 |
 |
| Korean J Ophthalmol > Volume 37(3); 2023 > Article |
|
Abstract
Purpose
To investigate the effect of order of examination on the results of noninvasive keratograph tear film evaluation using Keratograph5M in dry eye patients.
Methods
One hundred and four patients with dry eye symptoms were analyzed retrospectively. All patients underwent bilateral noninvasive tear film evaluation using measurements of tear meniscus height (TMH) and noninvasive keratograph break-up time (NIKBUT) obtained using Keratograph5M. Measurements were performed sequentially in the order of right TMH, left TMH, right NIKBUT, and left NIKBUT.
Results
There was no statistically significant difference in TMH values between the right and left eyes (0.24 ┬▒ 0.08 and 0.23 ┬▒ 0.08 mm, respectively). Mean NIKBUT-first (time at first tear film break-up) and mean NIKBUT-average (the mean of all tear film break-up time over the entire cornea) were 6.17 ┬▒ 3.28 and 10.00 ┬▒ 3.97 seconds, respectively, for right, and 7.43 ┬▒ 3.86 and 11.57 ┬▒ 4.34 seconds, respectively, for left eyes. In addition, mean NIKBUT-first between right and left eyes, and mean NIKBUT-average between them were statistically significant (p = 0.013 and p = 0.007, respectively). Mean NIKBUT and mean TMH differences were not significantly influenced by right or left eyes, age, or sex (all p > 0.050). Spearman correlation analyses of TMH, NIKBUT-first, and NIKBUT-average results showed moderate positive correlations between right and left eyes (r = 0.470, r = 0.322, and r = 0.576, respectively; p < 0.001).
Conclusions
TMH evaluation was not affected by test order; however, NIKBUT measurement was affected by test order, because of reflex tearing due to forced eye opening during the examination. Therefore, TMH should be evaluated before NIKBUT, and sufficient time interval and caution should be needed between NIKBUT measurements on both eyes.
Dry eye disease is a multifactorial condition affecting the ocular surface, characterized by disrupted tear film homeostasis and associated ocular symptoms; etiological factors include tear film instability, hyperosmolarity, ocular surface inflammation and damage, as well as neurosensory abnormalities [1]. Traditionally, tear film stability is assessed by fluorescein strip instillation without topical anesthesia, and time to first tear film break-up is measured after complete blinking [2,3], and this examination induces destabilization of the tear film by the fluorescein strip [4]. However, several new devices have been developed to evaluate tear film stability more accurately. Videomeniscometry, and optical coherence tomography have both been used to evaluate tear meniscus stability [5,6], and tear film break-up times also can be assessed noninvasively by videokeratography, using the Keratograph5M (K5M; Oculus Optikger├żte GmbH). Wang and Craig [7] suggested that the noninvasive keratography is better at diagnosing dry eye than the conventional fluorescein method. Many noninvasive techniques have enabled to evaluate exact assessment on tear stability; however, it is important how to measure it. For example, Koh et al. [8] reported that forced eye opening, which is required for the noninvasive tear stability examination, influenced the tear meniscus height (TMH) measurement due to reflex tear secretion. Therefore, in this study, we investigated the effect of the order of noninvasive keratograph tear film evaluation using K5M in dry eye patients.
This study followed the tenets of the Declaration of Helsinki. The study protocol was approved by the Institutional Review Board of Inha University Hospital (No. 2018-09-018). The requirement for informed consent was waived due to the retrospective nature of the study.
All patients in this study were Koreans aged 20 to 80 years. Patients with dry eye disease were recruited from outpatients who visited the Department of Ophthalmology at Inha University Hospital from November 2016 to February 2017 for the management of dry eye symptoms. All patients enrolled met the Korean Corneal Disease Study Group guidelines for the diagnosis of dry eye disease: the presence of dry eye symptoms, Schirmer test (Ōēż10 mm after 5 minutes), tear film break-up time (Ōēż10 seconds) and the presence of conjunctival and corneal fluorescein staining scores of Ōēź2 [9].
The data of 104 patients with dry eye symptoms that registered at our dry eye clinic were analyzed retrospectively. Patients less than 20 years old, and those with a history of ocular surgery within 6 months, ocular injury, or another ocular disease were excluded.
