Analyses of Foveal Avascular Zone in Patients with General Blunt Ocular Trauma Using Optical Coherence Tomography Angiography
Article information
Abstract
Purpose
To investigate the effect of blunt ocular trauma (BOT) on foveal circulation, and in particular the foveal avascular zone (FAZ), using optical coherence tomography angiography (OCTA).
Methods
This retrospective study consisted of 96 eyes (48 traumatized eyes and 48 nontraumatized eyes) from 48 subjects with BOT. We analyzed the FAZ area of deep capillary plexus (DCP) and superficial capillary plexus (SCP) immediately after BOT and at 2 weeks after BOT. We also evaluated the FAZ area of DCP and SCP in patients with and without blowout fracture (BOF).
Results
There were no significant differences in FAZ area between traumatized and nontraumatized eyes at DCP and SCP in the initial test. In traumatized eyes, the FAZ area at SCP was significantly reduced on follow-up when compared to initial test (p = 0.01). In case of eyes with BOF, there was no significant differences in FAZ area between traumatized and nontraumatized eyes at DCP and SCP on initial test. No significant difference of FAZ area was found on follow-up relative to the initial test, whether in the DCP or SCP. In case of eyes without BOF, there was no significant differences of FAZ area between traumatized and nontraumatized eyes at DCP and SCP in initial test. Also, no significant difference of FAZ area at DCP was found on follow-up test compared to initial test. However, the FAZ area at SCP was significantly reduced in follow-up test compared with that in the initial test (p = 0.04).
Conclusions
Temporary microvascular ischemia occurs in the SCP of patients after BOT. Patients should be warned of transient ischemic changes that may occur after trauma. OCTA can provide useful information regarding the subacute changes in the FAZ at SCP after BOT, even without evident findings of structural damage on fundus examination.
Ocular trauma is a major cause of monocular blindness and visual impairment worldwide [1] and the World Health Organization has reported that globally 55 million people experience serious ocular trauma every year [2]. Blunt trauma was the most common type of ocular trauma [3] and frequently occurs in various situations such as industrial settings, traffic accidents, and assault. Complications that may occur after a blunt ocular trauma (BOT) include traumatic hyphema, commotio retinae, retinal tear, retinal detachment, retinal and vitreous hemorrhage, blowout fractures (BOF), and traumatic optic neuropathy (TON) [4]. If these complications occur, even minor trauma to eye can cause severe visual dysfunction and impairment. Proper evaluation and treatment are needed immediately after the trauma.
Posttraumatic retinal disorders have been described and were attributed to the disruption of choroidal circulation might cause outer retinal damage after BOT [5]. Retinal vascular occlusions secondary to BOT also have been reported [6–10]. According to Long et al. [11], oxygen consumption is increased in eyes after closed-globe BOT, suggesting that BOT may affect retinal circulation. Thus, retinal circulation after BOT is important, but there have only been few studies about the retinal vascular changes after BOT.
Optical coherence tomography angiography (OCTA) is a safe, rapid, noninvasive deep resolved imaging technique that provides en face visualization of the retinal vascular networks by detecting the blood flow in different retinal layers [12–14]. This tool allows for detailed analysis of retinal perfusion damage in macular and peripapillary regions even without evidence of retinal structural loss, such as in several optic neuropathies [15]. OCTA can detect early microcirculatory disturbance [16] and separately evaluate the superficial capillary plexus (SCP) and deep capillary plexus (DCP) in various regions. It also provides a detailed analysis of the foveal avascular zone (FAZ) [13,17], a special part of the retina that maximizes the optical quality of vision [18,19].
According to Montorio et al. [20], BOT can cause temporary reduction in retinal vessel density, which leads to impaired retinal blood perfusion. Retinal perfusion can be estimated indirectly from the FAZ area, and previous studies have reported that the FAZ area is altered by focal ischemia of the retina and retinal microcirculation impairment in patients with branch retinal vein occlusion [21] and diabetic retinopathy [22]. We hypothesized that the patients with BOT may have disturbances in retinal perfusion even without any structural damage. Thus, using OCTA, we can noninvasively evaluate changes in retinal blood perfusion after BOT by comparing the FAZ area between traumatized and nontraumatized eyes. We can also monitor changes over time. Here we focused on changes in posttraumatic retinal perfusion in the absence of structural damage immediately after trauma.
Materials and Methods
Ethical statements
The study was performed adherence with the tenets of the Declaration of Helsinki and was approved by the Institutional Review Board of Myoungji Hospital (No. 2021-07-051). The requirement for informed consent was waived due to the retrospective nature of the study.
