Results
There were 198 eyes in the Active Sentry group and 251 eyes in the Centurion Ozil group. There were no statistically significant differences between the two groups, as the cumulative dissipated energy in the Active Sentry and Centurion Ozil groups were 8.32 ± 7.74 and 7.87 ± 9.25 μJ, respectively (p = 0.576). Total surgery time, ultrasound usage time, aspiration time, amount of fluid aspirated, postoperative corrected distant visual acuity, and postoperative decrease in corneal endothelial cell density were comparable between the two groups. The significant contributors to the number of ASM actuations were age, preoperative corrected distant visual acuity, axial length, and total ultrasound time.
Conclusions
There was no clear advantage of the Active Sentry handpiece compared to the Centurion Ozil handpiece. ASM actuation increases with age, poor visual acuity before surgery, short axial length, and prolonged ultrasound usage time. It is expected that in more severe and high-risk cataract surgery, the Active Sentry handpiece functions more effectively, possibly affecting the safety and prognosis.
Currently, phacoemulsification is the most common and basic technique used for cataract surgery. Phacoemulsification systems, fluidics, and ultrasound tips have been developed for easier and safer surgery through various studies and technologies [1,2]. Fluidics, which control the flow of fluid through the eye, is important for the efficiency and safety of phacoemulsification. Compared to the conventional passive fluidic method based on gravity, Active Fluidics technology (Alcon Laboratories Inc) adjusts the fluid bag pressure in response to changes in irrigation pressure built into the cassette, and it has been confirmed that intraocular pressure (IOP) can be maintained almost constant in a laboratory environment [3,4].
The ability to rapidly control the fluid and maintain adequate IOP in situations with fluctuations in the anterior chamber, such as postocclusion surge response, is critical for stable chamber maintenance and successful cataract surgery [5–7]. Studies published in 2016 and 2018 compared the Infinity Vision System (Alcon Laboratories Inc) of the gravity-fluidics method and the Centurion Vision System (Alcon Laboratories Inc) of the newly introduced the active-fluidics method and showed superior surgical results in lower accumulated energy, aspirated fluid volume, and aspiration time reported with the Centurion Vision System using Active Fluidics technology [4,8].
In addition to Active Fluidics technology, an Active Sentry handpiece containing an integrated pressure sensor inside the handpiece was developed. It can respond faster and more sensitively to changes in IOP by eliminating the delay in fluid adjustment compared to the earlier version, which has a pressure sensor near the cassette, thus, reducing IOP fluctuations [9]. Especially in postocclusion surge events, where intraocular pressure can suddenly drop, it is expected to quickly control flow, maintain a consistent IOP, and reduce surgical complications, such as anterior chamber collapse and damage to the cornea, iris, and lens capsule. It also automatically detects and corrects the patient’s eye level and inflow-outflow rate; thus, the anterior chamber is maintained more stable during surgery and is considered to increase the stability and efficiency of cataract surgery [10]. This study aimed to compare the effects of using an Active Sentry handpiece in cataract surgery and analyze surgical outcomes according to cataract grade.
Materials and Methods
Ethics statement
This study was approved by the Institutional Review Board of Yonsei University College of Medicine (No. 4-2022-0615) and was conducted following the tenets of the Declaration of Helsinki. The requirement for informed consent was waived due to the retrospective nature of the study.
Study participants
This is a retrospective and comparative study based on medical records of 449 eyes in 281 patients who underwent cataract surgery using the Centurion Vision System with Active Fluidics technology by one surgeon (IJ) at Severance Hospital (Seoul, Korea), from August 2020 to June 2021. Data were extracted from electronic medical records with anonymization by the researcher. Patients who have ocular disorders that significantly impair visual acuity including corneal opacity, glaucoma, retinal diseases, a history of ocular trauma, intraocular surgery, or inflammation, those who lost any preoperative or phacoemulsification-related intraoperative parameters that we need to evaluate, and those who did not maintain postoperative follow-up visits were excluded from the data analysis.
Data collection and analysis
Intraoperative and postoperative parameters were evaluated and analyzed in two groups operated with the Active Sentry handpiece and Centurion Ozil handpiece. All factors, such as cataract hardness or surgical difficulty, were not considered for the type of handpiece.
Demographic data, including age and sex, were collected. Preoperative ocular examinations included uncorrected distant visual acuity and corrected distant visual acuity (CDVA), IOP, manifest refraction, slit lamp, fundoscopy, specular microscopy (EM4000, Tomey), IOLMaster 700 (Carl Zeiss Meditec AG), and iTrace (Tracey Technologies). Biometric measurements including keratometry, axial length, anterior chamber depth, lens thickness, and white-to-white were obtained, and intraocular lens power was calculated, using IOLMaster 700. The severity of cataracts was based on the dysfunctional lens index (DLI) value of iTrace for objective evaluation on a scale of 0 to 10, with lower numbers indicating more severe cataracts [11].