All patients underwent a bilateral noninvasive keratograph tear film evaluation, including TMH and noninvasive keratograph break-up time (NIKBUT) using K5M before other examinations for dry eye disease. In the dry eye clinic, we requested the patients not to use any eye drops at least 2 hours before eye examination for accurate evaluation. Therefore, patients that used eye drops, including artificial tears, suspected not to apply t hem within at least 2 hours K5M testing.
To assess lower TMHs with K5M, the device was set to ŌĆ£tear film (TF) scan - tear meniscus modeŌĆØ to capture an image of the ocular surface with focus on the tear film. TMH was measured perpendicular to the lid margin at the central point relative to the pupil center using the tool supplied with the instrument, according to the manufacturerŌĆÖs instructions and as previously described [10-12]. During the test, patients were not required to open eyes widely or hold the upper eyelid.
ŌĆ£TF scan - NIKBUT modeŌĆØ was conducted by asking patients to blink three or four times and then maintaining their eyes open for as long as possible. During the test, 22 mire rings were projected on the corneal surface. More than 1,000 measurements were taken per ring which resulted in 22,000 analyzed data points per frame. Irregularities on images indicated instability or break-up of the TF. Simultaneously, a video was recorded for up to 25 seconds or the patientŌĆÖs next blink. The instrument provided a representation of TF break-up over time and provided a TF map showing the locations and sizes of TF break regions the first TF break-up time (time at first TF break-up, NIKBUT-first) and the average TF break-up time (the mean of all TF break-up times over the entire cornea, NIKBUT-average), as previously described [13-16]. Measurements were performed in the order of right eye TMH, left eye TMH, right eye NIKBUT, and left eye NIKBUT. All measurements were obtained in a temperature and humidity-controlled examination room by one experienced examiner.
Statistical analysis was performed using IBM SPSS ver. 20.0 (IBM Corp), and p-values less than 0.05 were considered significant. The Shapiro-Wilk test was used to check normality, except for NIKBUT-average result, all variables departed significantly from normality. Therefore, the Mann-Whitney U-test was used to compare TMH and NIKBUT values. Spearman rank correlation coefficient was used to analyze the correlation between TMH and NIKBUT values, and simple linear regression analysis to analyze the correlations between age and eye-to-eye difference of TMH and NIKBUT values.
A total of 104 patients with dry eye symptoms were included in the study. Mean patient age was 46.7 ┬▒ 15.3 years (range, 24-76 years), and 72 patients (69.2%) were female (Table 1).
Table 2 summarizes comparisons of TMH, NIKBUT-first, and NIKBUT-average values for right and left eyes. There was no statistically significant difference in TMH values between the right and left eyes (0.24 ┬▒ 0.08 and 0.23 ┬▒ 0.08 mm, respectively; p = 0.474), and the mean TMH difference (╬öTMH) was ŌłÆ0.01 ┬▒ 0.08 mm.
Mean value of NIKBUT-first and NIKBUT-average were 6.17 ┬▒ 3.28 and 10.00 ┬▒ 3.97 seconds, respectively, for right eyes, and 7.43 ┬▒ 3.86 and 11.57 ┬▒ 4.34 seconds, respectively, for left eyes. The mean NIKBUT-first and NIKBUT-average differences between right and left eyes were 1.26 ┬▒ 4.27 and 1.57 ┬▒ 3.82 seconds, respectively. Both values were significantly higher for left eyes which measured later (p = 0.013 and p = 0.007, respectively). No significant correlation was found mean difference TMH, NIKBUT-first, and NIK BUT-average values with sex (p = 0.092, p = 0.772, and p = 0.422, respectively) and age (p = 0.294, p = 0.601, and p = 0.604, respectively).
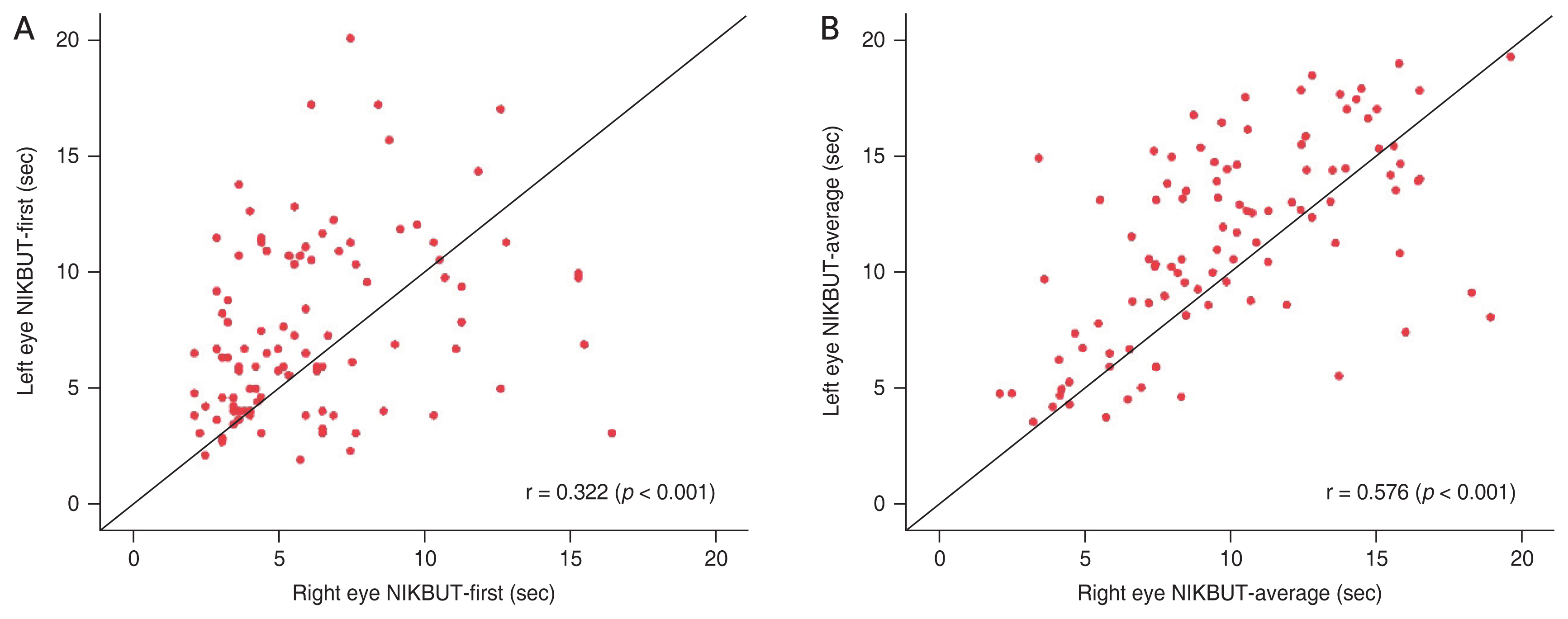
Spearman correlation analysis showed a moderate positive correlation between the TMH values of right and left eyes (r = 0.470, p < 0.001) (Fig. 1). For NIKBUT-first and NIKBUT-average, moderate positive correlations were observed right eyes (examined first) and left eyes (r = 0.322 and r = 0.576, respectively; both p < 0.001) (Fig. 2A, 2B). In patients with a right eye NIKBUT-first value of less than 5 seconds, the proportion of cases with a higher left eye NIKBUT-first value was 80.9%. In patients with a right eye NIKBUT-average of less than 7 seconds, the proportion of cases with higher left eye value was 82.6%.