Patient selection
This retrospective study evaluating imaging technology was conducted at Myongji Hospital from May 2019 to May 2021. The patients who visited the clinic immediately after or within 1 week after trauma and visited the clinic for follow-up 2 weeks after the initial visit were included. Patients who had high myopia (>6 diopters), amblyopia, prior history of systemic disease as diabetes, previous ocular trauma, previous ocular surgery, congenital eye disease, macular or vitreoretinal disease, glaucoma, presence of significant lens opacification, late visit over a week after trauma, or poor quality of OCTA images were excluded from the study. We also excluded patients with penetrating ocular trauma, choroidal rupture, traumatic macular holes, retinal tear or retinal detachment and binocular injured patients by considering changes in FAZ size between normal individuals.
Data collection
In all patients, a detailed history was obtained to determine the injury type, and the duration between injury and presentation. All patients underwent complete ophthalmic examination, including best-corrected visual acuity (BCVA), intraocular pressure, relative afferent pupillary defect, ocular movement, slit-lamp biomicroscopy, fundus examination, OCT, and OCTA imaging of the macula on both initial and follow-up visits.
OCTA image acquisition and analysis
All patients, retinal microvasculature was analyzed using a Nidek OCT instrument (RS-3000 Advance 2, Nidek) on both initial and follow-up visits. The RS-3000 spectral domain OCT uses a wavelength of 880 nm with a scan speed of 53,000 A-scans/sec. Scans with poor quality, defined by the following criteria, were excluded: signal quality index <2/5, signal strength index <7/10, poor clarity, residual motion artifacts visible as irregular vessel pattern on the en face angiogram, or off-center macula.
For each eye, a 3 × 3-mm scan centered on the fovea was acquired. OCTA images of the superficial and deep capillary networks were generated separately using the automated software algorithm. Based on the eight regional settings, the SCP layer was defined from the inner limiting membrane to 13 μm above the inner plexiform layer. The DCP layer was defined from 8 μm above the inner plexiform layer to 13 μm above the outer plexiform layer.
We analyzed FAZ area manually with ImageJ (US National Institutes of Health) after setting the scale to 800 × 800 pixels in 3 × 3-mm scan area same as previous study [23,24]. The FAZ area was separately calculated for the SCP area and DCP area and the maximum horizontal and vertical diameters of the FAZ were marked manually as shown in Fig. 1A–1F. All clinical information were masked, and the image analyses were performed independently by two ophthalmologists (LLW and JYL), and the average of the two values was recorded.

Analysis of optical coherence tomography angiography (OCTA) images of superficial capillary plexus (SCP) and deep capillary plexus (DCP) using ImageJ (US National Institutes of Health). Manual outlining of the border of foveal avascular zone. SCP OCTA images of (A) nontraumatized eye, (B) traumatized eye, and (C) traumatized eye 2 weeks after trauma. DCP OCTA images of (D) nontraumatized eye, (E) traumatized eye, and (F) traumatized eye 2 weeks after trauma.
Statistical analysis
Data were analyzed using IBM SPSS ver. 26 (IBM Corp). The FAZ area of traumatized eyes and nontraumatized eyes were compared using Wilcoxon signed rank test and the FAZ area immediately after trauma and 2 weeks after trauma were compared using paired t-test. The correlation of the difference in BCVA and the difference in SCP and DCP FAZ area between immediately after trauma and 2 weeks after trauma was analyzed using Pearson’s correlation test. Reliability analysis was performed by calculating intraclass correlation coefficient (ICC) and interobserver correlation coefficient between graders. A p-value of <0.05 was considered statistically significant. All results were presented as mean ± standard deviation.
Results
Demographics of the patients
Of the 64 patients (128 eyes) who met the inclusion criteria, the following were excluded: four (eight eyes) with binocular injury, eight (16 eyes) who visited the hospital a week after trauma, three (six eyes) had poor OCTA image quality, one subject (two eyes) had a history of glaucoma and retinal surgery. Therefore, 96 eyes from 48 subjects (38 male patients, 79.2%; 10 female patients, 20.8%) were included in the analysis (Fig. 2). The mean age of 48 patients was 40.69 ± 17.37 years. The 17 subjects were right eye injured and 31 subjects were left eye injured. A total of 48 traumatized eyes and 48 nontraumatized eyes were analyzed. Only 27 subjects (54 eyes) visited the hospital for follow-up. A total of 26 eyes (54.2%) were diagnosed as BOF. The mean BCVA of traumatized eyes was 0.06 ± 0.14 logarithm of the minimum angle of resolution (logMAR) at the initial visit and 0.02 ± 0.05 logMAR upon follow-up. The interval between the trauma and the initial visit was 2.46 ± 2.02 days (range, 0–7 days) and the interval between the initial visit and follow-up visit was 14.96 ± 4.66 days (range, 6–28 days). There were no patients with significant retinal and optic nerve complications such as TON or commotio retinae. Detailed demographics were presented in Table 1.