Intraoperative parameters during phacoemulsification included total case time, cumulative dissipated energy (CDE), total ultrasound time, aspiration time, estimated fluid aspirated, the number of active surge mitigation (ASM) actuations. Postoperative assessments were included visual acuity, endothelial cell density (ECD) reduction at 1 month after surgery, and any complications. These parameters were compared between the Active Sentry and the Centurion Ozil groups. These parameters, including the number of ASM actuations, were also analyzed in the three different cataract severity groups using the Active Sentry handpiece. We attempted to identify the factors that affect the number of ASM actuations to determine which conditions the Active Sentry handpiece more significantly contributed to cataract surgery.
Statistical analysis
Statistical analyses were performed using IBM SPSS ver. 25.0 (IBM Corp). Preoperative and intraoperative parameters and postoperative outcomes were compared between the Active Sentry and the Centurion Ozil groups using an independent t-test. A one-way analysis of variance test was employed to compare the parameters in the three groups with different cataract severities. Factors affecting the number of ASM actuations in the Active Sentry group were determined by multivariate linear regression analysis using the backward elimination method. Statistical significance was set at p < 0.05.
Results
Patient characteristics and preoperative assessment
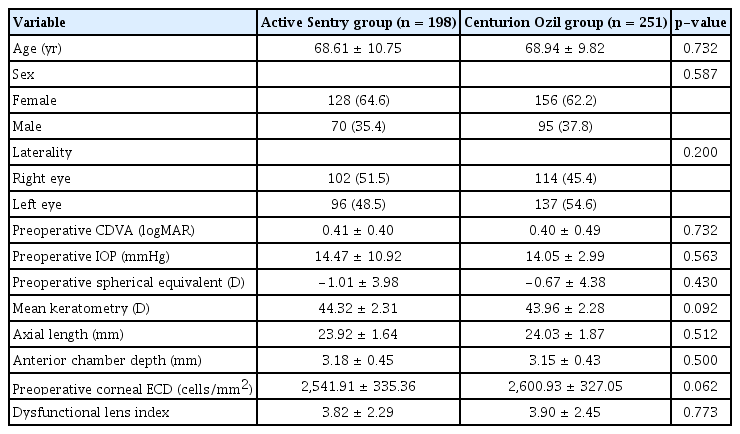
A total of 449 eyes from 281 patients were included in this study, of which 198 eyes were operated using the Active Sentry handpiece and 251 eyes using the Centurion Ozil handpiece. There were no statistically significant differences in patients’ demographics or preoperative measurements, including age, sex, CDVA, spherical equivalent, mean keratometry, axial length, anterior chamber depth, corneal ECD, and DLI of iTrace between the two groups (Table 1).
Comparison of intraoperative parameters
The total case time, total CDE, total ultrasound time, total aspiration time, and total estimated fluid aspirated were recorded in the Centurion Vision System after surgery, and these parameters were compared between the Active Sentry and Centurion Ozil groups (Table 2). The mean CDE was 8.32 ± 7.74 μJ in the Active Sentry group and 7.87 ± 9.25 μJ in the Centurion Ozil group. There was no statistically significant difference between the two groups (p = 0.576). All other parameters were comparable between the two groups (p > 0.05). In the Active Sentry group, ASM was activated approximately 16.99 ± 9.64 times per surgery on average.
Complications and postoperative outcomes
Four eyes (2.02%) in the Active Sentry group and four eyes (1.59%) in the Centurion Ozil group developed complications, including posterior capsular rupture or combined anterior vitrectomy during surgery, with no statistically significant differences between the two groups (p = 0.735). No other complications were observed, including dropped nucleus, iris damage, cystoid macular edema, endophthalmitis, lens dislocation, pseudophakic bullous keratopathy, retinal detachment, uncontrolled IOP, or glaucoma.
Analysis of the two groups revealed that postoperative IOP was lower when using the Active Sentry handpiece (p = 0.013) but did not reveal statistically significant differences in other postoperative outcomes, including postoperative CDVA and a decrease in corneal ECD (Table 3).