The purpose of this study was to investigate the effect of order of examination on the results of noninvasive keratograph TF evaluation using K5M. First, the order of TMH examination had no significant effect on eye-to-eye TMH differences. Tear meniscus contains 75% to 90% of tear volume [17], which is positively correlated with lacrimal secretory rate [18], and thus TMH is an informative diagnostic parameter for aqueous-deficient dry eye [19]. Many studies support this idea. In a study by Lim and Lee [20], TMH with fluorescein was 0.19 ┬▒ 0.05 mm in normal patients and 0.10 ┬▒ 0.04 mm in dry eyes, and there was a significant difference in two groups. TMH measurement with real-time optical coherence tomography also showed that TMH was smaller in dry eye patients than in healthy subjects. According to Shen et al. [21], upper TMHs were 0.174 ┬▒ 0.018 and 0.171 ┬▒ 0.021 mm for right and left, respectively, in normal patients and 0.148 ┬▒ 0.019 and 0.143 ┬▒ 0.019 mm for right and left, respectively, in dry eyes. Also, lower TMHs were 0.196 ┬▒ 0.023 and 0.190 ┬▒ 0.024 mm for right and left, respectively, in normal patients and 0.143 ┬▒ 0.024 and 0.141 ┬▒ 0.024 mm for right and left, respectively, in dry eyes [21]. Koh et al. [8] reported that there was no significant difference between TMH measurements obtained at 2-minute intervals in both normal group and dry eye group. Therefore, TMH measurement using K5M is less affected by test order and shows good repeatability.
In this study, NIKBUT-first and NIKBUT-average values using K5M were significantly different between right (first examined) and left eyes, and mean NIKBUT of left eyes was greater than those of right eyes. We speculated that as subjects were forced to keep eyes open for NIKBUT measurements, this resulted in reflex tearing in the other side. In addition, those with a lower NIKBUT value, indicating tear film instability, were more affected. Similar to our results, Koh et al. [8] reported the baseline TMH values (measured without NIKBUT testing) of dry eye group and normal group were 0.14 ┬▒ 0.03 and 0.20 ┬▒ 0.05 mm, respectively. In both groups, significant increases in TMH values were observed with the NIKBUT measurement. Furthermore, a negative correlation was observed between ╬öTMH and baseline TMH values (r = ŌłÆ0.44, p = 0.03) in only dry eyes, indicating subjects with severe dry eye were more affected by reflex tearing. They concluded that forced eye opening for NIKBUT measurements influences the TMH measurements, and therefore TMH should be evaluate before the NIKBUT assessments. Previous studies also showed that the tear meniscus changed significantly during delayed blinking [22-25]. Cui et al. [25] visualized precorneal tear films using ultra-high resolution optical coherence tomography in dry eye patients during normal blinking and delayed blinking. According to the study, the averaged of precorneal tear film was 4.4 ╬╝m during normal blinking, and the precorneal tear film thickness was significantly increased to 6.6 ╬╝m (standard deviation, 2.9 ╬╝m; p < 0.05) during delayed blinking in dry eye patients. They showed that precorneal tear films were thicker during delayed blinking compared with normal blinking because of reflex tearing.
Tear film break-up time (TBUT) are traditionally used to diagnose dry eye. However, TBUT values are affected by the amount of fluorescein dye used, and thus, results different between clinicians [26,27]. Also, applying the fluorescein strip induces reflex tearing on the ocular surface [28,29]. To increase sensitivity and accuracy, a TF stability analysis system (TSAS), a videokeratography system, and K5M were introduced as noninvasive methods for TF stability analysis [30], and the K5M has been reported to produce highly repeatable and reproducible TMH and NIKBUTs value for healthy subjects and patients with dry eye disease (coefficient of variation Ōēż26.1% and intraclass correlation coefficient Ōēź0.75) [31]. However, our results suggest that noninvasive methods can also induce reflex tearing when subjects keep eyes open for K5M testing. Koh et al. [8] emphasized that TMH testing should be conducted before any test requiring forced eye opening, such as NIKBUT testing. Therefore, sufficient time interval and attention should be required before testing, the other eye to prevent reflex tearing affecting results.
This study was conducted retrospectively and has a limitation in that it could not compare the effect of test order in a normal control group. However, by the previous studies [8,22-25], delayed blinking or forced eye opening increased the induction of reflex tearing in dry eyes than in normal eyes. Therefore, in especially dry eyes, sufficient time interval should be needed before testing.
We investigated the effect of order of examination on the results of noninvasive keratograph TF evaluation using K5M in dry eye patients. TMH evaluation was not affected by test order, however NIKBUT measurement was affected by test order, because of reflex tearing due to forced eye opening during the examination. Therefore, TMH should be evaluated before NIKBUT, and sufficient time interval and caution should be needed between NIKBUT measurements on both eyes.
References
1. Craig JP, Nichols KK, Akpek EK, et al. TFOS DEWS II definition and classification report. Ocul Surf 2017;15:276-83.