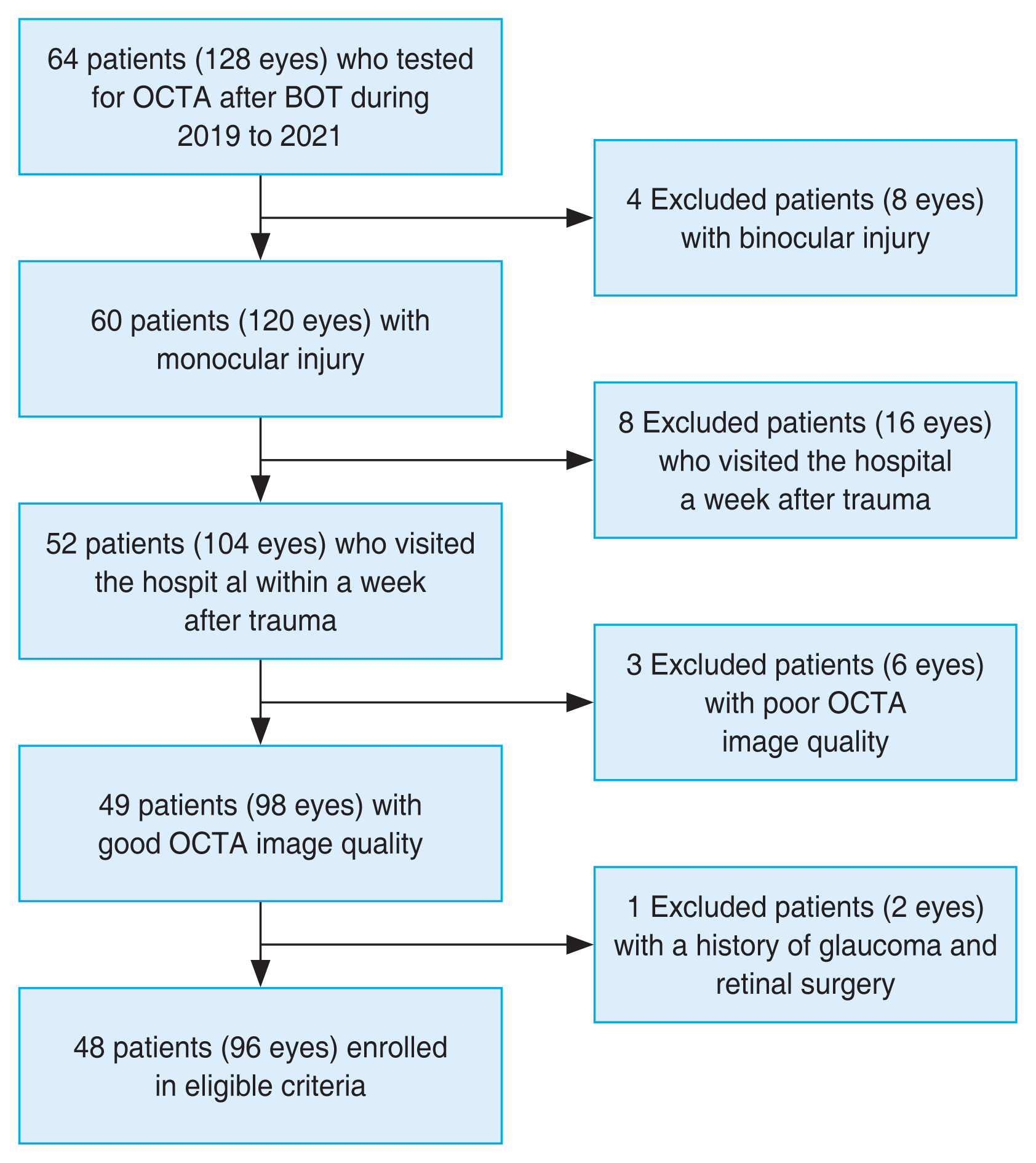
The process of identifying participants with blunt ocular trauma (BOT). OCTA = optical coherence tomography angiography.
