Dear Editor
Ectopic lacrimal gland tissue is reported to be located at epibulbar conjunctiva, other locations including orbital, eyelid, intraocular, lacrimal sac, and nasal mucosa sites [1]. Although ectopic lacrimal glands in the ciliary body are quite rare, there have been more than 10 cases reported worldwide [2,3]. Although accompanying proptosis at the time of diagnosis has been frequently reported, studies on long-term follow-up outcomes and complications are limited. Herein, we report a single case of ectopic lacrimal gland on ciliary body, resulting in secondary glaucoma during 20 years of follow-up. Informed consent for publication of the research details and clinical images was obtained informed consent from the patient.
A previously healthy 10-month-old female patient presented with right upper eyelid swelling and redness. And she was admitted to an emergency room in 2003. B-scan ultrasonography and orbit computed tomography demonstrated right orbital cellulitis and a round-shaped, 0.8-cm ciliary body mass. Fine needle aspiration and incisional biopsy were done, which revealed ectopic lacrimal gland tumor in histology. The size of residual mass gradually increased and there was no sign of malignant transformation during 17 years of follow-up period. The patient was transferred to the glaucoma clinic due to intermittent high intraocular pressure and corresponding ocular pain of the right eye once or twice a month in 2020. Thus, she started dorzolamide 2%/timolol maleate 0.5% fixed combination (Cosopt, Merck & Co Inc). No other abnormal findings were observed on slit-lamp examination.
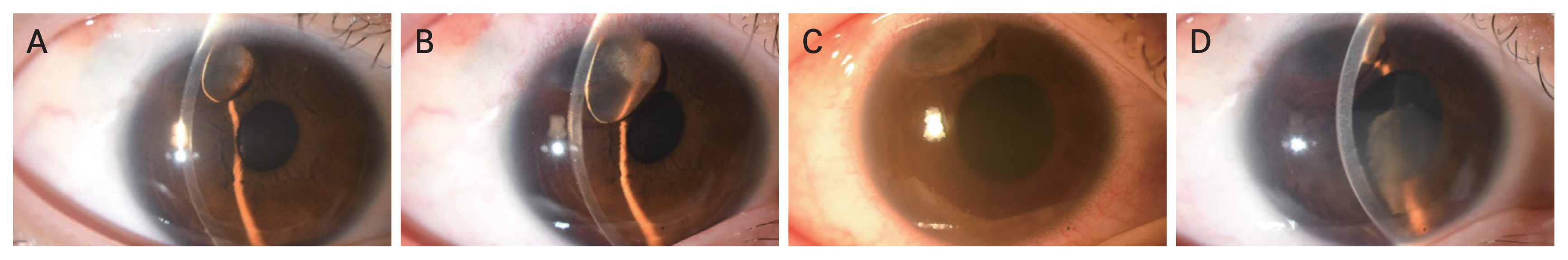
On January 10, 2021, she was admitted to an emergency room due to ocular pain and decreased vision in the right eye that started a day ago. Best-corrected visual acuity was 2 / 20 and intraocular pressure (IOP) measured by Goldman applanation tonometer was 44 mmHg. Slit-lamp examination showed corneal edema and moderate anterior chamber inflammation (cell grade from +2 to +3). Anterior chamber was deep enough and there was no peripheral angle closure. Pupil was fixed and fundus was normal in the right eye. The left eye was normal. Under the impression of secondary glaucoma associated with uveitis, she was treated with additional oral acetazolamide, topical prednisolone acetate 1% (Prednilone, Daewoo Pharm), brimonidine 0.15% (Alphagan-P, Allergan Inc) and intravenous mannitol injection. IOP was in the normal range after 3 days. Although she used Cosopt and Alphagan prophylactically, there were two more additional acute glaucoma attacks in 2021. Slit-lamp examination revealed new cystic lesion in superotemporal iris in March 2, 2022 (Fig. 1A). On July 6, 2022, the cystic lesion became larger than 4 months before (Fig. 1B), but there was no other abnormal sign such as increased IOP or anterior chamber inflammation.
On July 29, 2022, she was admitted to emergency room with a third attack, presented with decreased visual acuity and 33 mmHg of IOP in the right eye. The size of ciliary body mass was slightly decreased but there was flare reaction and inferior floating cells in the anterior chamber (Fig. 1C). The next day, cyclitic membrane was observed more clearly in the anterior chamber (Fig. 1D). As diagnosed with uveitis associated with iris cyst rupture, on August 4, 2022, she underwent anterior chamber and iris cyst aspiration biopsy of the right eye. The results of cytology revealed suspicious findings of lacrimal gland secretion, but no malignant cells were observed, and some pigment laden macrophages existed. During 2 months of follow-up period, IOP fluctuated from 10 to 38 mmHg. Therefore, short-term follow-up and additional anterior chamber irrigation to control IOP is considered.
To conclude, we report a case of secondary glaucoma associated with ectopic lacrimal gland tumor that eventually ruptured during a 20 years of long-term follow-up period. Although rare, long-term follow-up revealed ectopic lacrimal gland may cause uveitis and glaucoma attacks. Our limitations are that examinations showing glaucoma status such as optical coherence tomography or visual field examination were rarely performed during the follow-up period. Although optical coherence tomography did not show retinal nerve fiber layer thinning nor macular thinning yet, follow-up examinations are needed to confirm that recent Increase in IOP does not lead to structural and functional damage in the future.



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print