2. Jacobi C, Cursiefen C. Ophthalmological complications in SjogrenŌĆÖs syndrome. Z Rheumatol 2010;69:32-40.



3. Messmer EM. The pathophysiology, diagnosis, and treatment of dry eye disease. Dtsch Arztebl Int 2015;112:71-81.



4. Mengher LS, Bron AJ, Tonge SR, Gilbert DJ. A non-invasive instrument for clinical assessment of the pre-corneal tear film stability. Curr Eye Res 1985;4:1-7.


5. Doughty MJ, Laiquzzaman M, Button NF. Video-assessment of tear meniscus height in elderly Caucasians and its relationship to the exposed ocular surface. Curr Eye Res 2001;22:420-6.


6. Jeon SJ, Baek JW, Doh SH, Chung SK. Tear meniscus evaluation using optical coherence tomography in meibomein gland dysfunction patients. J Korean Ophthalmol Soc 2015;56:1684-91.

7. Wang MT, Craig JP. Comparative evaluation of clinical methods of tear film stability assessment: a randomized crossover trial. JAMA Ophthalmol 2018;136:291-4.



8. Koh S, Ikeda C, Watanabe S, et al. Effect of non-invasive tear stability assessment on tear meniscus height. Acta Ophthalmol 2015;93:e135-9.


9. Hyon JY, Kim HM, Lee D, et al. Korean guidelines for the diagnosis and management of dry eye: development and validation of clinical efficacy. Korean J Ophthalmol 2014;28:197-206.



10. Abdelfattah NS, Dastiridou A, Sadda SR, Lee OL. Noninvasive imaging of tear film dynamics in eyes with ocular surface disease. Cornea 2015;34:Suppl 10. S48-52.