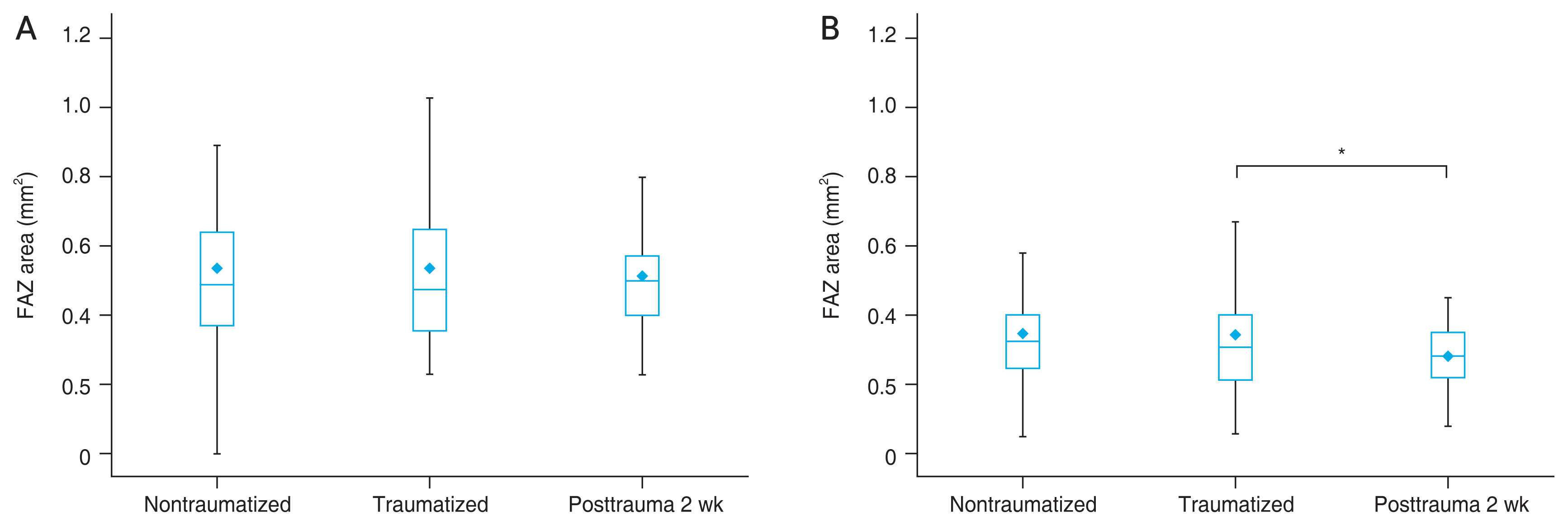
Comparisons of the FAZ area between traumatized eyes and nontraumatized eyes at the initial visit
The mean FAZ area of DCP in traumatized eye was 0.54 ± 0.21 mm2 and nontraumatized eye was 0.54 ± 0.20 mm2. The mean FAZ area of SCP in traumatized eye was 0.34 ± 0.13 mm2 and nontraumatized eye was 0.34 ± 0.12 mm2. There were no significant differences of FAZ area between traumatized and nontraumatized eyes at DCP ( p = 0.96) and SCP (p = 0.42) (Table 2).
Comparisons of the FAZ area between initial and follow-up visit in traumatized eyes
In traumatized eyes, the FAZ area at SCP was 0.34 ± 0.13 mm2 on initial visit and 0.30 ± 0.12 mm2 on follow-up visit. The FAZ area was significantly reduced on follow-up relative to the initial test (p = 0.013). There was no significant difference in size of the FAZ area in the DCP from initial visit (0.54 ± 0.21 mm2) to follow-up visit (0.53 ± 0.18 mm2, p = 0.197) (Table 2). The amount of FAZ areas between nontraumatized eyes, traumatized eyes, and 2 weeks after in traumatized eyes are presented in Fig. 3A and 3B. The correlation of the difference in BCVA and the difference in SCP and DCP area between immediately after trauma and 2 weeks after trauma was not statistically significant (p = 0.568 and p = 0.906, respectively). The excellent intrarater and interrater correlation was found for all measurement (ICC, 0.98 by LLW; ICC, 0.99 by JYL; ICC, 0.93 between LLW and JYL) [25].
Subset analysis: comparisons of the FAZ area between BOF eyes and non-BOF eyes
In the subset analysis, we further divided the subjects into eyes with and without BOF and again compared the FAZ area. In the 26 patients with BOF, there was no significant difference in size of FAZ area between traumatized and nontraumatized eyes whether in the DCP (p = 0.758) or in the SCP (p = 0.647). No significant difference in size of FAZ area was found on follow-up versus initial test at DCP (p = 0.326) and SCP (p = 0.162). In the 22 patients without BOF, there was no significant differences in FAZ area between traumatized and nontraumatized eyes at DCP (p = 0.661) and SCP (p = 0.444). Also, no significant difference of FAZ area was found between follow-up and initial in the DCP (p = 0.373). However, the FAZ area in the SCP was significantly reduced on follow-up compared to the initial (p = 0.043) (Table 2).
