Partial to complete shutdown of ophthalmic clinics and surgeries in the United States began in March 2020 in response to the COVID-19 pandemic [
1,
2]. Adapting safety measures to continuously evolving guidelines allowed clinics to ramp care back up but required triaging based on unprecedented clinical constraints. US clinic volume decreased between 40% to 60% during the first pandemic wave [
3]. Song et al. [
4] triaged urgency based on the next follow-up date which reduced scheduled appointments by 28% (and of that only 24% attended) and new appointments by 78% in the immediate 2-month aftermath. They saw the best maintained attendance rate in the retina clinic only at 74% and overall, in the highest urgency subgroup at 68%. Unintended delay in chronic disease management in the clinic led to progression of vision decline from diabetic macular edema and neovascular age related macular degeneration [
5-
7], as well as proliferative complications of nonproliferative diabetic retinopathy (NPDR) and stable PDR [
8]. In a pilot study, University of Texas Health San Antonio (San Antonio, TX, USA) saw an above normal surge in panretinal photocoagulation (PRP) procedures for PDR within 4 months of normalizing clinic volume that corresponded to patient anecdotes of missing appointments due to fears of contracting the disease, which has been described by other institutions [
9,
10]. It was not known if our COVID-19-related triaging had impacted care delay and DR progression and would lead to vitrectomies in excess of pre-COVID-19 times. Our search has not found whether triaging systems or patient-related fears were the dominant drivers in delay, disease progression, and how consequent proliferative complications were eventually managed.
To better understand the impact of COVID-19-related triaging and patient-related factors on care delay, disease progression, and management of proliferative complications in patients with PDR, we evaluated differences in patient follow-up behavior and disease factors for those who required surgery versus those who were managed with clinic procedures during the pandemic shutdown.
Materials and Methods
Ethics statements
This retrospective case-control study was approved by the Institutional Review Board of University of Texas Health San Antonio (No. HSC20210374EX) and adhered to the tenants of the Declaration of Helsinki. Informed consent was waived due to the retrospective nature of the study.
Patients and data
The study included patients who received diagnosis of PDR and were evaluated and treated between January 1, 2018, and March 4, 2021 at the University of Texas Health Science Center. Recorded electronic medical records data was retrieved for all ophthalmic visits and included date of visit, International Classification of Diseases 10th Revision (ICD-10), Current Procedure Terminology (CPT) code, provider, appointment type, appointment completion status, and reason for appointment cancellation.
Inclusion and exclusion criteria
Inclusion criteria were that patients had CPT codes for pars plana vitrectomy (PPV), PRP, and/or intravitreal injection (IVI) of anti-vascular endothelial growth factor (anti-VEGF) for the corresponding ICD-10 diagnosis of PDR. To evaluate follow-up trends, patients were excluded if they received fewer than two appointments before or after the COVID-19-associated clinical shutdown date in South Texas (set at March 1, 2020). Patients with confounding codiagnoses for proliferative retinopathy, such as venous or arteriolar occlusions or sickle cell retinopathy, were excluded.
Statistical analysis
This case-control had two outcome groups. Patients that received vitrectomy versus patients that received clinic procedural management only (IVI, PRP). Each group was further segmented into patient encounters that were considered pre-COVID-19 era (January 2018-February 2020) and COVID-19 era (March 2020-March 2021) to compare changes in follow-up behavior across the pandemic shutdown within each group and between each group.
The chi-square tests compared initial ETDRS (Early Treatment of Diabetic Retinopathy Study) DR diagnosis prevalence, rescheduling rate (patient or clinic-directed removal of planned encounter with advance notice), and no-show rates (patient-directed cancellation without advance notice). Two-tailed t-tests compared intervals between consecutive completed appointments and intervals between ETDRS DR stage progressions. A multivariate logistic regression was used to study the outcome of need for vitrectomy based on appointment behavioral factors of rescheduling rate, no-show rate, total appointments (burden of visits), variation in appointment intervals. Regression factors used that were related to disease severity were initial ETDRS DR stage, traction retinal detachment (TRD), vitreous hemorrhage (VH), stable PDR. Alpha was set at 0.05 and regression classification cutoff at 0.5.