11. Lee KW, Kim JY, Chin HS, et al. Assessment of the tear meniscus by strip meniscometry and keratograph in patients with dry eye disease according to the presence of meibomian gland dysfunction. Cornea 2017;36:189-95.


12. Arriola-Villalobos P, Fernandez-Vigo JI, Diaz-Valle D, et al. Assessment of lower tear meniscus measurements obtained with Keratograph and agreement with Fourier-domain optical-coherence tomography. Br J Ophthalmol 2015;99:1120-5.


13. Kim J, Kim JY, Seo KY, et al. Location and pattern of non-invasive keratographic tear film break-up according to dry eye disease subtypes. Acta Ophthalmol 2019;97:e1089-97.



14. Jiang Y, Ye H, Xu J, Lu Y. Noninvasive Keratograph assessment of tear film break-up time and location in patients with age-related cataracts and dry eye syndrome. J Int Med Res 2014;42:494-502.



15. Jung JW, Kim JY, Chin HS, et al. Assessment of meibomian glands and tear film in post-refractive surgery patients. Clin Exp Ophthalmol 2017;45:857-66.



16. Lee R, Yeo S, Aung HT, Tong L. Agreement of noninvasive tear break-up time measurement between Tomey RT-7000 Auto Refractor-Keratometer and Oculus Keratograph 5M. Clin Ophthalmol 2016;10:1785-90.


17. Holly FJ. Physical chemistry of the normal and disordered tear film. Trans Ophthalmol Soc U K 1962 1985;104(Pt 4):374-80.

18. Mishima S, Kubota Z, Farris RL. The tear flow dynamics in normal and keratoconjunctivitis sicca cases. Excerpta Medica Int Congr Ser 1970;222:1801-5.
19. Mainstone JC, Bruce AS, Golding TR. Tear meniscus measurement in the diagnosis of dry eye. Curr Eye Res 1996;15:653-61.


20. Lim KJ, Lee JH. Measurement of the tear meniscus height using 0.25% fluorescein sodium. Korean J Ophthalmol 1991;5:34-6.


21. Shen M, Li J, Wang J, et al. Upper and lower tear menisci in the diagnosis of dry eye. Invest Ophthalmol Vis Sci 2009;50:2722-6.


22. Yuan Y, Wang J, Chen Q, et al. Reduced tear meniscus dynamics in dry eye patients with aqueous tear deficiency. Am J Ophthalmol 2010;149:932-8.



23. Palakuru JR, Wang J, Aquavella JV. Effect of blinking on tear dynamics. Invest Ophthalmol Vis Sci 2007;48:3032-7.


24. Li J, Shen M, Wang J, et al. Clinical significance of tear menisci in dry eye. Eye Contact Lens 2012;38:183-7.


25. Cui L, Wang J, Perez VL, et al. Visualization of the precorneal tear film using ultrahigh resolution optical coherence tomography in dry eye. Eye Contact Lens 2012;38:240-4.



26. Bron AJ, de Paiva CS, Chauhan SK, et al. TFOS DEWS II pathophysiology report. Ocul Surf 2017;15:438-510.


27. Norn MS. Desiccation of the precorneal film. I. Corneal wetting-time. Acta Ophthalmol (Copenh) 1969;47:865-80.

28. Garcia-Resua C, Santodomingo-Rubido J, Lira M, et al. Clinical assessment of the lower tear meniscus height. Ophthalmic Physiol Opt 2009;29:487-96.

29. Lam AK, Tai SK, Chan JK, Ng RW. Lower tear meniscus height measurements using keratography and swept-source optical coherence tomography and effect of fluorescein instillation methods. Curr Eye Res 2019;44:1203-8.


Fig.┬Ā1
Scatterplot showing correlations between tear meniscus height (TMH) of right and left eyes, as determined using Spearman rank correlation. A moderate positive correlation was observed (r = 0.470, p < 0.001).

Fig.┬Ā2
Scatterplots showing correlations between noninvasive Keratograph break-up time (NIKBUT) of right and left eyes, as determined using Spearman rank correlation. (A) A moderate positive correlation was observed between the time at first tear film break-up (NIKBUT-first) of right and left eyes (r = 0.322, p < 0.001). (B) A moderate positive correlation was observed between the mean of all tear film break-up times over the entire cornea (NIKBUT-average) of right and left eyes (r = 0.576, p < 0.001).
Table┬Ā1
Demographic data and ocular surface status parameters in dry eyes (n = 104)
Table┬Ā2
Comparison of noninvasive Keratography tear film results for right (tested first) and left eyes (shown in measurement order)
- TOOLS



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print