Discussion
In the present study, OCTA demonstrated significantly decreased SCP FAZ area in eyes with BOT 2 weeks after trauma. To date, many studies about ocular trauma have been conducted only on BOF or TON. There are few studies about the patients with simple BOT. However, BOT patients who do not have any evident findings on ophthalmic examination sometimes complain of discomfort, including self-reported blurred vision. We hypothesized that a transient subtle perfusion disorder may cause these symptoms. Many studies about posttraumatic retinal perfusion focused on patients with TON [26,27] and commotio retinae [20,28,29]. There are few studies about retinal perfusion in patients with simple BOT. Yalinbas Yeter et al. [30] studied retinal vascular changes and the FAZ area in BOT patients using OCTA. However, they only analyzed the retinal perfusion in patients immediately after trauma, so changes retinal perfusion over time was unknown. Therefore, we aimed to evaluate retinal perfusion by analyzing the FAZ changes in DCP and SCP over a 2-week period after BOT. Yalinbas Yeter et al. [30] found no difference in the FAZ area between the traumatized and nontraumatized eyes 24 hours post-BOT. This was consistent with our own findings. Only at 2 weeks posttrauma was there a significant reduction in FAZ area in the SCP. This indicated that FAZ area in the SCP may be an early and sensitive marker of subacute retinal changes due to trauma.
The mechanism for our findings can be explained by increased oxygen transport and vascular endothelial growth factor (VEGF) expression in the retina after BOT. The neurosensory retina might be stretched by the direct mechanical forces after BOT and this concussive force could be transmitted to the retinal vascular plexus, inducing a vasogenic response, which possibly causes arterial spasm and reduced blood flow [31–33]. These vascular alterations following the trauma, can leads to transient ischemic damage of the retina and leading to increased oxygen transport for retinal repair and clearance of impaired retinal tissue [11]. Previous studies have reported that regulation of retinal oxygenation affects the retinal capillary extent and function [34]. In particular, Petrou et al. [35] reported that the FAZ area reduced in vitrectomy patients due to increased oxygen transport in the ischemic retina. Furthermore, ischemic retina increases VEGF expression, which promotes retinal endothelial cell proliferation [36,37]. Consequently, it seems that increased oxygen transport and VEGF expression in the retina after BOT affects the foveal capillary distribution and leads to a decrease in the SCP FAZ area even there was no structural damage on fundus examination. As a result of our study, the DCP FAZ area after 2 weeks of trauma did not show a statistically significant decrease, but the mean DCP FAZ area decreased. It is thought that additional studies with large patients are needed in the future.
Only in eyes without BOF was there a significant change in size of the SCP FAZ area between initial and follow-up. Some reports have suggested that eyes in blowout injuries are afforded some protection in comparison to eyes in non-blowout injuries [38–40]. Kreidl et al. [41] reported that significant intraocular sequelae, such as retinal detachment, choroidal hemorrhage, and lens dislocation, were higher in mild and moderate ocular trauma without BOF than in severe ocular trauma with BOF and they reported the patients with BOF showed better visual prognosis 1 month after injury compared to patients without BOF. Due to the protective mechanism of orbital fractures, in case of eyes with BOF, it is thought that the FAZ area of SCP did not change after 2 weeks of test compared to the initial test. In case of eyes without BOF, relatively greater damage was absorbed compared to eyes with BOF. As a result, only patients without BOF reduced the FAZ of SCP.
The main limitation of our study was its retrospective nature and cross-sectional design. Also, the lack of further follow-up may obscure the visualization of the changes in FAZ areas during recovery. However, the strength of our study was the relatively sufficient sample size, strictive inclusion criteria and well-planned examination for all patients. Prospective studies with longer follow-up periods are necessary to investigate the role of vascular alterations and FAZ changes in patients with simple BOT who do not have any evident findings on ophthalmic examination.
In conclusion, we demonstrated temporary microvascular ischemia at SCP in patients after BOT. Patients must be warned that transient ischemic changes may occur after trauma. OCTA detects subacute changes in the FAZ at SCP after BOT, even without evident structural damage on fundus examination.
Acknowledgements
None.
Notes
Conflicts of Interest: None.
Funding: This research was supported by the National Research Foundation of Korea (NRF) grant, funded by the Korean government (the Ministry of Science and ICT) (No. 2020R1F1A1072264).