Dear Editor,
The recent COVID-19 pandemic, caused by infection from the SARS-COV-2, has affected more than 328 million people and is responsible for more than 5 million deaths worldwide from 2019 to January 2022 [
1]. COVID-19 patients may have a number of complex and varied coagulation abnormalities that induce a hypercoagulable state and provoke venous thromboembolism, a condition called COVID-19-associated coagulopathy [
2]. In fact, COVD-19 appears to also affect the retina, with the most common retinal manifestations involving microvascular changes such as cotton wool spots and retinal microhemorrhages [
3]. Thus, retinal vein occlusions (RVO) in COVID-19 patients can be associated with this hypercoagulable state. Herein, we report a case of central RVO (CRVO) in a young teenage girl with COVID-19. Written informed consent for publication of the research details and clinical images was obtained from the patient.
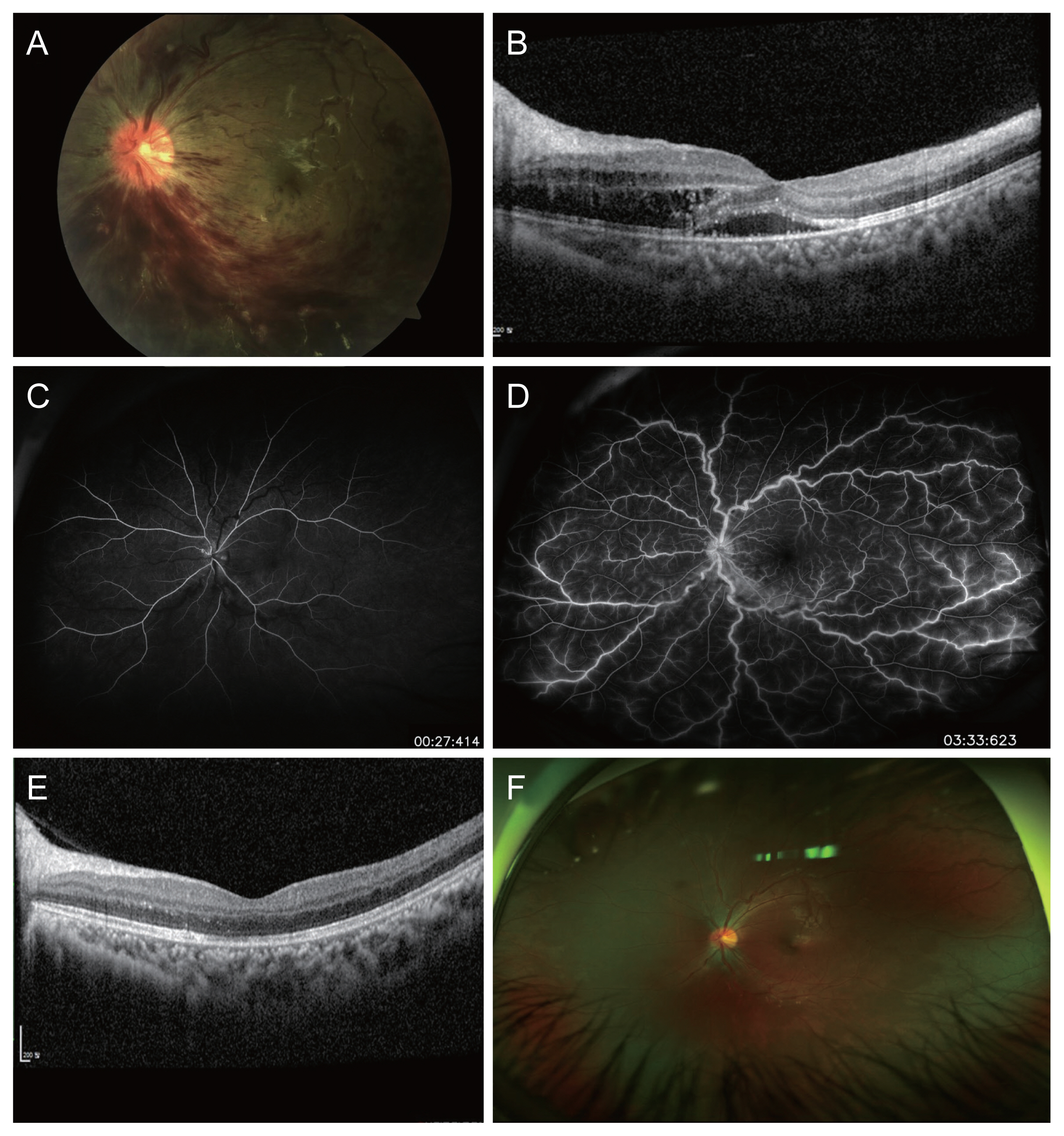
A 13-year-old girl presented with decreased vision in her left eye for 13 days. Her past medical history was unremarkable, except for COVID-19 infection, with which she was diagnosed 16 days before the onset of ocular symptoms. Her best-corrected visual acuity was 20/25 in the right eye and 20 / 63 in the left eye. Her intraocular pressures were 20 and 17 mmHg in the right and left eyes, respectively. Anterior segment findings were within normal limits in both eyes. Fundus findings in her right eye was unremarkable. The left eye fundus showed multiple retinal hemorrhages with optic disc edema and dilated tortuous vessels in all quadrants (
Fig. 1A). Optical coherence tomography (OCT) showed macula edema with subretinal fluid and a central foveal thickness of 397 ╬╝m (
Fig. 1B). Fluorescein angiography showed marked delay in arteriovenous transit time and staining of the dilated tortuous veins (
Fig. 1C, 1D). Based on these clinical findings, the patient was diagnosed with nonischemic CRVO, with possible association with COVID-19. A full diagnostic workup, including blood pressure measurement, complete blood count and hypercoagulability tests with peripheral blood smears, tests for homocysteine, anti-DNA, ELISA, anti-╬▓ 2 glycoprotein 1 (anti-╬▓2GP1) immunoglobulin G (IgG), anti-╬▓2GP1 IgM, anti-cyclic citrullinated peptide antibody, cholesterol, and anticardiolipin antibodies IgM and IgG, were unremarkable, except for positive antinuclear antibody. After 2 monthly intravitreal anti-vascular endothelial growth factor injections in the left eye, her visual acuity improved to 20 / 40 and OCT showed resolution of macula edema (