Results
Patients and disease severity
Of 1,194 patients, 739 had at least four completed visits in the study period and were included in the analysis. Of which, 202 patients were sorted into the vitrectomy group and 537 in the nonvitrectomy group (
Table 1). At the initial encounter, the vitrectomy versus nonvitrectomy group had 3% versus 17% moderate NPDR, 3% versus 14% severe NPDR, and 94% versus 69% PDR, respectively. The vitrectomy versus nonvitrectomy group had a VH occurrence during the study period in 15% versus 2%, TRD in 8% versus 2%, and stable PDR in 5% versus 6%, respectively.
Change in appointment characteristics
The total number of procedures related to PDR disease declined in the first 2 months following the onset of COVID-19 before rebounding in the following two quarters (
Fig. 1). In the pre-COVID-19 era, the mean interval (±1 standard deviation) between patient visits was 29.76 ± 45.11 days in the vitrectomy group and 40.23 ± 56.73 days in the nonvitrectomy group (
p < 0.001) (
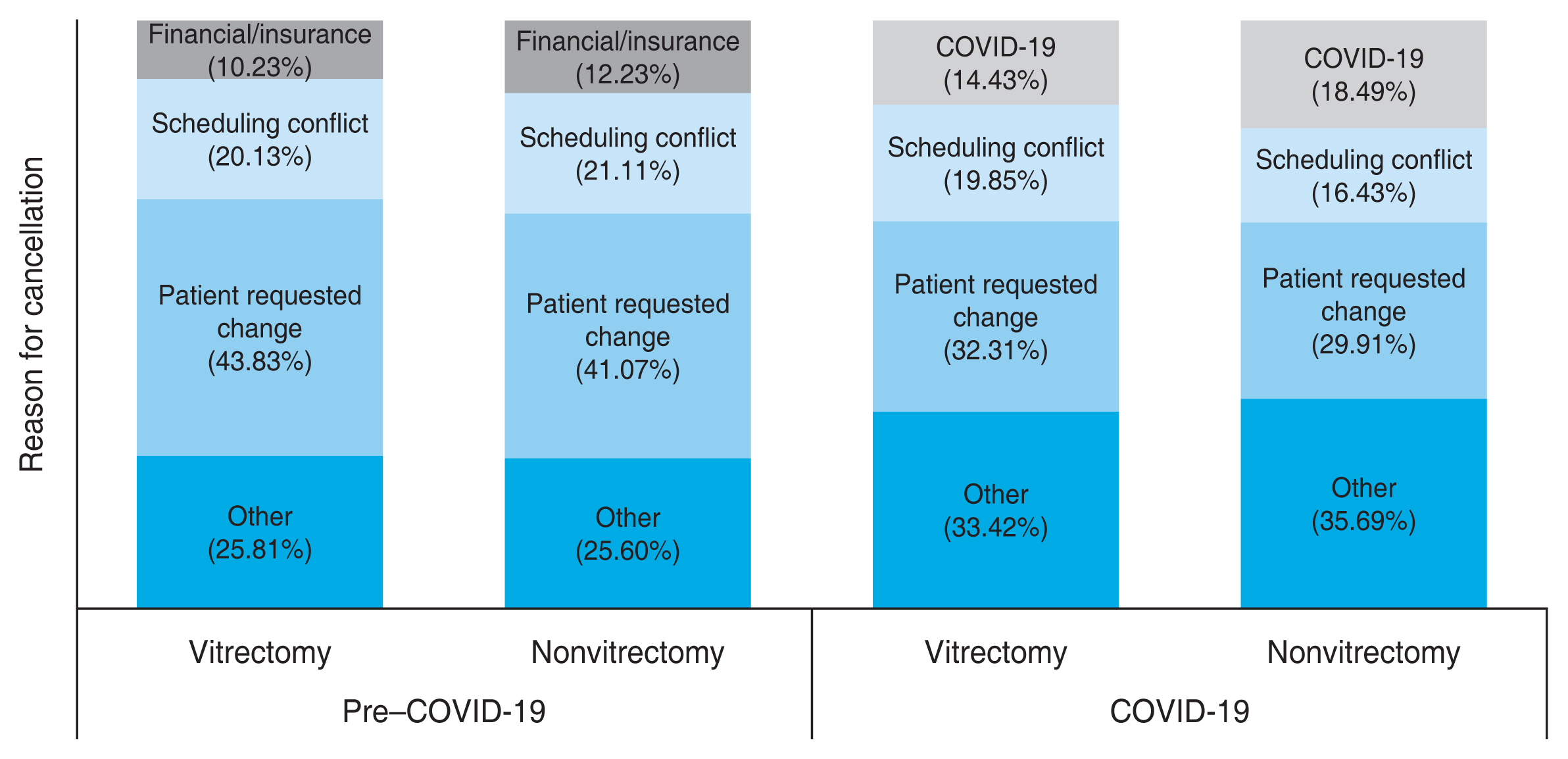
Table 2). After the COVID-19 shutdown, there was a statistically significant increase in the appointment intervals in both groups with a larger increase in the vitrectomy group. There was a corresponding statistically significant increase in the reschedule and no-show rate in the vitrectomy and nonvitrectomy groups after the onset of COVID-19. The reschedule rate increased by about 8% in both groups, with COVID-19 becoming one of the top three reasons for cancellations in both groups (
Fig. 2). There was a smaller increase in the no-show rate of around 1% in both groups, statistically significant in the vitrectomy group.