Analysis of intraoperative parameters and clinical outcomes based on cataract severity
Since there was no significant difference in intraoperative parameters between the Active Sentry and Centurion Ozil groups, the analysis between the three groups of different cataract severities assessed by the DLI of iTrace was performed in the Active Sentry group to compare the number of ASM actuations and the effect of the Active Sentry handpiece. According to the DLI value, cataract severity was categorized into three groups: mild (DLI > 6), moderate (3 < DLI ≤ 6), and severe cataracts (DLI ≤ 3). The more severe the cataract, the more energy, ultrasound time, and fluid used for surgery, and the lower the visual acuity after surgery. In severe cataracts, the number of ASM actuations tended to increase, and the decrease in corneal ECD after surgery tended to worsen, but this was not statistically significant (Table 4). When comparing only severe cataracts (DLI ≤ 3) in the Active Sentry and Centurion Ozil groups, the differences in outcome were not statistically significant between the two groups (Supplementary Table 1).
Multivariate linear regression analysis of ASM actuations in the Active Sentry handpiece
Multivariate regression analysis to examine multiple demographic or biometric factors (age, sex, preoperative CDVA, IOP, axial length, anterior chamber depth, spherical equivalent, mean keratometry, white-to-white corneal diameter, lens thickness, and ultrasound time) associated with the number of ASM actuations during cataract surgery revealed that age, preoperative CDVA, axial length, and total ultrasound time were significantly associated with the number of ASM actuations (Table 5). The final regression model was highly significant (p < 0.001), with a correlation coefficient of 0.609. Age, preoperative CDVA, and total ultrasound time were positively associated with ASM actuation (p = 0.038, p = 0.011, and p < 0.001, respectively). The axial length was negatively associated with ASM actuation (p = 0.011). The other variables did not contribute significantly to the number of ASM actuations.
Discussion
The Active Sentry upgrade is known to allow faster mitigation of surge response with the ability to sense IOP at the handpiece level [6]. It is expected that Centurion Vision System with Active Sentry handpiece improves the effectiveness and safety of cataract surgery by more sensitively controlling the fluid and improving anterior chamber stability than the conventional handpiece. However, in this retrospective study, there were no significant differences in intraoperative parameters or postoperative outcomes, including CDE, postoperative visual acuity, and decrease in corneal ECD, between the Active Sentry and the Centurion Ozil groups.
Several experimental studies analyzing the change of IOP or surge volume to evaluate anterior chamber stability after occlusion break events with the Active Sentry handpiece have been reported. Using the mechanical spring eye model, Centurion Vision System with Active Sentry had lower aqueous volume losses after occlusion break than other phacoemulsification systems [9]. Another study suggested Centurion Vision System with Active Sentry group has a lower percentage reduction of IOP and faster recovery to baseline IOP compared with the traditional handpiece by analyzing the real-time rate of drop and rise of IOP after occlusion break event in rabbit eyes [10]. Suzuki et al. [11] also reported similar results in porcine eyes that the Active Sentry handpiece contributes to anterior chamber depth stability even when occlusion occurs. According to these previous studies, the Centurion Vision System with Active Sentry handpiece is useful for controlling the IOP in surge events and maintaining anterior chamber stability. However, these are experimental studies triggering a specific situation of occlusion break. Whether the differences in chamber stability shown in these research results in an experimental environment can lead to a reduction in complication rate or better postoperative prognosis in human cataract surgery is another question.
Other studies on the clinical outcome of the Active Sentry handpiece in cataract surgery have been published. Jiraskova and Stepanov [12] compared the parameters of phacoemulsification using the two handpieces and showed a statistically significant reduction in CDE and ultrasound time in the Active Sentry group compared to the Centurion Ozil group. This result differs from the findings of our study, which showed no significant differences between the two groups. Another previous study by Cyril et al. [13] found no significant differences between the two groups when comparing CDE, patient and surgeon comfort levels, and postoperative CDVA prospectively. This is similar to the results we derived, but they reported that there is an advantage because a lower IOP is set in the Active Sentry group.
The Active Sentry handpiece was expected to reduce the complications of cataract surgery by preventing the chamber from collapsing and utilizing less energy when emulsifying the nucleus [6,9–11]. To evaluate the rate of complications when using the Active Sentry handpiece, complicated and difficult cataract cases were not excluded from our data, unlike previous studies. However, there was no clear difference in the rate of complications and evaluation was limited because complications are rare. Even the actual complication rate is much lower than approximately 2% because the total number of cases was reduced by excluding those not obtained or lost in the data collection process like phacoemulsification parameters.