Fig. 1E, 1F), with resolution of flame-shaped hemorrhage and decreased vascular tortuosity on fundus examination.
CRVO typically occurs in elderlies and far less commonly in healthy teenagers. Our 13-year-old patient did not have major risk factors of CRVO, including diabetes mellitus, hypertension, hypercoagulability, atherosclerosis, and vasculitis secondary to systemic inflammation, except that she had recently been diagnosed with COVID-19 approximately 2 weeks before the onset of visual symptoms. Although she had tested positive for antinuclear antibody (ANA), she did not have other symptoms or signs indicating autoimmune diseases including systemic lupus erythematosus, scleroderma, rheumatoid arthritis, Sj├ČgrenŌĆÖs syndrome or other rheumatic systemic diseases. Additionally, there was no family history related to autoimmune diseases, and a positive ANA can be seen in healthy individuals.
COVID-19-associated coagulopathy with venous thromboembolic disease have been described in many studies, including cerebral venous thrombosis in three young COVID-19 patients [
4], and autopsy findings of diffuse small vessel thrombosis in patients with severe COVID-19 [
5]. Excessive inflammation, platelet activation, endothelial dysfunction, and venous stasis have been suggested as the cause of arterial and venous circulation problems in COVID-19 patients. It is yet to be determined whether there is a direct causal relationship between CRVO and COVID-19, but the occurrence of the disease shortly after COVID-19 infection at such a young age in the absence of other systemic risk factors suggests that the prothrombotic state created by COVID-19 may have contributed to CRVO development in our patient. This case adds to the existing literature that there may be possible association in the occurrence of CRVO in the setting of COVID-19. As COVID-19 patients are at risk for vascular occlusive disease, patient education for retinal vascular complications and early detection with prompt treatment are imperative for visual prognosis.






 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print