Disease progression
Between consecutive completed visits, 6% of the vitrectomy group and 20% of the nonvitrectomy group had ETDRS DR progression, respectively. In the vitrectomy group, five patients (2.5%) had a two-step ETDRS DR progression at 253 ± 222 days before COVID-19 and 691 ± 0 days after COVID-19. One patient (0.5%) had one-step ETDRS DR progression from moderate to severe disease. Six patients (3.0%) had a one-step ETDRS DR progression from severe to proliferative disease at 195 ± 217 days before COVID-19 and 357 ± 0 days after COVID-19. In the nonvitrectomy group, 45 patients (8.4%) had a two-step progression at 210 ± 205 days before COVID-19 and 559 ± 300 days after COVID-19. Twelve patients (2.2%) had a one-step progression from moderate to severe disease at 149 ± 163 days and 53 (9.9%) had a one-step progression from severe to proliferative disease at 226 ± 209 days before COVID-19 and 609 ± 392 days after COVID-19 (
Table 3).
Regression of variables leading to vitrectomy
The presence of TRD conveyed the highest risk of eventual vitrectomy with an odds ratio (OR) of 5.36, followed by ETDRS DR stage (OR, 2.90) and presence of VH (OR, 2.59). Attendance behavior analysis showed total number of visits (visit burden on patient) and appointment interval variability (reflecting intermittent loss to follow-up) both had an OR of 1.02. Increased number of visit-reschedules (through increased patient touchpoints) and shorter visit intervals decreased the odds of vitrectomy with OR of 0.03 and 0.95 (
Table 4). No-show rate and history of stable PDR were not statistically significant.
Discussion
In the first 2 months upon resuming clinics post-COVID-19, we saw our procedural volume for PDR treatment decrease by 11% (anti-VEGF, 7%; PRP, 18%; vitrectomy, 6%) which was proportionally a smaller change than our total clinic volume reduction of 47% for all ophthalmic subspecialties, a trend similar to other institutions [
3,
4]. We became interested in whether our COVID-19-related triaging or patient follow-up behavior had an unforeseen impact on DR complications that would lead to surgical management. Our study evaluated the difference between two PDR patient groups that had the end point of either vitrectomy or nonsurgical procedural management after the shutdown of clinics starting in March 2020. For each group, we assessed follow-up behavior linked to delay of care as well as disease factors linked to proliferative complications from before to after clinic shutdown.
The follow-up variables were rescheduling rate, no-show rate, and intervals between appointment for the two groups before and after clinic shutdown. A reschedule was initiated either by clinic-directed triaging or by the patient request to be rescheduled later resulting in an increased duration between patient visits (increased interval) either way but likely to a varying amount based on whether the provider or patient directed the rescheduling.