It can be explained that there were no significant differences in CDE or other parameters between the two groups using Active Sentry and Centurion Ozil handpieces. One possibility is that the functional differences between the two handpieces may be more pronounced only in more severe and difficult-to-operate cataract surgery cases. When the surgical results were compared in the severe cataract group (DLI ≤ 3), there was no significant difference between the two groups either. However, since these comparisons lacked the number of patients and simply considered DLI values, additional studies in a larger group are needed by comprehensively considering anterior chamber depth and axial length. Another possibility is that the Active Sentry handpiece contributes to the earlier detection of chamber instability and maintenance of IOP, but the difference in the handpiece is insufficient to lead to clinically meaningful differences in ultrasound energy reduction or better postoperative outcomes, considering that both groups used Active Fluidics technology. Postoperative IOP was found to be statistically lower in the Active Sentry group. It can be affected by the ability of the Active Sentry handpiece to maintain the anterior chamber more stable, but the values of the two groups were 12.26 ± 3.11 and 12.98 ± 2.93 mmHg, respectively, which were not considered clinically meaningful differences.
In the analysis of the three groups with different cataract severities, more energy, ultrasound time, aspiration time, and aspirated fluid were required as the severity of cataracts increased. This analysis also revealed that the DLI of iTrace, used to classify cataract severity, was strongly correlated with preoperative visual acuity and is a reliable assessment method for cataract grade. This is also consistent with the results of previous studies on DLI as objective metrics correlated with the Scheimpflug-measured average density, subjective lens grading, and preoperative CDVA [14]. Although the most severe cataract group had the highest number of ASM actuations, there was no statistically significant correlation in the Active Sentry group.
The new features of the Active Sentry handpiece include ASM, which releases fluid into the aspiration tube using quick-valve technology when the built-in sensor in the handpiece detects an occlusion break [6,12,13]. In other words, ASM reduces the prevention of surge events or anterior chamber collapse and helps maintain chamber stability. The number of ASM actuations can be identified from the records in the Centurion Vision System after the operation. Unlike the expectation that the number of ASM would increase in severe cataracts due to the hardness of lens and frequent surge events during surgery, there was no statistically clear correlation between the severity of cataract and ASM expression. So, we tried to find out the factors that increase the number of ASM actuations, that is, under what conditions the Active Sentry handpiece contributes more actively to cataract surgery. Among various factors, age, preoperative CDVA, axial length, and total ultrasound time had significant effects on the number of ASM actuations. The number of ASM increased as the patient’s age increased, preoperative visual acuity was poor, and the phacoemulsification time was longer. The axial length of the eye showed a negative association with ASM actuation. This means that the older the patient, the more severe the cataract, and the shorter the eye, the more often the surge event occurs, and the more frequently the ASM functions, which would affect the anterior chamber stability.
This retrospective study has some limitations. First, as this study is a retrospective study, randomization between the two groups was not performed. Second, some cases were excluded from the study in the data collection process due to missing information on ophthalmologic examination results or intraoperative parameters. This can contribute to selection or missing bias and affect the results. Third, the possibility of complications in cataract surgery was very low, so the number of study participants was too small to compare the incidence rates of complications. Although the Active Sentry group did not show superior outcomes, it is expected that it would be useful in cataract surgery cases of patients with a high probability of complications such as relatively old age, difficulty in cooperation, severe cataract, and short eyes. Lastly, unlike the previous experimental studies about the Active Sentry handpiece, this study lacked appropriate parameters or measures to evaluate surges between the two groups.
In this study, energy or time of phacoemulsification, postoperative visual acuity, ECD, and complications after cataract surgery were comparable between the Active Sentry and Centurion Ozil groups. However, our results showed that the number of ASM actuations increased in challenging cases that require a long ultrasound time in older patients with poor visual acuity and short eyes. Therefore, the Active Sentry handpiece is expected to function more effectively with a better prognosis for cataract surgery in severe and high-risk groups. More prospective studies on various parameters are needed, with challenging cases with severe cataracts and shallow anterior chambers in larger groups.
Acknowledgements
None.
Notes
Conflicts of Interests: None.
Funding: This work was supported by a new faculty research seed money grant for 2022 from Yonsei University College of Medicine (No. 2022-32-0071), the Basic Science Research Program of the National Research Foundation of Korea (NRF) (No. NRF-2021R1I1A1A01047951), and the Korean Fund for Regenerative Medicine (KFRM) grant (No. KFRM 22C0615L1), funded by the Korean government (the Ministry of Science and ICT and the Ministry of Health and Welfare). The funding organizations had no role in the design or conduct of this study.
Supplementary Information
Supplementary materials are available from https://doi.org/10.334/kjo.2022.0157.
Supplementary Table 1.
Analysis of parameters and clinical outcomes in the severe cataract group (DLI ≤ 3)