The intervals between appointments significantly increased for both groups, 12 days (range, 40.2-52.4 days) for the nonvitrectomy group compared to the 16 days (range, 29.8-46.2 days) in the vitrectomy group. The delay in the vitrectomy group proportionally was 55% longer (vs. 30% for nonvitrectomy) which may reflect a proportionally higher impact on a group that may have already needed more frequent touchpoints. Patients initially with NPDR from either group saw progression of ETDRS diabetic retinopathy staging at 2 to 8 months pre-COVID-19 and 17 to 20 months in COVID-19 era (
Table 3), which may reflect detection of progression later than intended due to fewer touchpoints. Similarly, Forster et al. [
11] reported an OR of 1.3 and 3.76 of sight-threatening diabetic retinopathy for patients who miss 1 and 2 years of appointments, respectively.
No-shows were unanticipated by the clinic and resulted in delay in follow-up against the triage clinical logic. Surprisingly, both groups had an increase in no-show rate that was minimal in magnitude across the shutdown so was not a big influence in care delay difference between the two groups. Post-COVID-19, the rate of no-show was only one-third of the rescheduling rate so the delay in care was likely driven dominantly by clinic-led or patient-initiated triages (
Table 2). However, 77% and 80% of rescheduled visits were requested by the patient in the vitrectomy and nonvitrectomy group, respectively, which meant patient-initiated triage drove the majority of the delay. When weighing in no-shows, patient self-triage accounted for 83% to 85% of delayed visits for each groups. Interestingly, the vitrectomy group had more severe or unstable disease initially (vitrectomy group, 93.6% PDR vs. nonvitrectomy group, 69.5% PDR) but compared to the nonvitrectomy group had a similar appointment completion rate, rescheduling rate, no-show rate, and even longer interval delays suggesting the more severe or unstable group were not any better at self-triaging despite having more proliferative complications.
Our logistic regression found that disease factors outweighed clinic attendance factors for needing future vitrectomy (
Table 4). Factors reflective of more severe or unstable PDR had the highest OR of leading to a vitrectomy: diagnosis of TRD, initial ETDRS DR stage, and incidence of VH. Appointment interval variability and total visit burden were appointment factors that also increased the odds of eventual vitrectomy. We used interval variability as a signal of a loss to follow-up at some point where larger lapses produce larger variations. The number of total visits was used as an indicator of visit burden as many of these patients may have competing appointments from other specialties. Both factors were much less impactful than disease factor that reflect unstable PDR. The regression shows that patients who rescheduled and those who had shorter visit intervals had lower odds of needing vitrectomy which may be explained by patients who were rescheduled by the clinic and triaged appropriately to not allow long intervals between appointments. The trend is supported by
Table 2 which demonstrate that the vitrectomy group had proportionally more prolonged intervals.
Dar et al. [
9] reported that initially 55% of patients were worried of contracting the disease though 57% felt their ocular condition was important enough to risk exposure. However, the visually impaired segment may have a heightened perception of the pandemic and so were disproportionately affected [
10]. In our study, both groups cited COVID-19 as one of the top three reasons for rescheduling at similar rates of 14% to 18% despite differing in DR severity (
Fig. 2). Our data suggest that patients who needed vitrectomy for proliferative complications self-triaged their appointments similarly to those stably managed in clinic despite having more severe disease, leading to proportionally more delayed care. The implication is that patients with more advanced DR and unstable disease will need more clinician guidance when requesting to be rescheduled. The mechanisms of clinician verification will need to weigh in practicality for both patients and clinicians and warrant further investigation.
Our study has limitations, including its retrospective nature, limited duration, and limited patient-specific data, such as age, sex, and visual acuity of affected eyes. Our data could still underestimate the rate of vision-threatening diabetic retinopathy complications requiring surgery due to the short post-COVID-19 study period. Surgical intervention is a surrogate measure of more active PDR than clinically managed patients, which is generally true at our institution but the decision for surgery varies between surgeons and institutions. Additional limitations include accuracy and granularity of CPT and ICD-10 codes, and technician dependent accuracy of recording reasons for rescheduling. The query system could not pull patient-specific data such as age, gender, or visual acuity of affected eye or fellow eye so these variables were not able to be analyzed. Future studies should consider analyzing these variables for detailed analysis of disease severity and monocularity, which are important factors for surgical decisions. Our findings highlight the need to better understand patient self-triaging behavior and to develop more effective triaging systems to minimize the impact of delays in clinical care.






 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print




